Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1403
Case Report(ISSN: 2644-1403) 
Iatrogenic Alcohol Inhalation Inducing Coronary Spasm and Sinus Tachycardia in Asthmatic and Liver Cirrhotic Patient; Oxygen Reversal: A Case Report Volume 4 - Issue 1
Yasser Mohammed Hassanain Elsayed*
- Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Egypt
Received:December 17, 2020; Published: January 08, 2021
Corresponding author: Yasser Mohammed Hassanain Elsayed, Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt
DOI: 10.32474/GJAPM.2020.04.000179
Abstract
Rationale: Iatrogenic substance-inducing disease is an occasionally clinical entity. Alcohol is a common illicit and abused substance. Inhaling alcohol vapor and mists have common occupational health and safety risks including both respiratory and hepatic hazards. Patient concerns: An elderly-aged married male patient presented to the physician’s outpatient clinic with tachypnea, sinus tachycardia, and chest pain post-alcohol inhalation. Diagnosis: Iatrogenic alcohol inhalation inducing sinus tachycardia and coronary spasm in an asthmatic and cirrhotic patient. Interventions: Electrocardiography, oxygenation, monitoring for vital signs, and echocardiography. Outcomes: The dramatic normalization of clinical and electrocardiographic coronary artery spasm with sinus tachycardia after oxygenation had happened. Lessons: The identification of substance-induced disease is a pivotal step in diagnostic decision making of medical disorders. Alcohol inhalation can be inducing coronary artery spasm and sinus tachycardia. Alcohol-inducing coronary artery spasm and sinus tachycardia can be reversed by oxygenation. Hypoxia is a suggested theory in pathogenesis.
Keywords: Iatrogenic alcohol inhalation; induced coronary artery spasm; sinus tachycardia; asthma; cirrhosis; oxygen reversal
Abbreviations: CAS: Coronary Artery Spasm; ECG: Electrocardiogram; GCS: Glasgow Coma Scale; IHD: Ischemic Heart Disease; NSR: Normal Sinus Rhythm; O2: Oxygen; POC: Physician Outpatient Clinic; VR: Ventricular Rate
Introduction
Alcohol inhalation is a direct method of giving alcohol into the respiratory system using a steaming or nebulizing apparatus [1]. Occupational health and safety risks are common hazards due to inhaling alcohol vapor and mists. Coronary artery spasm (CAS) is occasionally accompanied by abused substances e.g., alcohol [2,3]. Ethanol is a well-known inducer for concentration-dependent CAS [4,5]. The mechanism of alcohol inducing CAS is still inconclusive [2]. Sinus tachycardia is a normal, physiological, reactive, and response process rather than a characteristic arrhythmia. It is augmented by catecholamine release [6,7]. It is a leading finding for the etiology [7]. A several recognizable causes has been implicated for sinus tachycardia, such as hypoxia, hyperthyroidism, fever, acute pulmonary embolism, acute myocardial infarction, sepsis, severe anemia, congestive heart failure, pain, anxiety, dehydration, betaantagonist withdrawal, and vasopressors [6,7]. Sinus tachycardia will resolve with resolution of this inciting process [7].
The Alcohol can be monitored by changes in plasma levels of prostanoids such as thromboxane, 6-keto prostaglandin F1 alpha, catecholamines, serotonin, cyclic nucleotides such as cyclic adenosine monophosphate-cAMP, cyclic guanosine monophosphate-cGMP, and platelet aggregation post-alcohol [2]. Inhalation devices are ultimately an easy way to overdose on alcohol than drinking. Indeed, alcohol possesses the first-pass metabolism in the stomach and liver with direct going into the bloodstream. Unfortunately, inhaled alcohol cannot be removed from the body by vomiting. Inhaled alcohol can dry out nasal passages that will be increasing the risk of infection [8]. The connection between alcohol and asthma is well-known in the opinion of many researchers. The studies demonstrated that alcohol worsens the symptoms causing full-blown asthmatic episodes. Histamines and sulfites are two components in various types of that are implicated, the hazardous culprit. Histamines are produced from bacteria and yeast when alcohol ferments. Histamines are a well-known allergen. This is particularly actual for asthmatic patients. Sulfites is an inducer for allergic reaction if there is hypersensitivity to them. Approximately10 % of asthmatic patients are sensitive to these additives. This sensitivity can yield several asthmatic symptoms. Some patients may be complaining of wheezing, but others may have an asthma attack [8]
Aim of This Study: In this manuscript, I reported the development of sinus tachycardia with significant ST-segment depressions within 30 minutes of alcohol inhalation that mistakenly using alcohol instead of sterile water in the water cup of the O2 cylinder.
Case Presentation
A 67-year-old married, farmer, male, Egyptian patient presented in the physician outpatient clinic (POC) with tachypnea, dizziness, and chest pain. Profuse sweating and acute confusion state were the associated symptoms. The patient relatives gave an old history of bronchial asthma and liver cirrhosis. They give a recent asthmatic episode 3 days ago. He was acutely managed by the other POC. The POC only prescribed humified oxygen (O2) as needed. Within 30 minutes of presentation, the patient gave a recent history of O2 inhalation mistakenly using alcohol instead of sterile water in the water cup of the O2 cylinder. Otherwise, oxygen, there were no prescribed drugs in the past. The patient denied any history of other cardiac, thyroid, or other relevant diseases. Upon examination, the patient appeared tachypnic, pale, sweaty, and confused. Her vital signs were as follows: blood pressure of 110/70 mmHg, the pulse rate of 120/bpm; and regular, the respiratory rate of 34/min, the temperature of 36.6°C, the pulse oximeter of oxygen (O2) saturation of 89%, GCS of 12, and tachycardia on heart auscultation. No more relevant clinical data were noted during the clinical examination. Emergency call for an ambulance to transport the patient to the nearest central hospital. The patient was temporarily managed and monitored for the vitals and O2 saturation. ECG tracing was done 3 days before the current presentation showing normal sinus rhythm (NSR) with VR; 62 bpm (Figure 1A). Serial ECG tracings were done. The initial ECG tracing was done on the alcohol toxicity presentation showing sinus tachycardia with significant STsegment depressions in both inferior (II, III, and aVF) and anterior leads (V1-6) with VR; 102 bpm. (Figure 1B). Oxygen inhalation (5 L/min) with an O2 generator was given. The patient had gradually become calm with clear improvement in the respiratory status. The second ECG tracing was taken within 30 minutes of O2 inhalation and 42 minutes of B.
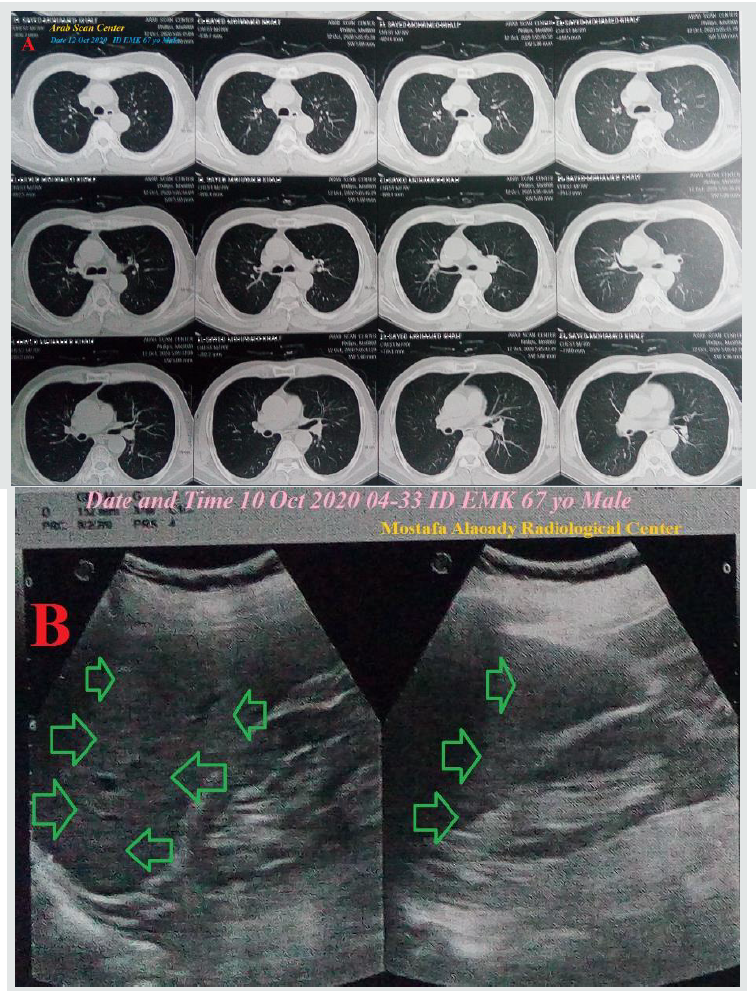
ECG tracing showing sinus tachycardia with decreased the magnitude of above ST-segment depressions and the number of affected leads in inferior (II and aVF) and anterior leads (V4 and V5) with VR; 118 bpm. There was a Wavy triple sign of hypocalcemia (Yasser sign) in I, III, aVL, and V1-3 leads (Figure 1C). The third ECG tracing was taken within 80 minutes of O2 inhalation showing NSR with VR of 60 beats/min and the disappearance of above STsegment depressions and Wavy triple sign. (Figure 1D). Workup; Complete blood count (CBC); Hb was 13.2 g/dl, RBCs; 4.81*103/ mm3, WBCs; 15.56*103/mm3 (Neutrophils; 73.5 %, Lymphocytes: 23.5%, Monocytes; 2, and Eosinophils; 1), Platelets; 235*103/mm3. Measured random blood sugar was normal; 70 mg/dl. S. Ferritin was normal; 196 ng/ml. D-dimer was normal; 200 ng/ml. The initial CRP was high; 6 g/dl. SGPT was normal; 40.2 U/L, SGOT was normal; 36 U/L, LDH was normal; 232 U/L, Serum creatinine; 1 mg/dl and blood urea were normal; 24.8 mg/dl. Plasma sodium was normal (139 mmol/L). Serum potassium was normal (4.6 mmol/L). Serum calcium showing hypocalcemia with ionized calcium; 0.84 mmol/L. The troponin test was negative (less than 2 ng/ L). Chest CT was done within 3 days post-presentation showing no abnormality detected (Figure 2A). Abdominal ultrasound was done within 24 hours of the presentation showing severe liver cirrhosis (Figure 2B). Later echocardiography showed no detected abnormalities with EF 61%. The dramatic response of the above ST-segment depressions and sinus tachycardia to O2 inhalation occurred. The patient was gone home within 2 hours after clinical relief and electrocardiographic normalization. On arrival of the ambulance, the patient was going to recovery. So, the patient refuses the referral and request to complete his treatment at home. Oral diltiazem, oral calcium, and vitamin-D preparation were added drugs when going. Future cardiologist, and pulmonologist, and toxicologist consultation was advised.
Figure 1: Serial ECG tracings A. ECG tracing was done 3 days before the current presentation showing NSR with VR; 62 bpm. There are missed V6 lead (blue arrows) with AC technical artifacts (golden arrows). B. ECG tracing; The initial emergency ECG tracing was done on presentation showing sinus tachycardia with significant ST-segment depressions in both inferior (lime arrows; II, III, and aVF) and anterior leads (blue arrows; V1-6) with VR; 102 bpm. C. ECG tracing was done within 30 minutes of oxygen inhalation and 42 minutes of B. ECG tracing showing sinus tachycardia with slight ST-segment depressions in both inferior (lime arrows; II and aVF) and anterior leads (blue arrows; V4 and V5) with VR; 118 bpm. There is Wavy triple sign of hypocalcemia (Yasser sign) in I, III, aVL, and V1-3 leads. Blue arrows indicate a depressing beat, green arrows indicate an isoelectric beat, and red arrows indicate an elevated beat. D. ECG tracing was done within 80 minutes of oxygen inhalation showing NSR with VR of 60 beats/min and the disappearance of above ST-segment depressions and Wavy triple sign.
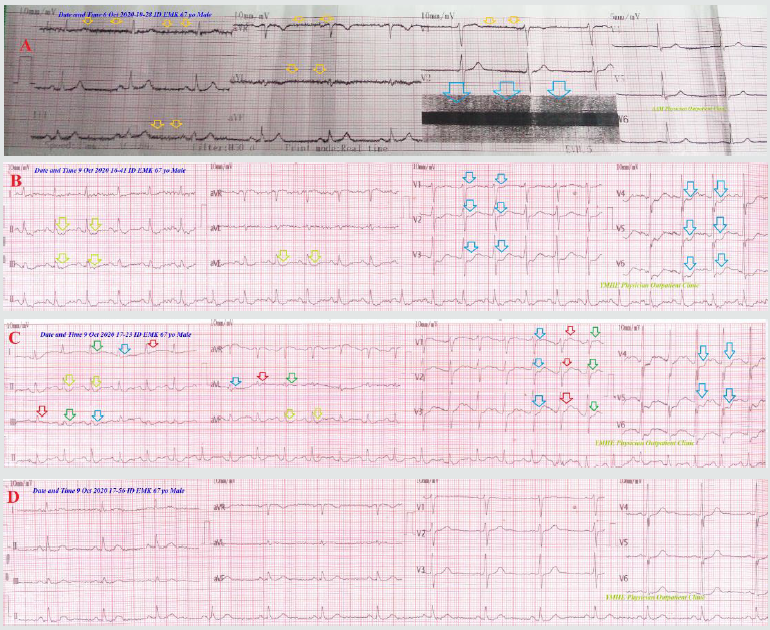
Figure 2: A. image- Chest CT was done within 3 days post-presentation showing no abnormality detected. B. image-Abdominal ultrasound showing severe liver cirrhosis (green arrows).
Discussion
Overview: A 67-year-old married male patient presented to the physician’s outpatient clinic with tachypnea, sinus tachycardia, and chest pain.
The primary objective: for my case study was the presence of tachypnea, sinus tachycardia, and chest pain post-iatrogenic alcohol inhalation.
The secondary objective: for the case study was How would you manage iatrogenic alcohol inhalation inducing sinus tachycardia and coronary spasm in an asthmatic and cirrhotic patient?
The dramatic normalization of electrocardiographic coronary artery spasm and sinus tachycardia after oxygenation had happened.
a. The identification of substance-induced disease is a pivotal step in diagnostic decision making of medical disorders.
b. Alcohol-inducing coronary artery spasm and sinus tachycardia were reversed by oxygenation.
c. The elevated CRP, presence of leukocytosis, and neutrophilia can be interpreted as associated acute inflammatory indices.
Indeed: the mechanism of alcohol-inducing coronary artery spasm and sinus tachycardia is unknown. Hypoxia is a suggested theory in pathogenesis.
a. The author thinks that liver cirrhosis and bronchial asthma may be trigger factors.
\b. The negative troponin test with non-conclusive ECG changes for ischemic heart disease (IHD), and normal echocardiography will quietly exclude the presence of IHD.
c. Despite the drug-drug interactions (DDIs) or even drug-food interactions have a strong impact in inducing various serious drug adverse effects, but it was unavailable in my case report. Absent of using drug combinations in the patient history may exclude the theory of drug-drug interactions.
d. Finally, I reported the development of sinus tachycardia and coronary spasm within 30 minutes of iatrogenic alcohol inhalation in a 67-year-old asthmatic and cirrhotic male patient.
e. The main differential diagnoses for the study case are acute pulmonary edema, acute pulmonary embolism, and IHD.
Limitations of the Study
a. There are no known limitations in the study.
b. This is the first case that reports these adverse drug reactions with inhaled alcohol. So, I can’t compare this case with another case because there was no similar publicized case report.
Recommendation
a. It is recommended to widening the research in clearing the simultaneous presence of coronary artery spasm and sinus tachycardia with alcohol inhalation.
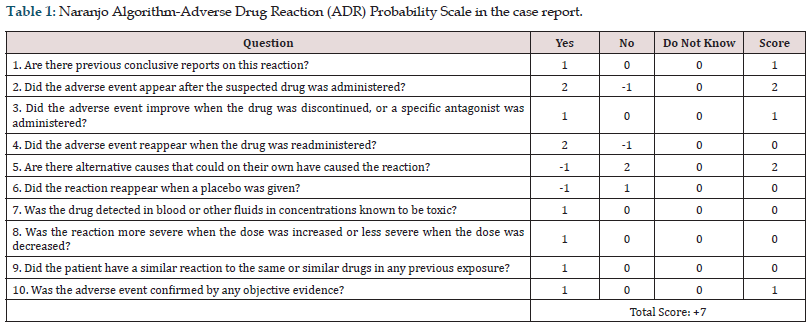
b. After the exclusion of other possible triggers in the current case, the Naranjo probability scale was used to evaluates the association between alcohol inhalation and the development of coronary artery spasm and sinus tachycardia. Naranjo probability scale in the current case study was +7. It is meaning that there was a probable relationship between these adverse reactions and the causing agent, alcohol (Table 1).
c. Substance-induced diseases is a pivotal step in the diagnosis decision making of any medical problems.
d. Substance adverse effects are a occasionally strong way for the diagnostic challenge in clinical medicine.
Conclusion
a. The dramatic disappearance of coronary artery spasm and sinus tachycardia after oxygenation in the patient using iatrogenic alcohol inhalation is meaning that this CAS and sinus tachycardia was lonely due to alcohol.
b. Alcohol can induce coronary artery spasm and sinus tachycardia.
c. The author thinks that alcohol-inducing coronary artery spasm and sinus tachycardia were reversed by oxygenation without using anti-IHD drugs.
d. Future precautions on using alcohol bottles or containers for safe storage, in general, are the recommendation for the current case study.
Acknowledgment
I wish to thank my wife to save time and improving the conditions for helping me.
Conflicts of Interest
There are no conflicts of interest.
References
- Ratner M, William ME, Jonathan SR (2020) Neurological effects of chronic occupational exposure to alcohol mists and vapors in a machinist. Toxicology Communications 4(1): 43-48.
- Oda H, Suzuki M, Oniki T, Kishi Y, Numano F (1994) Alcohol and coronary spasm. Angiology 45(3): 187-197.
- Menyar AA (2006) Drug-Induced Myocardial Infarction Secondary to Coronary Artery Spasm in Teenagers and Young Adults. J Postgrad Med 52: 51-56.
- Gowda RM, Khan IA, Vasavada BC, Sacchi TJ (2003) Alcohol-triggered acute myocardial infarction. Am J Ther 10(1): 71-72.
- Altura BM, Altura BT, Carella A (1983) Ethanol produces coronary vasospasm: evidence for a direct action of ethanol on vascular muscle. Br J Pharmacol 78: 260-262.
- Maleki M, Alizadehasl A, Haghjoo M (2018) Chapter 13-Tachyarrhythmias Practical Cardiology, (1st Edn), pp. 229-249.
- Asensio JA, Trunkey DD (2008) Chapter 85-the Diagnosis and Management of Cardiac Dysrhythmias. Current Therapy of Trauma and Surgical Critical Care (1st Edn), pp.602-609.
- Michelle C (2013) Inhaling alcohol vapor puts you at risk of overdose. CBS News.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...