
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1403
Case Report(ISSN: 2644-1403) 
Late Diagnosis In Netherton Syndrome in Adult: A Case Report Volume 1 - Issue 5
Oyamada LH, Militão LM, Pozetti M, Adami A, Sá APM, Coimbra RTLA, Lages TSFA, Rodrigues TAOV, Amorim MFM3 and Monson CA*
- Departament Dermatologia, Faculdade de Ciências Médicas IPEMED and UNIFESP, Brazil
Received:June 09, 2019; Published: June 17, 2019
Corresponding author:Monson CA, Departament Dermatologia, Faculdade de Ciências Médicas IPEMED, UNIFESP, São Paulo, Brazil
DOI: 10.32474/GJAPM.2019.01.000122
Abstract
This is a case report at the Dermatology Service of the Institute of Research and Medical Education (IPEMED, São Paulo Campus), a patient with suspected Netherton syndrome (NS), male, aged 40, who did not dermatological disease throughout childhood and even in adult life. Prior use of sporadic topical steroid alone, with temporary improvement of the cutaneous condition. After discussion about the challenges for the diagnosis of this syndrome, the patient underwent appropriate treatment, starting Retinoid orally, which resulted in a satisfactory clinical outcome after one month of starting therapy.
Keywords: Netherton; Erythroderma; Ichthyosis; Tricoscopy
Background
The Netherton Syndrome (NS) consists of a rare, autosomal recessive genodermatosis with defective production or retention of the stratum corneum, which belongs to the group of ichthyoses. It is associated with a genetic defect, described in the SPINK 5 gene, located on chromosome 5q31-32, which encodes a serum protease inhibitor, LEKT 1, expressed on skin and lymphoid tissue. This mutation results in alteration of keratinization, increasing the proteolytic activity of the skin, leading to premature peeling and skin barrier impairment. As a result, disorders and alterations of hair and skin, such as circumflex linear ichthyosis, eczematous rash, diffuse erythema, atopic diathesis and specific hair shaft alteration - called invaginated tricorrexis or bamboo hair - may also occur, with intellectual disability . Its early diagnosis is critical in the neonatal period, since the disease can be even more severe and fatal, since it presents, more frequently, serious complications due to hypernatremic dehydration, important weight loss, hypothermia, respiratory infection and sepsis. Therefore, other diseases, such as primary immunodeficiency syndrome, lamellar ichthyosis, erythrodermic psoriasis, congenital ichthyosiform erythroderma or seborrheic dermatitis should always be excluded. Its diagnosis can be confirmed through skin biopsy, electron microscopy and immunohistochemical study, however, because it requires careful evaluation, it tends to be late confirmed. Currently there is no known cure or specific treatment satisfactory for such a syndrome. However, treatment modalities, such as topical calcineurin inhibitors, topical retinoids, narrowband ultraviolet B phototherapy, psoralen and ultraviolet irradiation and oral acitretin have been used with variable success. In people with severe disease, intravenous immunoglobulin and anti-TNF-α are new therapeutic options.
Case Report
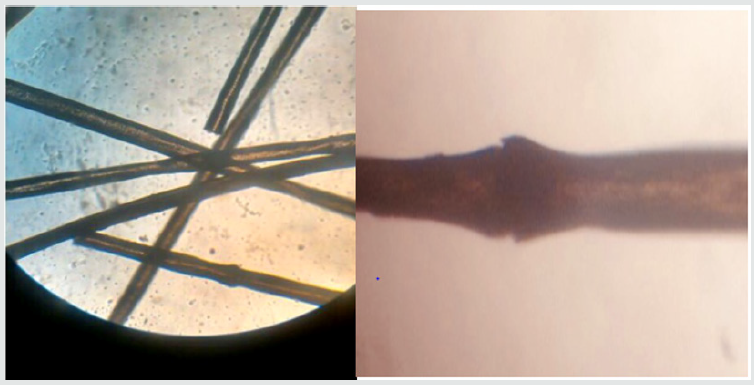
We declare that all the precepts of Bioethics were fulfilled in the present case report, including with the signature by the patient of Term of Free and Informed Consent. Male patient, born in Barreiras - BA, 40 years old, with a history of skin eruption from birth, complained of “fine and brittle hair”, scaling in the body, diffuse erythema of the skin, accompanied by pruritus, with temporary improvement when treated with topical corticosteroids and various antimicrobials. Dermatological examination revealed desquamative areas and diffuse erythema on the trunk, with serpiginous squamous plaques, as well as annular lesions and erythematous plaques on hands (Figures1 & 2). She had thin, opaque, rarefied and thin hair and eyebrows (Figure 3). Examination of the capillary rods under optical microscopy (100x) revealed tricorrexe invaginata (Figure 4). The histopathological picture was non-specific, with moderate epidermis and regularly thickened by acanthosis and elongation of the interpapillary ridges, hypergranulosis with stratum corneum replaced by parakeratosis, sometimes continuous. In the papillary dermis, dilation of the blood and lymphatic vessels with mild perivascular lymphocytic infiltrate was observed. Dermis reticular and hypodermic unchanged. It may, however, correspond to the Netherton syndrome (NS). In view of such findings, the diagnosis of (NS) was closed, and Acitretin 25mg daily was instituted in a single dose, and an important improvement was observed in a period of one month, and there was also a report of decreased pruritus and erythema . It was also reported a subsequent growth of eyebrows and hair. Clinical and laboratory evidence indicates that Acitretin, because it is derived from vitamin A and belongs to the retinoid group, shows a satisfactory action when applied in keratinization disorders. It is therefore frequently used in the ichthyoses in general. Thus, the benefits are evident, with a significant reduction in the indexes of desquamation, in the reduction of the scales, and in a greater skin elasticity [1-5].
Figure 1. Erythema diffuse in the trunk; erythematous-serpiginous and polycyclic lesions, with margins presenting double scaling edge.

Figure 2. Annular and serpiginous lesions with eczematous areas; erythematous plaques with circinate scaling on hand fingernails.
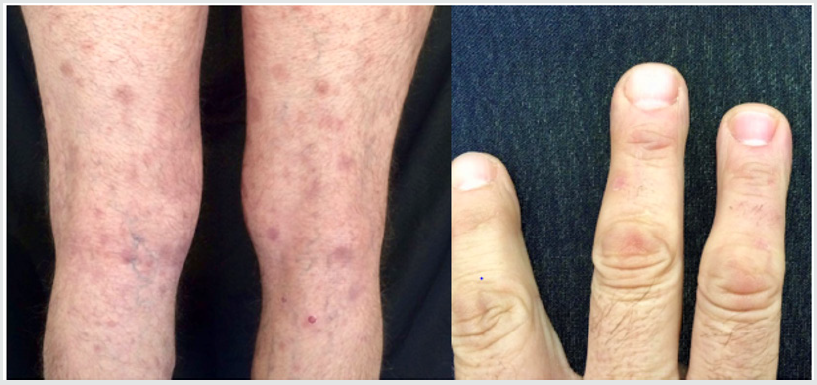
Figure 4. Microscopic examination of the hair demonstrating a typical bamboo alteration, characterizing the invaginated tricorrexe (in increase of 100x).
Discussion
(NS) is a dermatological disorder characterized by atopic manifestations, congenital ichthyosiform erythroderma, usually having its first appearance in the neonatal period, with erythroderma and/or hypotrichosis. There are also reports of characteristic capillary abnormalities, which are considered pathognomonic of the Syndrome, and are called “ tricorrexe invaginated “ (TI). (TI) consists of changes that occur due to a transient defect in hair keratinization due to an incomplete conversion of sulfhydryl to sulphide bridges in the cortical region, so the internal root sheath is keratinized, but the hair shaft does not, resulting in a fragility in the cortical region of the hair with invagination of the distal part on the proximal of the stem (striking zigzag pattern), which is described as brittle hair and hair (bamboo hair), and can be observed under light microscopy. Atopic signs and areas of peeling, usually polycyclic and migratory are seen, and may still manifest intellectual deficiency in some cases. The transmission of the defect is autosomal recessive due to a genetic defect associated with the mutation of the SPINK 5 gene, located on chromosome 5q31-32, responsible for encoding a serum protease inhibitor, LEKT 1, present in the epidermis and lymphoid tissue, being, its expressiveness, variable. The dysfunction of this inhibitor, or even the absence thereof, alters cell differentiation, thus justifying the association of the atopic condition and the keratinization disorder, since the abnormal expression of the inhibitor influences the differentiation of T cells, leading to the Th2 immune response, thus evidencing high levels of IgE and immunological fragility, corroborating with atopic manifestations, both cutaneous and alimentary or, still, respiratory. Differential diagnosis is therefore challenging, mainly because there are no typical cutaneous signs of the syndrome, and the same changes can be seen in many other erythrodermae. Concomitant atopy may also lead to misdiagnosis of atopic dermatitis and severe eczema. On the other hand, the pillar alterations, although pathognomonic, are not always visualized in a first sampling, therefore, they may require numerous analyzes, since they are not present in all the filaments, making the diagnosis even more difficult, which with high frequency is confirmed after several months and even years after the start of follow-up. Thus, complementary examinations may help in the establishment of differential and conclusive diagnosis, especially with skin biopsy, as well as electron microscopy, since this examination evidences “invaginated tricorrexe”, which elucidates the striking zigzag pattern characteristic. On the other hand, the histopathological examination shows non-specific psoriasiform changes, with parakeratosis and acanthosis, which are of little value in the diagnosis, but can still be collaborative [6-8].
Because it is a complex disease, with keratinization disorder and frequent complications, especially in the neonatal period, the use of systemic retinoids, such as acitretin, is usually recommended as soon as possible, which represents a greater chance of significant improvements in both the lesions as well as changes in capillaries. Concerning eczematous changes, these may be controlled with corticosteroids, when necessary.
One of the objectives of disclosing the present case report is to illustrate, therefore, the difficulty in performing the diagnosis of (NS) in a 40-year-old adult male without a diagnosis of confirmed skin disease since childhood, and was treated occasionally with steroids, but did not present clinically significant improvement responses. In the present case, the diagnosis, although late, was confirmed by electron microscopy and corroborated by histopathology. Of note, improvement in signs and symptoms was observed 1 month after initiation of oral Acitretin treatment [9-11].
Final Considerations
Clinical findings of (SN) tend to be inconclusive, since not all hair filaments present (TI) and cutaneous presentations are variable, which contributes to the fact that the diagnosis of the disease in the present case has been challenging and obscure for a long time, which happens, in most cases, late, usually after many tests, and at different times, which causes the patient to have poor quality of life. Thus, it is strongly recommended that health professionals provide the diagnostic hypothesis of (SN) in cases of erythroderma and associated capillary complaints without response to previous treatments and non-conclusive skin diagnoses, and perform thorough trichoscopy in suspected cases, whether in the and the avoidance of indiscriminate and unnecessary use of corticosteroids and steroids in the long term, thus improving quality of life, as well as increasing the expectation of life of these patients.
References
- Singer R, Çopur M, Yuksel EN, Kocaturk E, et al. (2015) Ichthyosis linearis circumflexa in a child. Response to narrowband UVB theraphy. J Dermatol Case Rep 4: 110-112.
- Roda A, Mendonça-Sanches M, Travassos AR, Soares-de-Almeida L, Metze D (2017) Infliximab therapy for Netherton Syndrome: A case report. JAAD Case Reports 3(6): 550-552.
- Bittencurt MJS, Moure ERD, Pies OTD, Mendes AD, Depra MM, et al. (2015) Tricoscopy as a diagnostic tool in trichorrhexis invaginata and Netherton syndrome. An Bras Dermatol 90(1): 114-116.
- Zhvania P, Hoyle NS, Nadareishvii L, Nizharadze D, Kutateladze M (2017) Phage therapy in 16-year-old boy with Netherton syndrome. Frontiers in Medicine 4(94): 1-5.
- Duquia RP, Souza PRM, Almeida HL, Vettorato G (2006) Síndrome de Netherton com 20 anos de acompanhamento. An Bras Dermatol 81(4): 563-566.
- Sun JD, Linden KG (2006) Netherton syndrome: A case report and review of the literature. International Journal of Dermatology 45: 693-697.
- Rudnicka L, Olszewska M, Rakowska A, Slowinska M (2011) Trichoscopy update 2011. J Dermatol Case Rep 4: 82-88.
- Boskabadi H, Maamouri G, Mafinejad S (2013) Netherton Syndrome: A case report na review a literature. Iran J Pediatr 23(5): 611-612.
- Leung AKL, Barankin B, Leong KF (2018) An 8-year-old child with delayed diagnosis of Netherton Syndrome. Case Reports in Pediatrics.
- Sarri CA, Roussaki Schulze A, Vasilopoulos Y (2017) Netherton Syndrome: A Genotype-Phenotype Review. Molecular Diagnosis and Therapy 21: 137-152.
- Goujon E, Beer F, Fraitag S, Hovnanian A, Vabres P (2010) ‘Matchstick’ eyebrow hairs: a dermoscopic clue to the diagnosis of Netherton syndrome. European of Academy of Dermatology and Venerology 24: 737-743.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





