Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1403
Case Report(ISSN: 2644-1403) 
Novel Use of Superficial Cervical Plexus Nerve Block and PECS I Block in Paediatric Patients for Vagal Nerve Stimulator Implant Surgery – A Case Series Volume 2 - Issue 4
Melody H Long1* and Tracy YS Tan2
- 1Department of Paediatric Anaesthesia, KK Women’s and Children’s Hospital, Singapore
- 2Department of Paediatric Anaesthesia, KK Women’s and Children’s Hospital, Singapore
Received: January 06, 2019; Published: January 16, 2020
Corresponding author: Melody H Long, Department of Paediatric Anaesthesia, KK Women’s and Children’s Hospital, Singapore 100 Bukit Timah Rd 229899, Singapore
DOI: 10.32474/GJAPM.2020.02.000143
Introduction
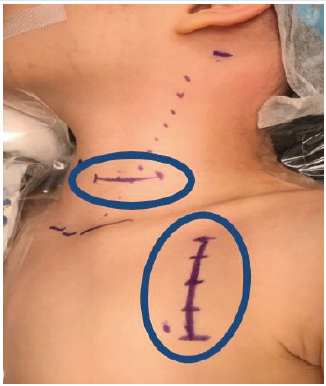
Pectoralis Nerve (PECS) block was first described as an alternative to thoracic epidural and paravertebral blocks in managing pain after breast surgery [1]. Since then, there have been modifications such as the PECS II block and expansion of its uses to include analgesia for Port-a-Cath insertion and removal [2], minimally invasive cardiac surgery [3] and cardiac resynchronization therapy (CRT) device implantation [4]. Superficial cervical plexus blocks have been described to be effective for analgesia preceding procedures in the head and neck region. These procedures include carotid endarterectomy, thyroidectomy, and even part of a combination of peripheral nerve blocks for shoulder surgery [5]. A vagal nerve stimulator implantation surgery is often offered to patients with refractory epilepsy as a last line of therapy to control seizures despite being on multiple anti-epileptic drugs. The surgery will involve incisions at both the lateral neck and pectoral region (Figure 1).
As such, we postulate that a combination of the superficial cervical plexus block and PECS 1 block will be effective in managing peri-operative pain for a vagal nerve stimulator implant. We believe this combination of blocks is especially useful for this patient population as the refractory seizures may have caused a certain degree of developmental delay-impairing the children’s ability to give accurate feedback about wound pain, therefore hindering pain assessment and the institution of appropriate analgesic management after surgery.
Case Report
We look at the following 2 cases where a combination of a superficial cervical plexus nerve block and PECS 1 block was performed for perioperative pain management for a vagal nerve stimulator implant surgery. Parental consents for case discussions and the use of photographs/images have been obtained for this publication.
Case 1
Figure 2: Left Superficial Cervical Plexus Block SCM: Sternocleidomastoid ASM: Anterior Scalene Muscle MSM: Middle Scalene Muscle.

A 5-year-old girl, 17.5kg with a history of refractory infantile epilepsy, presented for an elective vagal nerve stimulator implant surgery. Despite being on multiple anti-epileptic drugs, she had up to 20 episodes of seizures per day. She is non-verbal and communicates discomfort by pointing or making incomprehensible noises. Patient was induced with IV Propofol 60mg, Fentanyl 30mcg and Atracurium 8mg. She was intubated with a size 5 cuffed endotracheal tube using a McGRATHTM video-laryngoscope. A 22G intra-arterial cannula was inserted for haemodynamic monitoring. After intubation, the left superficial cervical plexus block (Figure 2) and PECS I block (Figure 3) were performed aseptically using an inplane approach with a PAJUNK® 50mm needle under ultrasound (SonoSite, M-Turbo®) guidance. Levobupivacaine 0.25% 2mls and 8mls (0.46ml/kg) were given respectively for the superficial cervical plexus and PECS I block after negative aspiration for blood.
IV Paracetamol 250mg (15mg/kg) and IV Fentanyl 40mcg (2.3mcg/kg – including 30mcg given at induction) were administered intraoperatively. At the conclusion of an uneventful surgery, neuromuscular blockade was reversed with Atropine 0.3mg and Neostigmine 0.8mg. The child was extubated deep after the airway was cleared of secretions. She was monitored in the Post Anaesthesia Care Unit (PACU) for immediate post-operative complications. She remained comfortable during recovery and did not show any signs of discomfort over the operation sites. She was discharged to the high dependency unit and prescribed regular Paracetamol and Ibuprofen. Her FLACC pain scale was 0 both after surgery and on Post-Operative Day (POD) 1 with oral Paracetamol. She was discharged well on POD 2.
Case 2
An 8 year–old boy, 23 kg, with a history of asthma and tuberous sclerosis complex consisting of cardiac rhabdomyoma, renal angiolipoma, harmatoma and refractory epilepsy, presents for elective vagal nerve stimulator surgery. Despite being on four antiepileptic drugs and ketogenic diet, he was still having refractory seizures. He is developmentally delayed but is able to verbalize pain. He was induced with IV Propofol 60mg, Fentanyl 25mcg and Atracurium 10mg. He was intubated with a size 5.5 cuffed endotracheal tube using a Karl Storz C-MAC® video-laryngoscope. A 22G intra-arterial line was inserted for hemodynamic monitoring. After intubation, left superficial cervical plexus block and PECS 1 block were performed aseptically under ultrasound (SonoSite, M-Turbo®) guidance with a PAJUNK® 50mm needle using Levobupivacaine 0.25% 2mls and 6 mls (0.3mls/kg) respectively.
The surgical incisions were similar to that described in the first case. Intra-operatively, IV Paracetamol 360mg (15mg/kg) and a total of IV Fentanyl 37.5mcg (1.6mcg/kg –including 25mcg given at induction) were administered. He was reversed with Atropine and Neostigmine and extubated awake. His pain score on the Numerical Rating Scale (NRS) was 0 in the PACU and he was able to play with his toy dinosaurs. He was discharged to the general ward with oral Paracetamol and Ibuprofen. He remained well in the general ward with NRS 0 on POD 1. He only required regular Paracetamol for analgesia post-operatively.
Discussion
At present, superficial cervical plexus nerve blocks and PECS 1 blocks are performed in isolation in scattered types of surgeries amongst children. By extrapolating from current knowledge of the areas which will be anaesthetized from the two blocks, we postulate that the combination of the blocks will be effective in covering pain from the incisions for a vagal nerve stimulator implant. From the two cases discussed, we see how the combination of blocks was effective in reducing peri-operative opioid usage and is a safe means of providing analgesia. In addition, they also provide long lasting pain relief up to 24 hours. These blocks are relatively easy to perform and do not add significantly to the total duration for anaesthesia induction. Caregivers are also satisfied with the quality of perioperative pain relief that these blocks have accorded. Moving forward, perhaps, it will be useful to compare the analgesic effectiveness of the combination of these blocks with only local anaesthesia infiltration at the wound alone to see if it is worth the extra effort to perform the blocks.
Conclusion
We believe our institution is the first to describe the combination of superficial cervical plexus block and PECS 1 block in providing peri-operative analgesia for vagal nerve stimulator implant surgery in paediatric patients. This has shown to be a safe and effective means of providing analgesia; and is a good adjunct to existing simple analgesics such as Paracetamol and NSAIDs.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
The authors have no sources of funding to declare for this manuscript.
References
- Blanco R (2011) The ‘pecs block’: a novel technique for providing analgesia after breast surgery. Anaesthesia 66(9): 847-848.
- Munshey F, Ramamurthi RJ, Tsui B (2018) Early experience with PECS 1 block for Port-a-Cath insertion or removal in children at a single institution. Journal of Clinical Anesthesia Volume 49: 63-64.
- Yalamuri S, Klinger R, Bullock W, Glower DD, Bottiger BA, et al. (2017) Pectoral fascial (PECS) I and II blocks as rescue analgesia in a patient undergoing minimally invasive cardiac surgery. Reg Anesth Pain Med 42: 764-766.
- Fujiwara A, Komasawa N, Minami T (2014) Pectoral nerves (PECS) and intercostal nerve block for cardiac resynchronization therapy device implantation. Springer Plus 3: 409.
- Musso D, Flohr MS, Meknas K, Wilsgaard T, Ytrebø LM, et al. (2017) A novel combination of peripheral nerve blocks for arthroscopic shoulder surgery. Acta Anaesthesiol Scand 61(9): 1192-1202.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...