Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1403
Research Article(ISSN: 2644-1403) 
Prize in Charge of the Polytraumatized at the Center Hospitalo-Universitaire Mustapha Pacha in Algiers Volume 2 - Issue 3
Sakhraoui R1*, Habchi N2, Bekralas H2, Bouallag M2, Ziane H3, Maouche H1 and Guerinik M1
- 1Department of Medical and Surgical Emergencies, Mustapha University Hospital, Algiers
- 2Neurosurgery service, Mustapha University Hospital, Algiers
- 3Microbiology department of Mustapha University Hospital, Algiers
Received: November 04, 2019; Published: December 05, 2019
Corresponding author: Sakhraoui R, Department of Medical and Surgical Emergencies, Mustapha University Hospital, Algiers
DOI: 10.32474/GJAPM.2019.02.000137
Abstract
Introduction: A polytraumatized patient is a victim of violent trauma.
Objective: to evaluate the management of polytrauma patients after describing their epidemiologic characteristics and to individualize the predictive factors of mortality.
Materials and Methods: This is a prospective and descriptive study on the observations of 147 polytrauma patients admitted to the medical and surgical emergency department of the University Hospital Center Mustapha Pacha between June 2011 and June 2013. We have not included in the final examinations of the present, but the half-way to the vital prediction for the clinical, biologic, therapeutic and epidemiological aspects of each patient admitted for polytrauma.
Results: 147 cases of polytrauma were collected: 23 women and 124 men. The average age is 38.46±2.93 years. The voices of puberty were the most common cause of trauma 69.38% The average duration of hospitality east of 14.25days±2.56 days. The average rate of care is 9.57±15.09 hours. 44.88% of our patients had 2 associated lesions. The average clinical GCS is 10.80±0.69. Respiratory distress dominates the clinical picture at admission (63.94%), consciousness disorders are observed in 80 patients (54.42%), The anisocoria was observed in 10 patients (6.80%). The thoracic lesions are predominant in our series, found in 63.26% of cases. 54.42% of polytrauma patients had head trauma associated with 18 cases (22.5%) of HED, 16 cases of HSD (20%) and cerebral edema was found in 29 cases (19.72%). The abdominal lesions were discovered in 30.61% of the cases. 57 of our patients died (38.77%). The predictive factor for mortality was: a respiratory distress syndrome (P<0.038), GCS low(P=2×10-6), the presence of anisocoria (P<0.018), inhalatory pneumonitis (P<0.01), low hemoglobin (P<10-4), and low hematocrit (P<10- 4), hypoprothrombopenia (P<10-4), use of controlled ventilation (P<0.001) and vasopressor drugs (P<0.001). Blood transfusion was needed in 35.37%, controlled ventilation in 47.61% of cases and vasopressor drugs in 16.32% of cases. Ninety-two patients (62.58%) required an urgent surgical intervention. Neurosurgical procedures involved 26 patients (17.68%). The laparotomy was indispensable in 23 patients (15.64%).
Conclusion: The decoration of the predictive polytraumatic based on urgent care and efficacy at the scene of the accident, for which the need for a real pre-hospital medicine, and the must be taken care of in the whole of the technical plateau needed and honed to this exercise is difficult.
Keywords: Kinetics; golden hour; evolutivity of lesions; mortality; sequelae.
Introduction
Anyone with at least one life-threatening or functional lesion, or whose mechanism or violence of the trauma suggests that such lesions may exist, is currently defined as a serious traumatic event [1]. Epidemiological studies estimate that there is approximately one severe trauma for ten hospitalized trauma patients and 100 patients presenting to the emergency department [2]. Road trauma remains the leading cause of polytrauma. Traumatic pathology has worsened with the importance and variety of means of transport. In Algeria, the 1st quarter of 2007 experienced 8933 accidents, with 861 dead and 12518 injured [3].
Multiple trauma is the leading cause of death in patients under the age of 35, and a significant source of suffering for both victims and their loved ones. In half of the cases deaths occur at the accident site, 30% within 12 hours after admission and 20% in the following days or weeks [2]. The causes of death for severe injuries vary by study. However, 5 main causes are found: head trauma is the main cause of death (41 to 50%), hemorrhage comes second (13 to 39%), then polytrauma (3 to 25%), medical causes (7 to 22%), finally the medullary traumatisms (4 to 8%) [2]. In Algeria, accidents on public roads are responsible for 4500 deaths a year. A study on polytrauma in the surgical emergency department of Dr Benbadis University Hospital in Constantine in 1999, showed a hospital mortality rate of 52, 35% [4].
The management of multiple trauma patients imposes a real strategy for determining vital emergencies and establishing a complete lesion report. Jean François Murat explains that “more than a full head, better knowledge and a clearly systematized and effective organization. The ability to plan for action remains the dynamic foundation for mastering the management of polytrauma patients “[5].The considerable number of complications related to the polytraumatized or even death that we face daily, led us to reflect deeply on our way of working to identify the shortcomings and failures in the management of these polytraumatized. The objective of our study is to evaluate the management of the polytraumatized at the University Hospital of Mustapha Alger, to search for the risk factors of excess mortality. To develop a multi-trauma care strategy at the UMC service level of Mustapha University Hospital in Algiers.
Patients and Method
This was a longitudinal descriptive and analytical study with prospective data collection over a period of two (02) years from June 1, 2011 to June 1, 2013. It was conducted at the level of the department of medical-surgical emergencies and resuscitation of the Mustapha University Hospital Center in Algiers. Our service of UMC is located of the Mustapha University Hospital which is the biggest hospital of the capital of Algeria. Our emergency service is the largest service nationwide, with 46 hospital beds. Not having enough resuscitation services, our patients stay in the emergency room for the rest of their stay in the hospital. Given the availability of a radiology department at the emergency department level (near the decompression room), 99% of patients had benefited from a radiological lesion report. The study population consisted of polytrauma patients admitted directly or referred from another health structure.
Inclusion criteria: Patients with two or more traumatic lesions, at least one of which is life-threatening in the short or medium term,
Exclusion Criteria: Polytrauma patients who died on admission were not included in this study.
Data collection
Data collection was done prospectively
The variables studied were:
a. Socio-demographic data (frequency, age, sex and profession of
patients)
b. Admission mode
c. Means of transport
d. Cause of the trauma
e. Clinical status at admission (vital distress, anatomical regions
reached, scores and severity indices), Four scores and severity
indices were used to assess the severity of the clinical condition
of patients at admission: Revised Trauma Score (RTS), Glasgow
Coma Score (SCG), Injury Severity Score (ISS) and Simplified
Gravity Index II (IGS II).
f. Para-clinical data (biological and radiological examinations)
i. Biological tests: Groupage, FNS, blood crase (TP, TCA,
fibrinogen), biochemistry
ii. Radiological examinations:
• The chest and pelvic radio and the abdominal ultrasound are
systematic at the level of the salvage room.
• The whole-body CT is required in all hemodynamically stable
patients
• Other examinations such as aortography, echocardiography is
requested according to clinical suspicions
g. Therapeutics, evolutionary and prognostic data.
Data Analysis
The collected data has been processed with Epi info software version 3.5.1. The tables were compiled with the Excel 2007 software. The quantitative variables were expressed on average with a standard deviation. Qualitative variables were expressed by simple count and percentages. The comparison of proportions and percentages was performed with the Chi2 test or the Fisher exact test as appropriate, p≤0.05 was considered statistically significant.
Results
Epidemiological data: Comprehensive study
During the study period, 5784 patients were admitted to the emergency department, of which 2829 were traumatized, i.e. 48.9% of the cases. Among them, 147 polytrauma patients were identified, that is to say 5.19% of traumatized patients and 2.54% of all admissions. 84.35% of the polytraumatized were male and 15.64% female. The sex ratio (M/F) was 5.39. The average age of patients in our series was 38.46±2.93 years with extremes of 9 and 98 years. The age group of 20 to 40 years accounted for 74% of the study population.
Circumstances of the accident
Road traffic accidents were the most common cause: 69.38% of cases (39.21% of all patients were pedestrians), 23.12% suffered a fall and 5.44% physical aggression (willful knocks and wounds). Natural disasters (landslide and falling tree trunks on the body) were noted in 1.36% of cases.
Access channels, arrival times, transport methods
In our study, 42.18% of patients came directly from the accident site and 57.82% were referred from a health center after first aid. The average time taken between the occurrence of the trauma and admission to the emergency department is 3.76±0.13 hours. Medical transport was provided for 11.56% of patients.
State on arrival
48.97% of patients had cardiac distress, 54.42% neurological distress and 63.94% respiratory distress. 44.88% of our patients had 2 associated lesions, 38.77% had 3 associated lesions, 12.24% had 4 associated lesions, 3.40% had 5 associated lesions and 0.68% had 6 associated lesions. 58.50% of patients had head trauma, 19.72% had spinal trauma (cervical spine in 34.48%), the incidence of thoracic traumas was 63.26%, abdominal lesions were found in 36, 05% patients. Renal and urological trauma accounted for 8.16% of patients. The incidence of limb trauma is 68.02% (12% pelvic trauma). The average Glasgow score was 10.80±2.4 with extremes of 3 and 15 (18.36% had a GSC of less than 8). The average ISS was 31.2±6.4 with extremes of 19 and 50. Mean IGS II was 22.6±8.2 with extremes of 12 and 61.
Biological data
The biological assessment was systematic; the average platelet count was 126214.28±58072.14 elts /mm3 [10000-300000 parts/ mm3]. Thrombocytopenia less than 140,000 / mm3 was found in 25.85% of patients (4.76% had a rate of less than 50,000/mm3). The mean prothrombin rate was 57.28±21.99%, with limits ranging from 20% to 92%, and less than 50% in 16.32% of patients. The average hemoglobin level was 8.68±2.49g/l with limits ranging from 4 to 13.5g/l. Leukocytosis was observed in 46.25% of cases, with an average white blood cell count of 10005.71±4119.69 with limits ranging from 4000 to 21000. The average urea level was 0.36 g / l±0.15 with limits ranging from 0.6 to 5.8 g/l and creatinine of 10.9±4.06 mg/l with limits ranging from 5-33 mg/l. The Troponin Ic assay was performed in only 22% of patients, despite the high incidence of thoracic trauma in our series and was greater than 0.01 in 18% of these patients.
Imaging
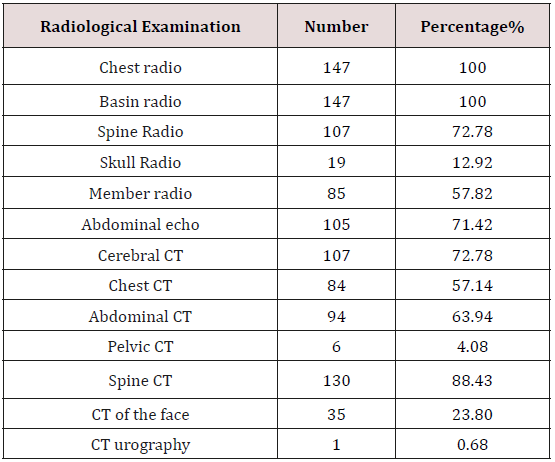
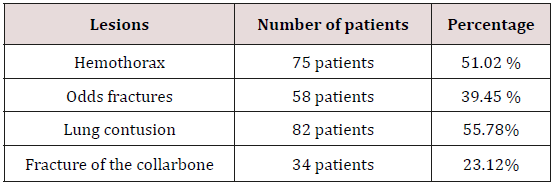
The hierarchy of complementary examinations was dictated by the therapeutic urgency of life-threatening lesions. The emergency examinations in the crush chamber were dominated by the search for a visceral lesion: chest X-ray, abdominal ultrasound, radiograph of the pelvis. Other para-clinical examinations (CT of the skull, thorax, spine, abdomen and pelvis) or other more specialized radiological examinations were performed according to clinical data. 53% of the patients had a whole-body scan. Table 1 illustrates the various radiological examinations performed in our patients as well as their frequencies. Chest X-ray revealed bone fractures such as rib fractures and ribs in 39.45% of cases. The fracture of the clavicle was noted in 23.12% of cases. 51.02% of patients had hemothorax and 55.78% had pulmonary contusion Table 2.
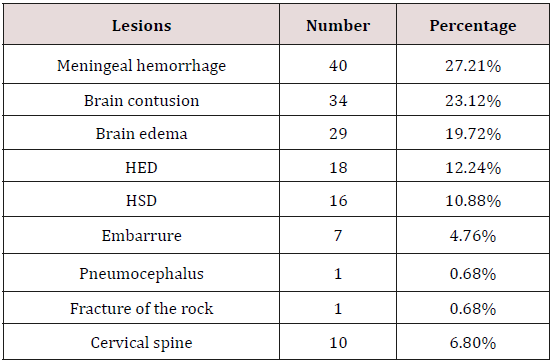
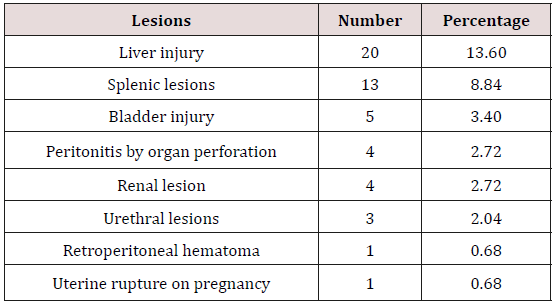
72.78% of the patients had received a brain and cervical scan on admission. This CT was redone during hospitalization if it was performed before the 3rd hour or in case of aggravation. In our series, 58.50% of polytrauma patients had head trauma associated with 18 cases 12.24% HED, 16 cases of HSD (10.88% and cerebral edema in 29 cases (19.72%). The study of cranio-encephalic and cervical anatomical lesions is listed in Table 3. 71.42% of patients had abdominal ultrasound and 63.94% had abdominal computed tomography. Ultrasonography and abdominal CT were the main radiological methods in our series, which made it possible to explore the different abdominal lesions found in 53 patients (36.05%) Table 4.
Renal and urological trauma in our series concerned 12 patients (8,16%). Renal lesions were detected in 4 patients or 2.72% and urological lesions, which were mainly represented by the involvement of the urethra and bladder, were reported in 8 patients 5.44%. Radiography of the pelvis was systematic (100% of patients) before the bladder survey. On the other hand, x-rays of the limbs were requested according to the clinical examination. The incidence of limb trauma is 68.02% (100 patients). These traumatisms were mainly represented by fractures in 73 patients, i.e. 49.65% whereas limb wounds were present in only 15 cases, i.e. 10.20%. The trauma of the pelvis was less frequent in our series and was present only in 12 patients or 8.16%.
Therapeutic data
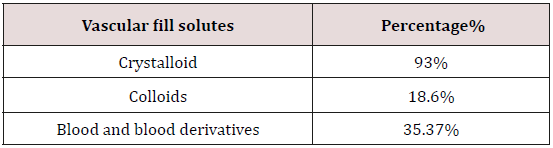
No patients received pre-hospital care during the study period. In the hospital, care included the treatment of various vital distress, the achievement of the lesional balance sheet and surgical procedures. In emergency, a conditioning was carried out and included a peripheral or central venous approach depending on the case, the establishment of a bladder catheter after removal of a pelvic fracture and a nasogastric tube. The management of cardio-circulatory distress was provided urgently by vascular filling with crystalloids in 93.5%, with blood and blood derivatives in 35.37% of cases and with colloids in 18.6% of cases Table 5. The effectiveness of the filling is judged on the improvement of the arterial pressure and the resumption of the diuresis. Patients requiring blood derivatives received in average 3±2 packed red blood cells; 7±5 units of fresh frozen plasma and 5±3 of platelet pellets. The use of vasoactive drugs was necessary in 24 patients (16.32%), generally after failure of the filling to improve the hemodynamic state especially when there was hemorrhage or traumatic brain injury: 87.5% of cases that had received vasoactive amines had an adverse evolution. Upper airway release and oxygen therapy were performed in all patients and 47.61% were intubated and artificially ventilated within the first 24 hours of hospitalization Table 6.
The indication for mechanical ventilation was neurological failure in 48.57% of cases, respiratory distress in 38.57% of cases or hemodynamic failure in 12.85% of cases. The ventilatory parameters were regulated in such a way as to have O2 saturation SaO2>90%. 32.85% of ventilated patients had a favorable evolution. In patients with cranial impact who had a GCS<8: neuro-sedation was required within the first 48 hours and used the combination of Midazolam (1 to 5mg/h) and Fentanyl (5-25g)/h), if persistence of signs of intracranial hypertension and convulsive state, the use of thiopental was necessary at the dose of (3mg/Kg/h). However, those who had 9 <GCS<14 had all received symptomatic treatment of HTIC. The prescription of anticonvulsants was routine in all patients with severe head trauma or in the case of brain injury documented on CT. The drugs used to prevent or treat seizures were CLONAZEPAM (RIVOTRILR), VALPROIC ACID (DEPAKINER), CARBAMAZEPINE (TEGRETOLR) or PHENOBARBITAL (GARDENALR). The latter was the most used in the service.
Analgesia was our major concern at the admission of our patients in that it allowed the comfort of the patient with reduction of the general metabolism and thus decrease of oxygen consumption. It was ensured by opioids in 77% of cases either in a fractional or continuous way with the self-pushing syringe. The use of opioids was limited in cases of severe thoracic injuries outside ventilatory support. Paracetamol for injection was used in all patients in combination with morphine or sometimes antiinflammatory drugs. Antibiotic prophylaxis was systematic in patients admitted to hemorrhagic shock, which corresponds to 48.97%, during emergency surgical procedures, or in the case of open fractures (10.20%) Cefazolin (cefacidal ®)) is the most used. Antibiotic therapy was administered in 26 patients with inhalation pneumonitis at admission, i.e. 17.68% (cefotaxime+metronidazole combination). The prevention of tetanus was systematically ensured by antitetanus serum (TAT) followed by tetanus toxoid (TT) vaccine.
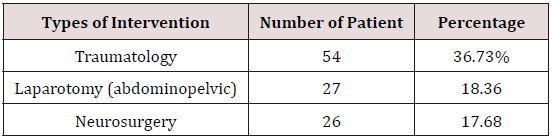
Prevention of thromboembolic disease was physical and medicinal. The compression stockings were mainly used in three situations in our context: head trauma, existence of a haemorrhagic risk (contusion, hematoma, haemothorax ...) and disorders of the blood crase. Elsewhere was prophylaxis with low molecular weight heparin (LMWH). 51.02% of our patients benefited postoperatively from prophylaxis of thromboembolic disease by LMWH. 19% of patients were placed on LMWH 24h after admission (after assessment of the lesion and elimination of a contraindication). In 29.8% of our patients, prophylaxis for thromboembolic disease was physical. Low molecular weight heparin was continued until the patient was discharged from resuscitation. The mean duration of LMWH treatment was 14.25 days±2.56 days. Specific treatment according to the lesional diagnosis was undertaken in intensive care before transfer to the operating room at admission, 34.69% of the patients required pleural drainage and one patient required a tracheotomy for cervical lesions post-injury (tracheal section at the cervical level). 72.78% of patients required urgent surgery:- The neurosurgical interventions concerned 26 patients or 17.68%, it was essentially an evacuation of an Extra-Dural Hematoma (HED) in 6 patients (23.07%); the other neurosurgical interventions had interested HSD (19,23%) dural hematomas and the embarrassment in 11,53% of the cases; The decompressive component was performed in 4 patients (15.38%), the setting up of a PIC in 15.38% of patients and 3 interventions on the cervical spine (11.53%).
Laparotomy was essential in 23 patients (15.64%): 8
exploratory laparotomies (34.78%), the liver is approached in
8.69%, 5 patients underwent splenectomy which corresponds to
21.73%, 4 perforations of a hollow organ (17.39%), 2 diaphragmatic
fractures (8.69%), uterine rupture on 6 months of pregnancy and
retro-peritoneal hematoma (3.34%) had all benefited from urgent
surgery.- Urological surgery involved 4 patients (2.72%).
- No thoracotomy of haemostasis was performed.
-In our series, 54 patients (36.73%) had benefited from
a traumatological intervention of which 27.77% of cases are
represented by wounds and open fractures.
Evolutionary and prognostic data
The mean duration of hospitalization in intensive care was 14.25 days ±2.56 days with extremes ranging from 1 day to 120 days. The evolution was favorable in 61.9% of the cases, the patients had joined their home either directly after their exit of resuscitation or after a stay in a re-education service. 38.1% of the polytraumatized died. During their hospitalization, some patients had complications following trauma, therapeutic measures or long hospitalization: 46.93% had a nosocomial infection (urinary [13.4%], ventilated pneumopathy [85, 5%], postoperative wall infection [1.44%], 39.45% had pressure ulcers, 17.68% had inhaled, 2.72% had had a fatty embolism, 1 had had thrombophlebitis and 1 had other fatal acute renal failure. The causes of death were intracranial hypertension (36.84%), acute respiratory distress syndrome ARDS (28.07%), hemorrhagic shock (12.28%), nosocomial infection (10.0%), 52%), multi-visceral failures (8.77%), fat embolism (1.75%) and acute renal failure (1.75%). In the 90 survivors and saw that most of our patients after leaving the service were lost sight of, in the long run. We could detect that early sequelae (at the end of the service) in 45 patients. These sequelae were represented by functional impotence (14.28%), headache (7.48%), epilepsy (4.76%), pressure ulcers (2.72%) and frontal syndrome (0.68%).) and aphasia (0.68%). Our work allowed us to identify several prognostic factors (clinical, biological, radiological and therapeutic) that are summarized in Table 7.
Discussion
In our study, the frequency of polytrauma patients in ICU was
17.95%. This rate is lower than those reported by Sima et al in
Libreville, Gabon and Gao et al, China, respectively at 34.8% and 65%
[6,7]. These frequencies, constantly high, reflect the place occupied
by the polytraumatized in the activities of a unit of resuscitation.
Polytrauma is a pathology of the young subject between 20 and 30
years of age. This frequency is explained by the demographic age
curve on the one hand, and by the activity of young subjects, which
increases the risk of polytrauma [8, 9]. In Algeria this is justified
by the young age of our population. In fact, 36.73% of the study
population was between 10 and 30 years old and 112 (76.19%)
were under the age of 50.
In industrialized countries where the population is aging,
polytrauma is more and more common in the elderly [10-12].
According to a 1998 study in the province of MARRAKECH, 85.5%
of the seriously traumatized are under the age of 50, as is a similar
study in Casablanca, which noted an age of patients ranging from 16
to 50 years [13,14]. A study done in 1999 in Constantine in Algeria
by Professor O. Boudehane found an average age of 38.8 years [15].
Although polytrauma mainly affects the young subject, in our series
the average age was 38.46±2.93, it did not come out as a prognostic
factor, possibly because of the young age of our patients they in the
groups of survivors or in the group of the deceased.
Male predominance has been reported by all authors. This is
explained by the prevalence of risk activities in humans [12,16].
The difference is less marked in the industrialized countries
where there is a growing involvement of women in all areas of
work, leisure and sport [17,18]. This difference tends to disappear
with age [11,12]. The predominance of the male sex is confirmed
in our study with 84.35% of men and 15.64% of women without
influencing mortality, thus joining the other series of studies. A great
variability of the trauma circumstances is noted in the different
epidemiological studies according to the sociological, economic and
demographic characteristics of the populations. Road accidents are
the most important cause of polytrauma [19].
In our series, road accidents account for 69.38% of polytrauma
cases. For the American system: the pre-hospital care of emergencies
is based on the major principle of the speed of transport to the
hospital. It is provided by non-medical ambulances. Emergency care
is started by the paramedical team. Coordination and regulation
are provided by control centers. The intervention of the ambulance
network is done according to a precise territorial division which
allows very short intervention times [20,21]. For emergencies in
France, there is a pre-hospital care medicalized. The task of the
doctor is to maintain the vital functions, to diagnose and stabilize
the lesions, and to prepare the reception in the most appropriate
department [22,23].
In Algeria, the transport of casualties is mainly by non-medical
ambulances of the civil protection. There is no coordination or
liaison with the reception centers. In our series only 17 patients
benefited from a medical transport. The delay in management
reflects the organization of the medical system and influences
the vital prognosis of the traumatized [24,25]. An American study
reports that the time to care for the traumatized is less than one
hour [20].In our series 58.50% of patients have a management
time of less than 4 hours and 41.5% are supported after the 4th
hour with impact on mortality.19.04% of patients admitted directly
to Mustapha CHU had a management time of less than one hour.
Clinical examination of the polytraumatized is difficult. Many
consider that clinical examination has little value for the diagnosis
of hemoperitoneum [26].
On the other hand, a summary clinical examination is useful by
focusing on the neurological examination, the auscultation of the
thorax, the search of the distal pulses, the examination of the bone
in particular of the thorax, the rachis, the pelvis, and the limbs, and
the pelvic touches. Initial clinical examination, although difficult
and sometimes uninformative due to impaired consciousness, is of
major importance. It allows to suspect, before any sedation, serious
lesions of difficult diagnosis and to direct the patient towards a
suitable center. These lesions are spinal fractures and sprains,
pelvic fractures, abdominal hollow organ fractures, and cerebral
and medullary neurological lesions. The clinical examination of
the polytraumatized must be rapid and complete. For this, it is
necessary to adopt a systematic clinical approach that will be
even faster than it is pre-established, executed and recorded
automatically [27]. Nearly 30% of post-traumatic deaths can be
prevented according to a large study carried out in Great Britain in
1988 [28]. These preventable deaths are linked in 70% of the cases,
the non-recognition or the insufficient treatment of a hypoxemia or
a hypovolemia [19, 28].
The origin of respiratory distress may be related to alveolar
hypoventilation with multiple causes. The central origin may be
related to the depth of coma and repeated convulsive seizures or to
high spinal cord injury. The peripheral origin reflects an alteration
of ventilatory mechanics during thoracic traumas (flaps), during
heavy pneumothorax or haemothorax. It may be a disorder of
alveolar-capillary diffusion in the context of a pulmonary contusion
or an inhalation pneumopathy [29]. The multiplicity of etiologies of
respiratory distress explains early death in the absence of rescue
procedures [30,31]. In our study the main causes of distress were
respiratory (63.94%), neurological (54.42%) and hemodynamic
(48.97). Respiratory distress is a predictor of mortality (P<0.025).
In the initial phase, arterial hypotension refers to hypovolemia
of externalized, retroperitoneal hemorrhagic origin or multi-focal
diaphyseal fractures (femur) and / or endothoracic compression
of the heart chambers in most cases.30 to 40% of these patients
die from haemorrhagic shock and its consequences, patients
with a systolic blood pressure lower than 90mmHg when treated
at the scene have a mortality of more than 50% [32,33]. In our
study, both systolic and diastolic blood pressure were predictive
of excess mortality. Most authors emphasize the seriousness of the
association of hypotension with head trauma. Neurological distress
is defined by a deep coma (GCS<8), or a coma with a localization
sign, or secondary installation coma [34,35]. Cervico-medullary
injuries also constitute distress situations with the risk of secondary
aggravation [36,37].
Severe head trauma is the most common association, it greatly
modifies the prognosis. Thirty percent of patients with head injury
on admission die from direct consequences of brain damage [29]. In
our series 58.50% of patients had 31.39% associated head trauma
to deep coma (GSC<8). A GSC<8 and the presence of anisocoria
increased the risk of death in our patients. For the evaluation of
gravity, the ISS has been able to evaluate the lesional severity on
a scale from 1 to 75 [19,38]. He cannot predict the favorable or
unfavorable evolution of a patient but has made it possible to locate
each individual in a group whose mortality rate is known. The
average ISS in our series is 29.7. The Glasgow coma scale estimate
is decisive for the choice of therapeutic behavior [19,24,36]. The
mean GCS in our study is 10.80±0.69 [3-15]. In our study, there is a
significant difference in the mortality rate according to the average
values of the GCS (p=2x10-6). The latter thus constitutes a risk factor.
Conclusion
Polytrauma is common and affects many young adults between the ages of 16 and 35 with male predominance in our hospital. It is mainly due to road accidents. Improving pre-hospital care by boosting the activities of civil protection and the UAS, equipment and better organization of emergency and resuscitation units as well as the application of care protocols, will help to improve their vital and functional prognosis.
References
- Riou B, Vivien B, Langeron O (2006) Which priorities in the initial care of the polytraumatisé? Conferences of update 217-227.
- Tentillier E, Masson F (2000) Epidemiology of trauma-in severe trauma. In: Beydon L, Carli P, Riou B (Eds.), Severe trauma, Arnette, Paris, France, p. 1-15.
- First United Nations World Road Safety Week 23-29 April 2007, Geneva, Switzerland.
- Boudehane O (1999) Evaluation of the severity and strategy of the PEC of the polytraumatised at the surgical emergencies of the Constantine University. These of DESM 205.
- Murat JE, Huten N (1995) The polytraumatized. Encycl. Med Chir Emergencies 24-101-D p.16.
- Sima ZA, Benamar B, Ngaka D, Mbini J, Nzoghe J (1998) Traumatic pathology and resuscitation in African environment: experience of the hospital center of Libreville. Medicine of Black Africa 45: 535-37.
- Gao JM, Gao YH, Zeng JB, Wang JB, He P, et al. (2006) Polytrauma with thoracic lesions and/or abdominal experience in 1540 cases. Chin J trauma 9: 108-14.
- Houssin B, Claire G Ravary H (1994) Socioprofessional reintegration of polytrauma patients without cranioencephalic or medullary lesion Anesth 42(4): 467-469.
- Mahe V, Jamali S, Himri N, Dounas M, Ecoffey C (1997) Severity score in surgical resuscitation RéanUrg 6(1): 65-66
- Broos Plo (1992) Diagnosis procedures in abdominal trauma. J Emergencies 5: 134-143.
- Sztark F, Hazera S, Masson F, Thicoipe M, Lassiep D (1995) The serious trauma of the elderly: specificities and prognostic factors. Ann Fr Anesth Réanim 14: R 355.
- Vander SCK, Klasen HJ, Eisma WH, Ten Duis HJ (1996) Major trauma in young and old: what is the difference J trauma 40(1): 78-81.
- El Houdzi J (1995) Support for cranial trauma at the ibn tofail hospital in MARRAKECH. Thesis Med Casablanca, 1988, No. 110 14-KHALIFI L Closed chest trauma. Thesis Med, Casablanca pp. 182.
- Carli P (1997) Conduct to be held prehospital in front of a polytraumatized person following a road accident. JEUR 1: 33-7.
- Boudehane O (1999) Evaluation of the severity and strategy of the PEC of the polytraumatised at the surgical emergencies of the Constantine University. France.
- Bode PJ, Edwards MJR, Kruit MC, VanVugt AB (1999) 1671 patients with blunt abdominal trauma. AJR 172(4): 905-911.
- Eberhard LW, Morabito DJ, Matthay MA, Mackersie RC, Campbell AR, et al. (2000) Initial severity of metabolic acidosis predicts the development of acute lung injury in severely traumatized patients. Crit Care Med 28(1): 125-31.
- Rose JS, Levitt MA, Porter J, Hutson A, Greenholtz J, et al. (2001) Does the presence of ultrasound really affect the computed tomographic scan use? A prospective randomized trial of ultrasound in trauma. J Trauma 51(3): 545-550.
- Carli P, Riou B (1992) Trauma of the thorax. Ann Fr Anesth Reanim 43: 611-626.
- Ankel F, Roenigsberg M (1992) Prehospital Care in Chicago, European Emergency 5(4): 235-242.
- Harvey S, Levin PH, Francois Aldrich E (1992) Severe head injury in children: Data Bank Neurosurgery 31(3): 435-444.
- Bleichner G, Mane PH, Desboudard (1990) Investigation of the operation of reception and emergency services of 260 hospitals. Med Urg Intensive Care 6(1): 31-37.
- Calon B, Launoy A, Ocquidant PH, Mahopudeau G, Gengen WINN, et al. (1994) Polytrauma and the elderly. Cah Anesth 42(4): 535-537.
- Telasne B, Tulasne P, Kempf IA (1988) Polytraumatized. Encyc Med Chir, 14033A 10: 15.
- Ilef D, Isnard H, Capek I, Junod B (1993) Evaluation for the response to a serious emergency: the analysis of the delay of care. Rev SAMU 6: 311-316.
- Parmentier G, Katz A, Fermanian J, Chalaux G (1983) The abdomen of the polytraumatized. Comparative study of 225 polytrauma patients with and without abdominal lesions. Incidence of abdominal complications. J Chir 120(2): 85-93.
- The polytraumatized manual of anesthesia, resuscitation and emergency Elsevier Masson II (edn), 2002.
- Qmoeschler (1997) Initial pre-hospital care of the polytraumatized. Med and Gyg 55:1848-1854.
- Polytraumatise: news in the pre-hospital phase Ph. Dabadie, Sztark F, Thicoïpé M, ME Small Jean. Department of Emergencies, Department of Anesthesia Resuscitation Pr. Erny, Hospital Group Pellegrin, 33076 Bordeaux, France.
- Scalea TM, Rodriguez A, Chiu WC, Brenneman FD, Fallon WF, et al. (1999) Focused assessment with sonography for trauma: results from an international consensus conference. J Trauma 46(3): 466-472.
- Shackford SR, Rogers FB, Osler TM, Trabulsy ME, Clauss DW, et al. (1999) Focused abdominal sonogram for trauma: the learning curve of nonradiologist clinicians in detecting hemoperitoneum. J Trauma 46(4): 553-564.
- Edouard A, Mimoz O (1997) Hemodynamic aspects of the polytraumatized. Conferences of update 1997. French Society of Anesthesia and Resuscitation. Paris, Elsevier, pp. 445-463.
- Sauaia A, Moore FA, Moore EE, Haenel JB, Read RA et al. (1994) Early predictors of multiple organ failure postinjury. Arch Surg 129(1): 39-45.
- Martin C, Domergue R (1997) Prehospital and early hospital management of a traumatic hemorrhagic shock state. Ann Fr AnesthRerm 16(8): 1030-1036.
- Bickell WH, Wall MJ, Pepe PE, Martin RR, Ginger VF, et al. (1994) Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med 331(17): 1105-1109.
- Carli P (1997) Conduct to be held prehospital in front of a polytraumatized person following a road accident. JEUR 1: 33-37.
- Spaite DW, Criss AE, Valenzuela TD, Meislin HW (1998) Prehospital Advanced Life Support for Major Trauma: Critical Need for Clinical Trials. Ann Emerg Med 32(4): 480-489.
- Moreau M, Gainer PS, Champion H, Sacco WJ (1985) Application of the trauma score in the prehospital setting. Ann Emerg Med 14(11): 1049-1054.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...