
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1403
Case Report(ISSN: 2644-1403) 
Enchondroma - Case Report Volume 1 - Issue 5
João Vicente de Souza Filgueiras1, Maria de Fatima Maklouf Amorim1, Airton Schmitt2, Deivid Donizete Borges1 and Carlos Alberto Monson1*
- 1Ipemed College of Medical Sciences, Specialization Course Dermatology, Brazil
- 2Beneficial Society New Har, Surgeon
Received:July 13, 2019; Published:July 18, 2019
Corresponding author:Carlos Alberto Monson, Ipemed College of Medical Sciences, Specialization Course Dermatology, Brazi
DOI: 10.32474/GJAPM.2019.01.000125
Abstract
The goal of our study was to report the clinical presentation, treatment, and attendance of enchondroma in the distal phalanx of the finger of a 45-year-old female patient. The presenting sinals as hyperkeratosis and melanonychia were recorded. A diagnosis was made by biopsy and anatomopathological. The surgical procedure was performed two times due recurrence of the tumor. The observational endpoint was a healing finger.
Keywords: Enchondroma; Melanonychia; Hyperkeratosis
Introduction
Chondromas are benign tumors defined by a hyaline or mature cartilage without the histological characteristics of chondrosarcoma as large cellularity, pleomorphism, presence of large cells with double nuclei or with mitoses. Most develop in the central part of the bone (enchondroma), although in some occasions they can be in the periphery of the bone (juxtacortical). The lesion may be solitary or may form part of a multiple enchondromatosis that affects several bones [1]. Enchondroma is the major responsible for the bone tumors of the hand. No well-established etiology is correlated, but some authors relate these lesions to congenital defects related to endochondral ossification failures. They usually present after the second decade of life, with a peak of concentration between 30 and 35 years and no difference between female and male [1]. The malignancy of the solitary enchondroma is rare, especially those located in the hands and feet; however this transformation is more frequent in cases of multiple enchondromatosis. Biopsy and pathology are mandatory to exclude malignancy in any soft tissue or bone tumor that rapidly increases or becomes painful [2]. Melanonychia, from Greek melaina, black, somber, resulting from an accumulation of melanin in the nail plate originating from the nail matrix. Several etiologies, among them, subungual melanoma, its etiological diagnosis becomes essential and as early as possible [3]. The present work aims at a review of the findings of the findings and the presentation of the atypical case of a white woman with a pigmented lesion in the nail bed of the first finger hand who underwent surgical treatment.
Chondroma
Unilateral enchondromatosis is a dyschondroplasia known as Ollier’s disease. Maffucci syndrome is characterized by multiple enchondromas associated with hemangiomas. The enchondroma may occasionally occur in the long bones (mainly the distal femur) proximal humerus and tibia. At these locations, it makes a differential diagnosis with bone infarction (usually painless, radiographic finding) and central chondrosarcoma (symptomatic, which causes erosion of the internal cortical bone). In this situation, the histological diagnosis between chondroma and grade I chondrosarcoma is very difficult. It is preferable to observe clinically and radiographically, comparing the images, before adopting any procedure. The clinical and radiographic behavior of the lesion should guide the behavior. Chondroma radiographically presents as a rarefaction lesion, sometimes with focus of calcification and may cause some deformity [4]. Treatment of chondroma is curettage of the lesion and placement of graft, if necessary. When it occurs on the outer surface of bones is called chondroma juxtacortical and should be treated surgically by parietal resection. The enchondroma is responsible for 90% of the bone tumors of the hand. They do not present well established etiology; however, some authors relate these lesions to congenital defects associated with endochondral ossification failures. They are generally present after the second decade of life, with a peak of concentration between 30 and 35 years and with no difference between the female and the male sex [4].
The malignant transformation of the solitary enchondroma is rare, especially those located in the hands and feet, however this transformation is more frequent in the cases of enchondromatosis multiple. Metaphysis or diaphysis chondromas (radiolucent, well demarcated, rounded or oval masses) result from the abnormal development of cartilage within the bone. Skeletal deformities and pathological fractures are common, and neurological deficits resulting from the invasion of cranial cranial junctions and the development of malignant tumors can occur. In general, they are bilateral and asymmetric. Bone lesions may appear before skin changes. The reported incidence of malignant transformation in enchondromas is 15 to 30%. Chondrosarcoma is the most common type of malignancy; others reported are angiosarcoma, fibrosarcoma, lymphangiosarcoma, intracranial tumors, ovarian neoplasia and pancreatic adenocarcinoma [2]. Malignant transformation most frequently are in long tubular and flat bones while this is far less common in the small bones of hands and feet. This is positive since enchondromas preferentially are located at the hands and feet [5]. Enchondromas are often inocent and the most discovered incidentally on imaging studies. However, pathologic fractures or nail lesions occurring in the area of the tumor may lead to the diagnosis [6]. Enchondroma usually can be diagnosed with plain radiography with typical features of a welldefined central lucency with or without speckles of calcification in the diaphysis or metaphysis of the bones of the hand. As the enchondroma grows, endosteal scalloping, cortical thinning, and expansile remodeling can happen [7]. The treatment consists of the removal of the skeletal and cutaneous lesions when possible. Biopsy is mandatory to exclude malignancy in any soft or bone tissue tumor that shows symptoms or exhibits progressive growth [2]. Melanonychia is a discoloration of the nail from brown to black that can be localized or diffuse. The localized form, whose main distribution is longitudinal, named as a longitudinal or striated melanonychia, is a stain that varies from light brown to black, compromising the nail plate from the proximal to the distal border [8]. The importance is the fact that the differential diagnosis is subungual melanoma, and because the diagnostic approach often ends in a biopsy and a surgical intervention that will certainly generate important and irreversible nail dystrophy for the patient. Because of this, the diagnostic intervention must be very well founded. In some cases, the etiological diagnosis is not that simple, even for the most experienced. The causes of melanonychia are varied, from fungal infection, trauma and consequent bruising and even melanoma [8,9], bring other causes that may result in longitudinal melanonychia, which are: subungual hematoma, being the most frequent cause, dermatoscopy and clinical history elucidate these cases with some ease. Exogenous pigmentation should always be remembered by contact with products such as silver nitrate, tobacco, henna and others.
The clinical history and the patient’s profession explain many cases; Fungal infections caused by trichophyton rubrum (var nigricans) and dematiaceous fungi such as Scytalidium dimidiate may have a blackish color; Addison’s disease, endocrinopathy, at the same time as promotes alteration in the pigmentation of the skin, can also affect shape of the nail plate; Treatment for HIV with Azidothymidine (AZT), such as the disease itself, can generate pictures of melanonychia. This drug injury begins at 8 weeks to 1 year after initiation of therapy; Nutritional deficiencies of vitamin B12 and folic acid can lead to melanonychia, whose color is more a blueish black, its correction can lead to complete reversal; Nonmelanocytic tumors, in rare cases, non-melanocytic tumors may stimulate melanogenesis and cause longitudinal melanonychia, its main cause being Bowen’s disease; Inflammatory diseases such as lichen planus, Hallopeau’s continuous dermatitis and pustular psoriasis are some entities that may present with longitudinal melanonychia. It is a sign that demands a lot of care and attention as biopsy is mandatory.
Case Report
We declare that all the precepts of Bioethics were fulfilled in the present case report, including with the signature by the patient of Term of Free and Informed Consent. MFPM female patient, white, 46 years old, an employee in a footwear company, in the role of auxiliary shoemaker in the Sinos Valley Region, Rio Grande do Sul. On February 19, 2018, she sought care due to first pain in right finger hand after a trauma in a drawer three days before. Making use of Tylenol and Nimesulide, without improvement of pain. Featuring edema, hyperemia, erythema and fluctuation in the region of the proximal nail fold, painful the mobilization. During the examination, hyperkeratosis was observed on the nail plate in 1/3 lateral, hypochromia in the range with no history of trauma. The patient reports having had the lesion for approximately five years and has performed numerous treatments, including topical antifungal and orally without any change in the condition. In this service, treatment with antibiotic therapy and analgesia as prescribed and sent to the outpatient surgeon to biopsy the nail injury with the presence of melanonychia and hyperkeratosis. On February 19, 2018, the surgical procedure was performed, sent to the biopsy specimen and mycological research, without intercurrences. Presenting the following results: Direct mycological and Culture: Straight: Blastoconidia; Culture: No fungal structures were visualized. The results of the pathology performed on February 27, 2018 presented material: I - Fragment of skin and nail bed; Macroscopic Examination: I-Two fragments of tissue, gray and shiny, measuring the largest 1.0x0.8x0.4cm; Diagnosis: I-Skin and tissue nail fragments containing cartilaginous tissue fragment; - The appearance is compatible with enchondroma (Figures 1-5).
Source: Author Archive.
Figure 1: A.1, A.2, A.3, A.4: clinical lesion of the fist right finger on February 19, 2018; B.1, B.2: clinical lesion of the first righthand finger on April 2, 2018; C.1, C.2: clinical lesion of the first right finger in 16 of April 2018; D.1, D.2: clinical lesion of the first right-hand finger on May 4, 2018; E.1, E.2: clinical lesion of the first right-hand finger on May 25, 2018.

Source: Author Archive.
Figure 2: A.1, A.2: Intraoperative injury by excision of the matrix and one third of nail plate, on June 25, 2018. B.1, B.2: postoperative lesion by excision in the matrix and one third of nail plate, on July 2, 2018. C.1: postoperative excision of lesion in the matrix and one third of nail plate, on July 9, 2018. D: evolution of the operative wound on July 30, 2018; E.1: evolution of the surgical wound on August 13, 2018. E.2: evolution of the surgical wound on October 19, 2018 presenting healthy nail matrix. E.3: Last picture on February 15, 2019 presenting healthy nail matrix.

Source: Author Archive.
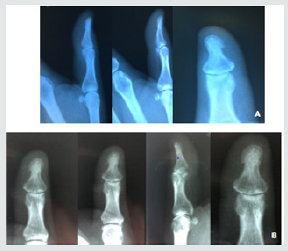
Figure 3: A: Right hand radiograph. Made on March 14, 2018 without pathology; B: radiography of the first right-finger on June 14, 2018.
Source: Dr. Daniel Canela Furian CRM 33936 - Histolab Laboratory - Feb. 2018.
Figure 4: Histopathological examination of the nail matrix of the first right finger. A: Cartilaginous tissue; B: Cartilaginous tissue; C: Cartilaginous tissue; D: Condrositos.
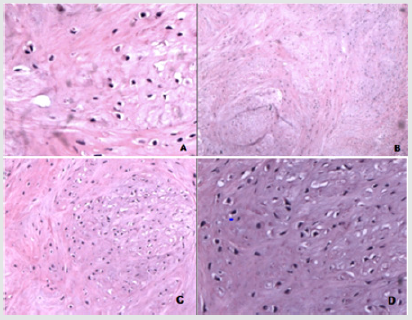
Source: Dr. Daniel Canela Furian CRM 33936 - Histolab Laboratory - Jul.2018.
Figure 5: Microscopic examination of the nail matrix of the first right finger. Subungual epithelium and stroma with fibrosis.

Patient underwent radiography on March 14, 2018 and Magnetic Resonance Imaging on March 15, 2018, of the right hand both after lesion excision and biopsy result. Presented the following results: right hand radiograph (examination performed on March 14, 2018): no alterations; Resonance of the right hand (examination performed on March 15, 2018): no changes. Patient returns to the unit after complete excision of the nail and result of the biopsy. It reports slight local sensitivity, in use of Rifamycin, topical. The anatomopathological of July 13, 2018, presented the following result: material: I - Nail matrix and Grocott staining (fungi). II - Fragment of nail. Macroscopic Examination: I-Fragment of fabric, gray and shiny, measuring 0,8x0,5cm. II - Fragment of brown nail, measuring 1.8x0.6cm. Diagnosis: I-Nail bed with fibrosis and chronic inflammatory infiltrate. Fungus research (GMS) is negative. II-Nail tissue with dystrophic alterations. Following the patient during the restoration of the nail plate. Hyperkeratosis returned in the same region, hyperchromic, a new x-ray and a new lateral 1/3 matricectomy were requested and treatment with Terbinafine for Onychomycosis was started.
Conclusion
Chondromas are rare tumors mainly in the nail matrix. A thorough examination of signs such as melanonychia due to the importance and severity of melanoma is essential. Importance of early biopsy and pathology for treatment. The postoperative follow-up in this case was necessary due to the recurrence of the lesion. The experience and educational guidance of the supervisor, Dra. Maria de Fátima Maklouf Amorim and the pathologist were essential for this clinical case.
References
- Baran R, Nakamura R (2011) Do diagnóstico ao tratamento: Condroma 1 ed Rio de Janeiro: Elsevier Editora Ltda.
- Azulay RD, Azulay, Abulafia (2015) Dermatologia: Púrpura e Afecções Vasculares. 6 ed Rio de Janeiro: Grupo Editorial Nacional e Guanabara Koogan.
- Bilemjian Apj et al. (2009) Melanoníquia: importância da avaliação dermatoscópica e da observação da matriz / leito ungueal. An Bras Dermatol. 84(2): 185-189.
- Lopes AC (2016) Tratado de clínica médica: Lesões Ósseas Tumorais e Pseudotumorais.
- Pansuriya TC, Kroon H, Bovée, Jvmg (2010) Enchondromatosis: insights on the different subtypes International journal of clinical and experimental pathology 3(6): 557-569.
- Reisler T, Viviano SL, Granick M (2015) Osseous Tumor of the Hand: Finger Enchondroma Eplasty 15(4).
- Sun TTT et al. (2017) Enchondroma of the Hand: Result of Surgery Curettage and Grafting and Possible Factors Affecting the OutcomeJournal of Orthopedics, Trauma and Rehabilitation 22: 13-17.
- lopes Os, Egito Ep (2010) Melanoníquia Estriada Melanoma - Boletim Informativo do Grupo Brasileiro de Melanoma Ano XIII, n 50 Julho, Agosto e Setembro.
- Wilson Ca, El Khayat, RH, Mckenna K (2015) Digitial endochondroma - Dermatology Online Journal 21(2).

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




