Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1403
Research Article(ISSN: 2644-1403) 
Humidified High Flow Nasal Cannula Algorithm for Primary Therapy in Hypercapnic Respiratory Failure Volume 1 - Issue 4
Raquel d’ Espiney, Jacek Jablonski, Michal Brys and Juan F Martin Lazaro*
- Newham University Hospital, London, UK
Received:May 28, 2019; Published: June 13, 2019
Corresponding author:Juan F Martin Lazaro, Newham University Hospital, London, UK
DOI: 10.32474/GJAPM.2019.01.000120
Abstract
Background: Humidified high flow nasal cannula (HFNC) has been shown to be an effective respiratory support therapy in both primary and post-extubation patients with Type 1 respiratory failure (T1RF). Clinical outcomes using HFNC in patients with hypercapnic respiratory failure or Type 2 respiratory failure (T2RF) are less well understood as research to date has frequently excluded hypercapnic patients. However, there is growing evidence that suggests HFNC could be beneficial in patients with T2RF.
Aims: To describe the outcome of patients with T2RF who received primary HFNC and to elaborate a safe algorithm for its use.
Methods: We conducted a retrospective observational study on the use of HFNC as a primary treatment in 102 (n=102) consecutive subjects admitted to the Intensive Care Unit (ICU) from August 2015 to June 2017. Vital signs and arterial blood gases were evaluated before, one hour and 6 hours after initiation HFNC and their need for escalation of therapy was collected from patient records.
Results: In T2RF patients it was observed that HFNC was successful in 51.28%, and despite escalation, 90% of subjects were successfully discharged from hospital. Need for escalation of therapy was observed at 24.56 hours of treatment with HFNC. In our population, in both T1RF and T2RF, those with a pH<7.30 and a RR≥30 prior and one-hour post initiation of HFNC were more likely to require escalation of therapy and, these parameters had 97% specificity and 80% predictive value. Conclusion: HFNC could be cautiously used as primary therapy in hypercapnic respiratory failure. The clinical parameters: pH<7.30 and a RR≥30, prior and post initiation of HFNC, allow a risk stratification of subjects and a safe guide in case of needing an escalation of therapy.
Keywords: Humidified high flow nasal cannula; Respiratory high flow therapy; High flow oxygen therapy; High flow nasal cannula oxygen therapy; Heated humidified high flow therapy; Type 2 respiratory failure
Introduction
The benefit and effectiveness of heated and humidified high-flow nasal cannula (HFNC) in Type 1 respiratory failure (T1RF) patients has been well recognized in literature [1-3]. It allows delivery of heated and humidified oxygen at high flow rates (typically 40–50L/ min) and with accurately predetermined oxygen concentrations. It has been observed that the therapy produces an improvement in physiological parameters (oxygen saturations and respiratory rate) [4] by providing low-level positive airway pressure, reducing physiological dead space and improved patient comfort ultimately, resulting in a reduced work of breathing [5]. The use of HFNC in Type 2 respiratory failure (T2RF) is still under much investigation with limited evidence available supporting its use in: sleep – related hypoventilation [6], hypercapnic respiratory failure [7] and chronic obstructive pulmonary disease (COPD) [8]. This is likely due to clinicians being reluctant to deliver oxygen in a cohort of patients where it can reduce their respiratory drive when exposed to high oxygen concentrations. Emerging data by Hernandez et al. demonstrates the developing use of HFNC in hypercapnic patients during post-extubation and there are increasing case reports demonstrating the successful use of HFNC in the primary treatment of acute hypercapnic respiratory failure [9-11], Airway model reconstructions have shown that HFNC can produce a washout of the carbon dioxide in the anatomical dead space and increase alveolar ventilation [12]. Studies have demonstrated HFNC to be at least non-inferior to NIV with regards to intubation rate, Intensive Care Unit (ICU) mortality and ventilator-free days at day 28 [13]. It also has improved patient tolerance; more relief of dyspnoea and patients are more compliant with treatment [14]. The long-term humidification therapy provided by HFNC statistically significantly reduced days of exacerbation, increases time to first exacerbation, and generally improves lung function and quality of life in subjects with COPD and bronchiectasis [15]. In stable COPD patients when HFNC was compared to long term oxygen therapy, there was a 7.3% reduction in CO2 levels and a 64.9% improvement of end expiratory lung impedance [16].
Aim
Our study aims to describe the outcome of patients with T2RF who received primary HFNC and to elaborate a safe algorithm for its use. Also, to provide further understanding, through physiological parameters and arterial blood gases (ABGs), on the use of HFNC as primary treatment in hypercapnic patients in an Intensive Care Unit (ICU) setting as an emerging alternative treatment option.
Methods
A retrospective observational study was conducted at a district general hospital in an 8-bed adult ICU at Newham University Hospital, London, over a 21-month period. Subjects were consecutively included in the study if they were aged above 18 years old and had received HFNC as a primary treatment during their ICU admission. ICU admission criteria was based on National Early Warning Score 2 (NEWS 2) [17], when this score was >5. Subjects who did not have initial baseline observations and arterial blood gases to allow data comparison were excluded. The decision to provide HFNC was made by the ICU team when there was not a clear indication for immediate intubation. HFNC was delivered by the Fisher & Paykel Healthcare Opti flow system. Therapy was initiated at the previous fraction of inspired oxygen (FiO2 ) delivery system and a flow rate varying between 30-60L, titrating both flow and FiO2 to maintain target percutaneous oxygen saturations (SpO2 ) >94% in T1RF and 88-92% in T2RF. Temperature was set at 37. Clinical parameters (heart rate, respiratory rate, oxygen saturations) and arterial blood gases were obtained from the patient´s ICU observation chart at baseline, 1 hour and 6-hour post treatment initiation, as standard procedure in critical patients. Remaining demographic and comorbidities were obtained from the hospital patient electronic system. During the study period, 102 subjects received HFNC from which there were identified as T2RF by mean partial arterial pressure of carbon dioxyde (PaCO2 ) >6.7kPa (>50mmHg) and bicarbonate >24mmol/l or T1RF when mean partial arterial pressure of oxygen (PaO2 ) was below 8kPa (<60mmHg) with normal or low PaCO2 ,<6.7kPa (<50mmHg) as cut off point. The primary outcomes were whether subjects required escalation of treatment whilst on HFNC (non-invasive ventilation, intubation and palliation) and whether they were successfully discharged from hospital. Secondary outcomes included improvement in physiological parameters and ABGs. Failure of HFNC treatment, due to the lack of a universal standardized algorithm, was determined by the treating clinician based on worsening physiological parameters, gas exchange and failure to tolerate treatment. Primary outcomes were further analyzed against physiological markers and pH to allow risk stratification of features associated with need for escalation of therapy. This allowed a proposed algorithm to be developed to support clinicians identify “alarms signs” prompting early assessment and escalation of therapy if necessary.
The study was approved by the hospital ethic committee and patient consent was waived because data collation occurred retrospectively after patient discharge.
Statistical analysis
Excel software was used for initial data collation and Statistical Package of Social Sciences (SPSS version 20) was used for statistical analysis. Demographic data were expressed as mean±standard deviation and dichotomous variables were reported as number (percentage). Parametric data were analysed through Student T – Test. Non – parametrical tests were used in some subgroups due to the limited number of subjects (n<30) and qualitative data were compared using the Fisher exact test. Friedman test was used for analysis of variance for repeated measures. Assigned rank test P<0.05 was considered statistically significant.
Results
Subject characteristics
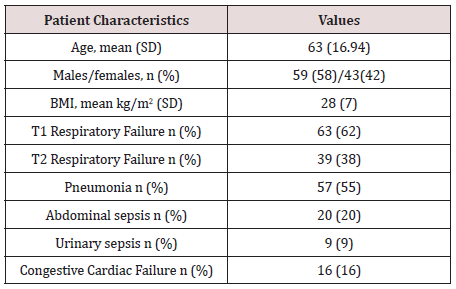
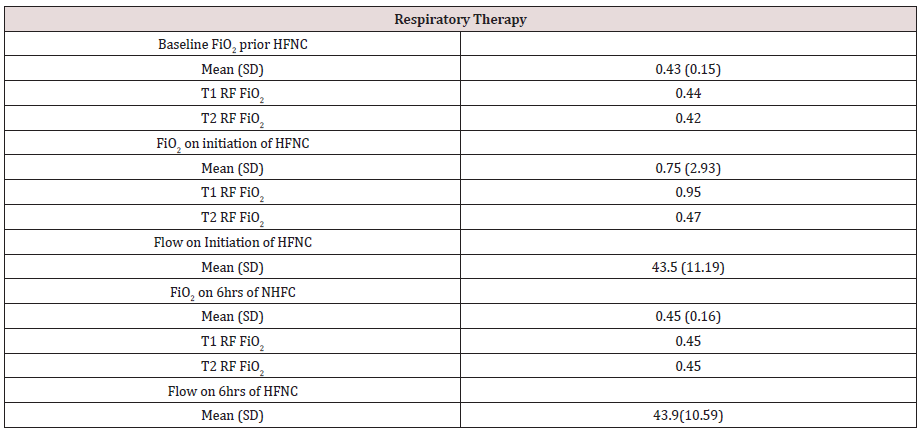
The study included 102 subjects treated with HFNC as primary respiratory support. The mean age of our population was 62 years with a standard deviation (±SD) of (±18 years). In our population, 59 were male (57.84%) and 43 were females (42.16%) with a mean age of 62.41 and 61.60 years respectively. The underlying diagnosis within our population group were; pneumonia, abdominal sepsis, congestive cardiac failure and urinary sepsis. There were 63 subjects identified as having T1RF and 39 subjects with T2RF. The average BMI of our population group was 28kg/m2 . We observed that within our population group the mean FiO2 prior to HFNC was 0.43 and this was delivered via conventional oxygen (nasal prongs or venturi mask). On initiation of HFNC within the Type 1 RF the mean FiO2 was 0.95 and 0.47 for T2 RF with an average flow rate of 43.5L. Within 6 hours of HFNC therapy the FiO2 was titrated down to 0.45 within the Type 1 RF and in T2 RF this was increased to 0.45. Tables 1 & 2 reflect patient demographics and FiO2 and flow settings prior and during HFNC therapy, respectively.
Primary outcomes
In Type 2 RF it was observed that HFNC was successful, without escalation of therapy, in 20 subjects (51.28%) compared to 43 subjects (68.23%) among the T1RF group. In T2 RF treatment was escalated in 19 subjects (48.7%) and it was on average initiated after 24.56 hours of treatment with HFNC whilst T1 RF escalation was required in 20 subjects (31.74%) and initiated on average 15.19 hours post initiation of therapy. Non-invasive ventilation (NIV) was required for 14 subjects (36%), 4 were intubated (10%) and 1 (5%) patient received HFNC therapy for palliation. Despite escalation, 34 subjects (90%) were successfully discharged from hospital.
Secondary outcomes
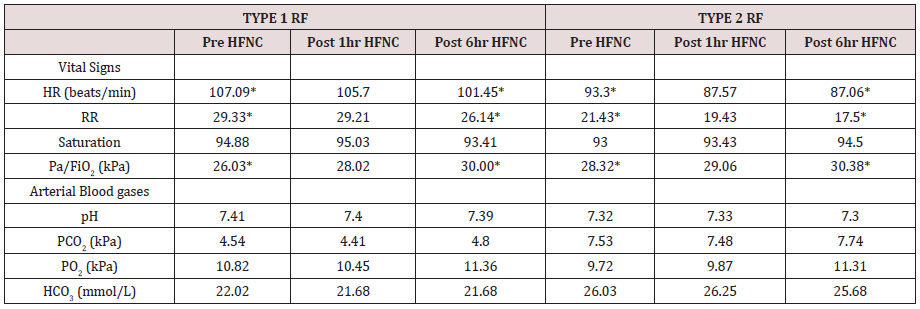
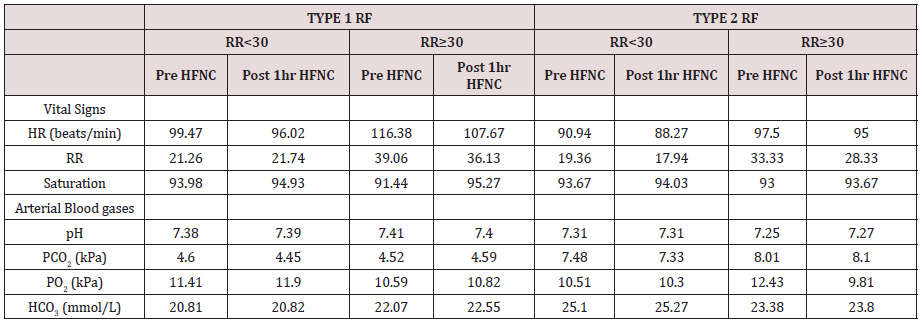
On initiation of HFNC, a statistical difference (p<0.05) was observed for the clinical parameters: HR and RR, as well for physiological lung changes in the Pa/FiO2 across two time points, namely pre and post 6hrs of HFNC as demonstrated in Table 3. We did not observe a statistical significance in the reduction of pCO2 in both groups at pre and 6 hours post HFNC.
(*) Statistically significant difference (p<0.05).
Effect of RR and pH on primary and secondary outcomes
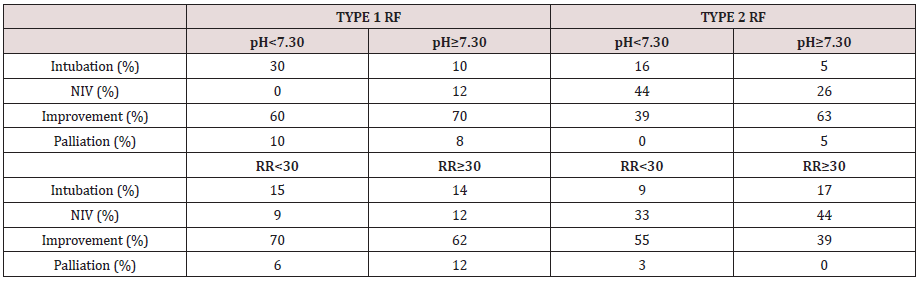
Subjects with a RR≥30 were identified as having reduced likelihood of improvement, namely in T1RF 70% vs 62% and in T2RF 63% vs 39%. In those with a pH<7.30 an increased need for escalation of therapy was observed in both groups, with an increased risk of intubation. HFNC allowed an improvement in most physiological and arterial blood gas parameters in subjects with a pH<7.30 and RR≥30, irrespective of their type of respiratory failure, with exception of T2RF where worsening hypoxia, acidosis and an increase in PaCO2 was observed. Demonstrated in Table 4 & 5. Both parameters combined (RR≥30 and pH<7.30) demonstrated a specificity of 97% and predictive value of 80% for need of escalation.
Discussion
This study adds understanding to the limited evidence and experience of using HFNC in hypercapnic subjects. In our population we observed HFNC could be cautiously used in hypercapnic respiratory failure as primary therapy for respiratory failure with a success of 51.28%. HFNC allowed an improvement in their vital signs and gas exchange by delivery of gas at flow rates exceeding the patient´s peak inspiratory demand, upper airway dead space washout and the ability to generate low levels of positive airway pressure15. We did not observe a statistical significance in the reduction of pCO2 in these subjects and, in the group pH <7.30 and RR≥30, pCO2 increased. This could be explained by FiO2 not being titrated to target saturations which may have resulted in suppressed respiratory drive in this population group. Despite escalation of therapy on HFNC, only 10% were intubated and 90% of subjects were successfully discharged from critical care. With increased pressure and demand for critical care beds and the poor tolerance associated with NIV, the initiation of HFNC on hypercapnic subjects is an attractive alternative therapy to ventilator support and a bridge to stabilizing vital signs until escalation of therapy decisions are made and patient is transferred to critical care. As the use of HFNC becomes increasingly available in facilities outside critical care, clinicians need to be supported in recognizing deteriorating signs and the need for escalation. In our population, in both Type 1 and Type 2 Respiratory failure, those with a pH<7.30 and a RR≥30 prior and one-hour post initiation of HFNC were more likely to require escalation of therapy and these parameters had 97% specificity and 80% predictive value. These parameters allow risk stratification of subjects and propose an algorithm (Figure 1) to be used within the first hour of initiation of HFNC which supports clinicians, particularly those outside critical care settings, in recognizing subjects not thriving on HFNC. Despite our limited sample size in hypercapnic respiratory failure, our retrospective review suggests that HFNC could be cautiously used as primary therapy and allow decision making time for clinicians.
Conclusion
HFNC could be cautiously used as primary therapy in T2RF patients. The clinical parameters: pH<7.30 and a RR≥30, prior and post initiation of HFNC, allow a risk stratification of subjects and a safe guide in case of needing an escalation of therapy.
References
- Maggiore SM, Idone FA, Vaschetto R, Festa R, Cataldo A, et al. (2014) Nasal high flow versus Venturi mask oxygen therapy after Extubation. Effects on oxygenation, comfort, and clinical outcome. Am J Respir Crit Care Med 190: 282-288.
- Corley A, Bull T, Spooner AJ, Barnett AG, Fraser JF (2015) Direct extubation onto high-flow nasal cannulae post-cardiac surgery versus standard treatment in patients with a BMI≥30: a randomised controlled trial. Intensive Care Medicine 41(5): 887-894.
- Parke RL, McGuinness SP, Eccleston ML (2011) A preliminary randomised controlled trial to assess effectiveness of nasal high-flow oxygen in intensive care patients. Respiratory Care 56(3): 265-270.
- Sztrymf B, Messika J, Mayot T, Lenglet H, Dreyfuss D (2012) Impact of high-flow nasal cannula oxygen therapy on intensive care unit patients with acute respiratory failure: a prospective observational study. J Crit Care 27(3): 324.
- Nilius G, Franke KJ, Domanski U, Rühle KH, Kirkness JP, et al. (2013) Effects of nasal insufflation on arterial gas exchange and breathing pattern in patients with chronic obstructive pulmonary disease and hypercapnic respiratory failure. Adv Exp Med Biol 755: 27-34.
- Okuda M, Kashio M, Tanaka N, Matsumoto T, Ishihara (2014) Nasal highflow oxygen therapy system for improving sleep-related hypoventilation in chronic obstructive pulmonary disease: A case report J Med Case Rep 13(8): 341.
- Millar J, Lutton S, O’Connor P (2014) The use of high-flow nasal oxygen therapy in the management of hypercarbic respiratory failure. Ther Adv Respir Dis 8(2): 63-64.
- Bräunlich J, Mauersberger F, Wirtz H (2018) Effectiveness of nasal highflow in hypercapnic COPD patients is flow and leakage dependent. BMC Pulmonary Medicine 18: 14.
- Hernandez G, Vaquero C, Colinas L (2016) High flow conditioned oxygen therapy for prevention of reintubation in critically il patients at high risk for extubation failure: A multicenter randomised controlled trial. JAMA 316: 1565-1574.
- Lepere V, Messika J, La Combe B, Ricard JD (2016) High-flow nasal cannula oxygen supply as treatment in hypercapnic respiratory failure. AJEM 34(9): 175-185.
- Pavlova I, Plamondon P, Delisle S (2017) Nasal high-flow therapy for type II respiratory failure in COPD: A report of four cases. Respiratory Medicine Case Reports.
- Fricke K, Tatkov S, Domanski U, Franke KJ, Nilius G, et al. (2016) Nasal high flow reduces hypercapnia by clearance of anatomical dead space in a COPD patient. Respir Med Case Rep 19: 115-117.
- Frat JP, Thille Aw, Mercat A (2015) Hig-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Eng J Med 372(23): 2185-2196.
- Möller W, Celik G, Feng S (2015) Nasal high flow clears anatomical dead space in upper airway models. J Appl Physiol 118: 1525-1532.
- Rea H, McAuley S, Jayaram L (2010) The clinical utility of long-term humidification therapy in chronic airway disease. Respir Med 104(4): 525-533.
- Fraser JF, Spooner AJ, Dunster KR, Anstey CM, Corley A (2016) Nasal high flow oxygen therapy in patients with COPD reduces respiratory rate and tissue carbon dioxide while increasing tidal and end-expiratory lung volumes: a randomised crossover trial. Thorax 71(8): 759-761.
- (2017) Royal College of Physicians. National Early Warning Score (NEWS) 2. Standardising the assessment of acute illness severity in the NHS. Updated report of a working party. RCP, London, UK, England.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...