Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1403
Mini Review(ISSN: 2644-1403) 
Effects of the Type of Anesthesia (Inhalation or Intravenous) for Survival or Recurrence After a Cancer Surgery Volume 2 - Issue 4
Bonilla Castillo Luis*, Pérez Herrero, María A and Abad Anna
- The Department of General Surgery and the digestive system. University Hospital of Fuenlabrada, Spain
Received: January 27, 2020; Published: February 03, 2020
Corresponding author: Bonilla Castillo Luis, The Department of General Surgery and the digestive system. University Hospital of Fuenlabrada offers comprehensive surgical assistance, Spain
DOI: 10.32474/GJAPM.2020.02.000145
Frozen Shoulder
Surgery has a very important role in solid tumors multimodal treatment. The primary excision can be curative itself or can be combined with neoadjuvant or adjuvant chemotherapy and / or radiotherapy. Despite therapy advances, recurrence and metastases appear as an important source of morbidity and mortality in cancer patients. There is a huge growing interest in events related to surgery and the perioperative period that not only help to release cancer cells into general circulation, but also facilitate its growing, leading to regional recurrences and metastases. Data obtained from laboratory and animal experimentation suggest that anesthetics drugs may affect long-term results after cancer surgery. In this review, we summarize the experimental and clinical data that we have nowadays, and we present the potential role of anesthetic techniques (inhalation and intravenous) in cancer recurrence and survival.
Materials and Methods
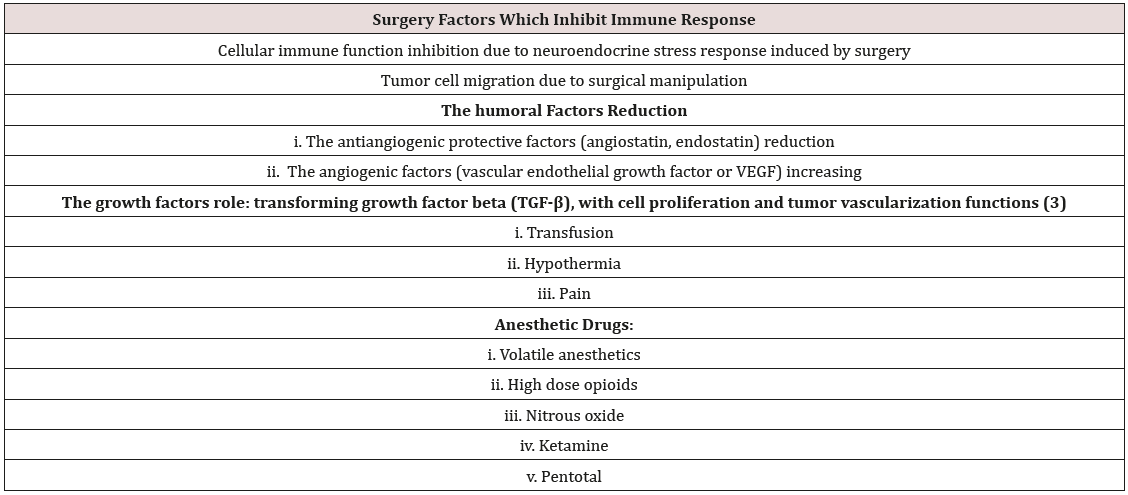
A bibliographic search has been done out using Medline / PubMed database and Embase, using as key words “anesthesia and metastasis”, “anesthetic drugs and cancer”, “halogenated and cancer”, “volatile anesthetic agents and cancer”, “propofol and cancer”, anesthetic technique and cancer”. They have been included the most relevant English or Spanish papers (Table 1).
Results
Experimental Evidence
a. Surgery itself and the neuroendocrine response related
to stress have a negative effect on immune system due to cellmediated
immunity depression they cause. Even after the
complete tumor excision, circulating tumor cells released during
the surgical procedure may lead to recurrence or metastasis
thanks to their ability to avoid immunological process [1].
Thereby, they can decrease antiangiogenic protective factors
concentration (e.g. angiostatin and endostatin) while increase
angiogenic factors such as vascular endothelial growth factor
(VEGF). Surgery is also associated with transforming growth
factor-beta (TGF-B) which plays a significant role in tumor
blood supply and cell proliferation [2].
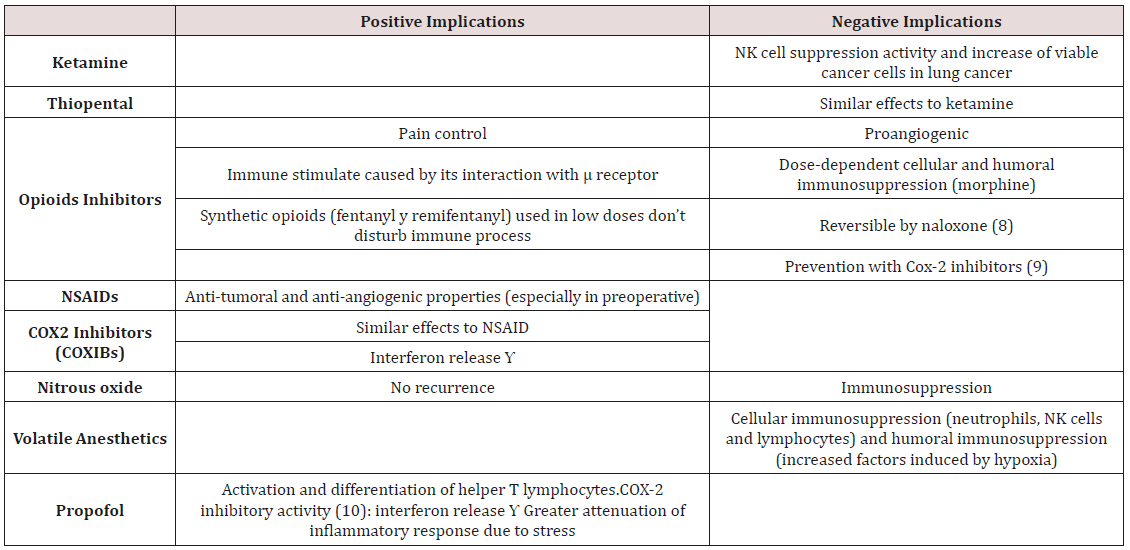
b. Anesthesia process also interacts with several immune
functions, including those related to neutrophils, macrophages,
dendritic cells, T cells and natural killer cells (NK). In vitro
studies about the possible metastasis induction of inhalation
anesthetics role are based on their time-and-dose-dependent
inhibitory effects. Thus, they modify neutrophil function,
suppress mononuclear cells cytokines release, decrease
lymphocyte proliferation and promote lymphocyte apoptosis.
Moreover, inhalation anesthetics also promote the growth and
proliferation of endothelial stem cells (proangiogenic effect)
which would improve tumor growth and / or teratogenicity
[3]. Nevertheless, propofol does not seem to depress immune
system, according to evidence available. It seems to improve NK
cells cytotoxicity, to reduce motility and tumor cells invasion, to
inhibit cyclooxygenase and to not promote HIF (antiangiogenic
effect) synthesis [4].
c. Opioid drugs inhibit both cellular and humoral human
immune function, increase angiogenesis and promote the
growth of breast tumoral cellular in rodents. In this way, they
also interfere with immune functions by depressing NK cells
activity [3] However, these drugs can reduce stress response
caused by pain and offer some benefit. Clinical evidence.
d. Most of the available evidence nowadays is based on
intermediate results (substituted variables: cell reduction,
inhibitory activity…) such as the previous ones mentioned and
the only studies with patient-centered results (final variables:
survival, mortality, recurrence) are the ones that we are going
to review. A recent retrospective analysis composed by more
than 7,000 patients from an oncology hospital in United
Kingdom was carried out to determine long-term survival of
patients who were receiving inhalation anesthesia (isofluoran
or sevofluorane) versus intravenous anesthesia (propofol and
remifentanil) in cancer surgery. After several analysis, including
multivariate analysis, it was found that those who received
inhalation anesthetics were those who had a lower survival (HR
[hazard ratio] 1.46; 95% CI 1.29-1.66 if we compared with the
group who received intravenous anesthesia [5].
e. Lee JH, the author of another retrospective analysis
composed by more than 300 patients taken from an oncology
hospital South Korea, determined the association between the
type of anesthesia (inhalation or intravenous) and recurrence
or survival in patients that have undergone radical mastectomy.
Large significant differences were not found between the
two groups about survival (HR of 0.550; 95% CI 0.311-
0.973) but they found a lower recurrence in the intravenous
anesthesia group Enlund M [6] found greater survival in
patients undergoing cancer surgery with propofol compared
to sevofluoran, but when multivariate analysis is used with
variables such as type of tumor (breast, colon and rectum), this
association disappears [7] (Table 2).
Discussion
Unfortunately, there is a drawback to available evidence; in vitro conditions used in many studies do not accurately replicate cancer cells biological condition. Therefore, the speculative extrapolation of these results to clinical scenario is not ideal. However, retrospective clinical studies about the type of anesthesia (inhalation versus intravenous) and cancer recurrence or survival after tumor excision are beginning to be published. The main disadvantages of these retrospective studies are selection, information and confusion biases. Wigmore [5], incorporated the propensity analysis, which is the best method to control known confounding variables in observational studies. However important variables such as type (including more than 20 cancer types with different prognoses), cancer stage or mortality attributable to cancer (despite it had been considered total mortality) was not considered. Notwithstanding that, the strength of this study falls on the large number of patients included. However, Lee JH [6] included in his study a single type and stage of cancer at the beginning of the study, but it still seemed that there were biases not included in the analysis, such as the use of nitrous oxide or morphics and the anesthetic technique preference of anesthesiologists. Moreover, they could also exist several hidden confounding factors which were not taken into account in a multivariate analysis of retrospective, observational, nonrandomized data. About these words, it is also important to consider the regional anesthetic techniques (RA), which are almost always a complement to general anesthesia. Studies have demonstrated lots of advantages of RA in cancer patients by reducing recurrences. The role of intrathecal and epidural opioids commonly used in regional analgesia and pain management has not been explored [8].
As mentioned previously, immune function combined with surgical stress and the direct effects of anesthetic drugs, create a favorable environment for tumor growth and dissemination, which finally affect patient survival. Reducing the response to surgical stress, minimizing inflammation and using optimal anesthetic and analgesic techniques are the main key to reduce long-term negative effects of cancer surgery. However, overall progress in this area, the actual lack of evidence leads to the impossibility of change our daily clinical practice. More and better randomized clinical trials, prospective cohorts are needed to prove that there is causality between the type of anesthesia and cancer recurrence.
References
- Peach G, Kim C, Zacharakis E, Purkayastha S, Ziprin P (2010) Prognostic significance of circulating tumour cells following surgical resection of colorectal cancers: A systematic review. Br J Cancer 102:1327-1334.
- Looney M, Doran P, Buggy DJ (2010) Effect of anesthetic technique onserum vascular endotelial growt factor C and transformig growth factor beta in women undergoing anesthesia and surgery for breast cáncer. Anesthesiology 113(5): 1118-1125.
- Tavare AN, Perry NJ, Benzonana LL, Takata M, Ma D (2012) Cancer recurrence after surgery: Direct and indirect effects of anesthetic agents. Int J Cancer 130(6): 1636-1643.
- Melamed R, Bar YS, Shakhar K, Ben ES (2003) Suppresion of natural killer cell activity and promotion of tumor metástasis by ketamine, thiopental, and halñotane, but not by propofol: Mediating mechanisms and prophylactic measures. Anesth Analg 97(5): 1331-1339.
- Wigmore Tj, Mohammed K, Jhanji S (2016) Long-term survival for patients undergoing volatile verssus IV anesthesia for cáncer surgery: A retrospective analysis. Anesthesiology 124(1): 69-79.
- Lee JH, Kang SH, Kim HA, Kim Bs (2016) Effects of propofol-based total intravenous anesthesia on recurrence and overall survival in patients after modified radical mastectomy: a retrospective study. Korean J Anesthesiol 69(2):126-132.
- Enlund M, Berglund A, Andreasson K, Cicek C, Enlund A, Bergvist L (2014) The choice of anaesthetic-sevofluorane or propofol- and outcome from cancer surgery: A retrospective analysis. Ups J Med Sci 119(3): 251-261.
- Bajwa SS, Anand S, Kaur G (2015) Anesthesia and cancer recurrences: The current knowledge and evidence. J Can Res Ther 11(3): 528-534.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...