Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2644-1403
Research Article(ISSN: 2644-1403) 
Comparative Evaluation Of Postoperative Pain Scores and Opioid Consumption In Septorhinoplasty After Administration Of Single-Dose Pre-Emptive Paracetamol and Ibuprofen: A Randomized Controlled Trail Volume 4 - Issue 5
Ali Abdullah AlShehri*
- Doctor of Medicine, Department of Surgery, Najran University, Saudi Arabia
Received: October 1, 2021; Published: October 12, 2021
Corresponding author: Ali Abdullah AlShehri, Doctor of Medicine, Department of Surgery, Najran University, Saudi Arabia
DOI: 10.32474/GJAPM.2021.04.000199
Abstract
Introduction: Septorhinoplasty operates on cartilage and bone of the nose and is ensued by severe postoperative pain. The objective of this study is to evaluate effects of preoperative administration of intravenous (IV) paracetamol and ibuprofen on postoperative pain scores in patients undergoing septorhinoplasty.
Methodology: 150 patients undergoing septorhinoplasty were randomly assigned into three groups with 50 patients in each group. The control group (Group A) was administered 100 ml saline solution, paracetamol group (Group B) was administered 1000 mg IV paracetamol in 100 ml saline and ibuprofen group (Group C) was administered 800 mg IV ibuprofen in 100 ml saline before surgery. Opioid analgesics were employed to achieve postoperative analgesia. Postoperative pain was evaluated using Visual Analogue Scale (VAS). Postoperative opioid consumption and adverse effects were also recorded for each patient.
Results: In comparison with Group A, VAS in Group B and Group C was statistically lower in all the time intervals (p<0.05). In 1st and 6th hours postoperatively, VAS in Group C was lower than Group B (p<0.05). In control group, total opioid consumption was highest in all time intervals (p<0.05). In Group C, total opioid consumption was significantly lower than Group B at 0-6 and 6-12 hours interval. (p<0.05).
Conclusion: Single-dose pre-emptive administration of ibuprofen has more profound postoperative analgesic effect than paracetamol during first 6 hours in septorhinoplasty. After first 6 hours of the procedure, there is no difference in analgesic effect between ibuprofen and paracetamol.
Keywords: Septorhinoplasty; Ibuprofen; Paracetamol; RCTs; VAS; Pre-emptive analgesia
Objective
Pain is considered as the fifth vital sign in modern medical practice. Hence apart from other vital parameters, evaluation of pain has become a primary and necessary requirement for proper patient care and comfort. Septorhinoplasty is an elective and ambulatory surgical procedure which involves massive hard and soft tissue manipulation in the nasal region of the face. The postoperative pain is severe in septorhinoplasty since it necessitates to operate on the nasal cartilage and bone [1]. This postoperative pain is often disturbing, distressing and requires efficient pain control management [2]. Severe postoperative pain can lead to complications such as delayed wound healing, ischemia, thromboembolism, pulmonary complications, immunological changes, increased hospitaliza tion and cost of treatment [3,4]. In this quest to provide effective postoperative pain control, patients are frequently prescribed opioids. Opioids acts centrally on the nervous system and thus have strong analgesic potential [5]. Although they provide relief in acute pain but are associated with opioid-related adverse events (ORAE), dependence, abuse, overdose and deaths [6]. This situation is undesirable and hence is the need to develop regimes which involves the avoidance of opioid overmedication and at the same time provide adequate analgesia. Therefore, American Society of Anaesthesiologist (ASA) has recommended the use of multimodal analgesia techniques involving local anaesthesia, regional anaesthesia and non-steroidal anti-inflammatory drugs (NSAIDs) to potentiate pain relief and reduce adverse effects [7].
Pre-emptive analgesia is one such modality to reduce the severity and duration of postoperative pain. Pioneered by George W Crile, it is an antinociceptive drug administration done before tissue trauma to prevent the peripheral, central sensitization and hyperexcitability of the central nervous system [8]. This decreases the nerve sensitization and thereby reduces postoperative hyperalgesia and allodynia [9]. Administration of apt analgesia at appropriate time, dose and form before the surgical procedure has shown to reduce postoperative pain and need of analgesia. Pre-emptive analgesia also contributes to comfortable recovery, reduces the need of opioid consumption, improves patient’s satisfaction, outcomes and reduces cost of care [10]. Thus, the combination of multimodal and pre-emptive analgesia techniques in post-operative pain management have been researched and clinically experimented. Recently, pre-emptive intravenous (IV) administration of ibuprofen and paracetamol for post-operative pain management has been extensively researched. Ibuprofen is a common NSAID with anti-inflammatory, analgesic and antipyretic effect. It is a non-specific inhibitor of cyclooxygenase (COX) enzymes (COX-1 and COX-2 isoenzymes) which is associated with the analgesic effect [11]. Ibuprofen does not increase the risk of bleeding or gastrointestinal problems [12]. Paracetamol is another time-tested safe drug with analgesic and anti-pyretic effect but no anti-inflammatory action. Paracetamol acts centrally which effects both the peripheral and central antinociception process [13]. Clinically, paracetamol is more advantageous and safer over other NSAIDs since it causes less gastric irritation, antiplatelet activity and untoward drug interactions [14]. The primary objective of this present study is to evaluate the effects of preoperative administration of IV paracetamol and IV ibuprofen on postoperative pain scores in patients undergoing open septorhinoplasty. The study also aims to evaluate the postoperative opioid consumptions in patients treated with pre-emptive analgesia approach. The secondary objective of this study is to evaluate the incidence of adverse effects associated with the study drugs.
Material and Methods
Ethics: The study was conducted at Najran University Hospital, Saudi Arabia and ethical approval was obtained from the institutional ethics committee. The study protocols were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000.
Study Design: It was a prospective, randomized and doubleblinded study in which 150 patients between 18-60 years of age to be operated for open septorhinoplasty with ASA physical status I-II and planned hospitalization stay of minimum 24 hours were included. Written and informed consent form was obtained from each patient. Demographic data including age, gender, Body Mass Index (BMI), ASA score, duration of surgery (minutes) and duration of anaesthesia (minutes) were recorded. Patients graded ASA III and above, with history of renal, hepatic, cardiovascular or pulmonary disease, allergy to study drugs, long-term abuse of NSAIDs or opioids, history of Angiotensin Converting Enzyme (ACE) inhibitors, furosemide or aspirin use, bleeding diathesis, platelet dysfunction, gastrointestinal disease, peptic ulcers, neuropathic diseases, pregnancy, those planning pregnancy in near future, breastfeeding mothers were excluded in this study.
On the day of the scheduled surgery, the patients were explained about the study protocol, drugs used in the study, visual analogue scale (VAS). A computer software program was used to assign patients in three random groups (Group A – control, n=50; Group B – paracetamol, n=50; Group C – Ibuprofen, n=50). Group A was administered 100 ml of saline solution, Group B was given 1000 mg IV paracetamol in 100 ml saline and Group C received 800 mg ibuprofen in 100 ml saline before the surgical procedure. General anaesthesia was administered after a 30 min waiting period in all the three groups. Propofol 2-3 mg/kg, rocuronium 0.6 mg/kg and fentanyl 50-75 mcg were administered during induction. Anaesthesia was maintained with sevoflurane 2% in 40-60% oxygen-air mixture and remifentanil 0.125 μg/kg/ min intravenously. Standard ECG, peripheral oxygen saturation level (SpO2) and non-invasive blood pressure were monitored and recorded in all the patients. All the surgical procedures were performed by the same surgical team using similar technique. Fifty milligram (50 mg) of tramadol was administered to all the patients about 30 min before the end of surgery. Following surgery and extubation all patients were taken to postoperative care unit.
The patient, surgical team and anaesthesiologist were blinded to the study drugs. Postoperative pain intensity was self-assessed by the patient using visual analogue scale (VAS 0 = no pain, VAS 10 = the most severe pain) in the presence of nurse who was blinded to the drugs and groups. VAS was recorded at 1st, 6th, 12th and 24 hour interval. Opioid consumption was measured at 0-6, 6-12 and 12-24 hours interval and total at 24 hours. Pethidine 0.25mg/ kg was given to patients with VAS score of 4 and above for rescue analgesia. During postoperative care, all the patients received single dose of 0.5 mg/kg methyl prednisolone to control inflammation and 40 mg esomeprazole for gastric protection. During the 24 hour postoperative follow-up duration, the adverse effects of the drugs used in the study was recorded. Events of constipation, bleeding, nausea, vomiting, respiratory depression, sedation/confusion, urinary retention, pruritus and dyspepsia were charted for each patient.
Statistics: The statistical analysis was performed by IBM SPSS 20.0 software program. Power analysis was performed based on the total opioid (Pethidine) consumption. It was found that the sample size was 95.42 in the 95% confidence interval and the power was 0.99 in the significance level. This indicates that the sample size is sufficient. The descriptive statistics were explained as mean±SD. The data distribution was analysed using the Kolmogorov-Smirnov test. The Pearson’s chi-square test was used to compare the categorial data between the three groups. One-way ANOVA followed by Tukey’s test was used to evaluate the differences amongst groups at 5% significance level for normally distributed continuous variables.
Results
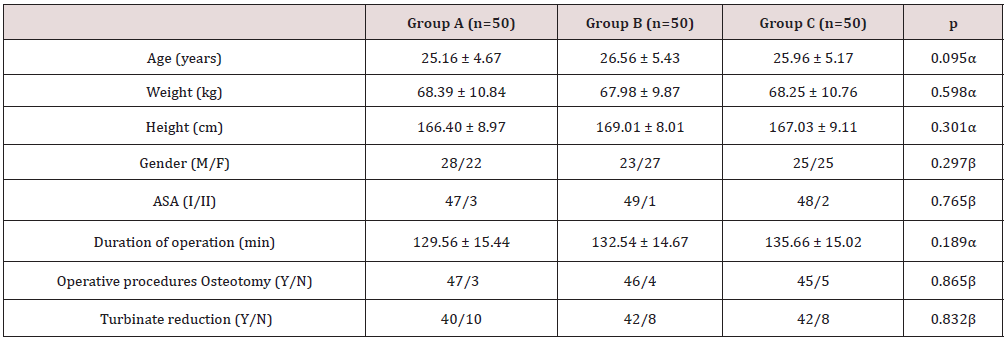
In this study, each group included 50 patients. Baseline demographic data, duration of operation and type of operative procedure showed no statistical difference between the groups (p<0.05) Table 1.
Values are expressed in mean ± standard deviation or number
ASA American Society of Anesthesiologist
αp>0.05 One-way ANOVA between groups
βp>0.05 chi-square test between groups
Postoperative VAS pain score were significantly lower in Group B and Group C compared to Group A at 1st, 6th, 12th and 24 hour interval (p<0.05). Postoperative VAS pain scores were significantly lower in Group C compared to Group B at 1st and 6th hour interval Table 2.
Values are expressed in mean ± standard deviation or number
VAS Visual Analogue Scale
αp<0.05 One-way ANOVA compared with Group A
βp<0.05 One-way ANOVA compared with Group B
γp>0.05 One-way ANOVA compared with Group B
Postoperative opioid (Pethidine) consumption was significantly lower in Group B and C compared to Group A (p<0.05). In the 0-6 hours’ time interval, total postoperative opioid consumption was significantly lower in Group C compared to Group B (p<0.05). Group B and C had statistically fewer rescue analgesia than Group A at all time intervals Table 3.
Table 3: Comparison of total postoperative opioid (Pethidine) consumption and rescue analgesia between Group A, Group B and Group C.

Values are expressed in mean ± standard deviation or number
α p<0.05 One-way ANOVA compared with Group A
β p<0.05 One-way ANOVA compared with Group B
γ p>0.05 One-way ANOVA compared with Group B
a p<0.05 chi-square test compared with Group A
b p<0.05 chi-square test compared with Group B
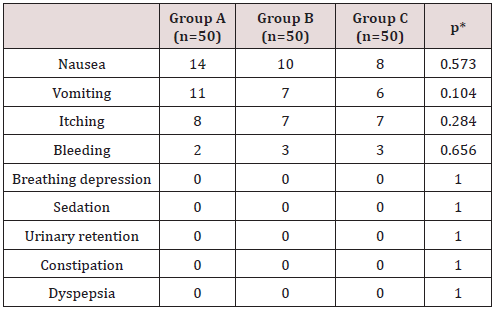
In terms of adverse effects, no differences were found in their incidence between the groups as a result of the medications used in the study Table 4.
Values are expressed in mean ± standard deviation
*p>0.05
Discussion
Rapid resumption of routine activities after surgical procedures is dependent on efficient postoperative pain management and minimum opioid consumption. This becomes more important in ambulatory and elective surgical procedure like septorhinoplasty or other facial plastic surgery which are routinely performed for cosmetic and functional purposes. In this study, it was found that the pre-surgical administration of intravenous ibuprofen or paracetamol significantly reduced the postoperative pain score and opioid consumption in the 24 hours post-surgical period in comparison to control in patients treated for septorhinoplasty. Also, the utilization of rescue analgesia was significantly lower in the ibuprofen group followed by the paracetamol group and control group. Compared to septoplasty, septorhinoplasty is associated with severe post-surgical pain as extensive hard-tissue incursion is involved [15]. Postoperative pain and discomfort can lead to increased hospital stay, extend healthcare cost, reduce readmission rates, and reduce patient satisfaction [16,17]. This can be controlled by effective and efficient postoperative pain management. Opioids have mostly remained the front-line drugs for the management of postoperative pain. Nevertheless, these opioids are associated with multifarious systemic adverse effects which hampers the post-surgical well-being of the patient [6]. Other drugs such as GABA, local anesthesia, NSAIDS and α-agonist have also been experimented for analgesic regime in patients treated for septorhinoplasty [18]. In the recent decade, clinicians and researchers have used alternative and combination analgesic strategies to reduce their over-reliance on opioids and still provide adequate analgesia. Intravenous paracetamol and ibuprofen are two such drugs which have been studied actively considering their safety and analgesic profile.
In this study, 800 mg of IV ibuprofen provided better analgesic effect and reduced postoperative opioid consumption compared to 1 g IV paracetamol in the first 6 hours after the surgery. This can be attributed to the superior anti-inflammatory and COX inhibition capacity of ibuprofen. COX-1 contributes to bleeding and gastro-intestinal adverse effects. COX-2 is responsible for the ideal analgesic, anti-inflammatory and anti-pyretic effect. The inhibition rate of COX-1 to COX-2 is 2.5:1 for ibuprofen, which is accountable for its lower risk of bleeding, constipation, and other undesirable gastrointestinal adverse effects. Other NSAIDs such as ketorolac have inhibition rate of 330:1 which increases the risk of bleeding [19]. A recent systematic review and meta-analysis has concluded that ibuprofen is not associated with an increased risk of postoperative bleeding in plastic surgery [20]. The other experimental drug in this study, paracetamol is known to have less contraindication, well established safety profile and lacks significant drug interactions [21]. Due to its lack of peripheral COX- 1 inhibition, paracetamol doesn’t amplify the risk of postoperative bleeding and is considered safe [22]. The concern for bleeding is compounded in septorhinoplasty due to the risk of epistaxis. Since nose is a highly vascular region, packing it leads to increased pressure and obstruction contributing to significant bleeding [23]. Hence IV ibuprofen and paracetamol can be used safely in patients treated for septorhinoplasty without the risk of associated bleeding. The incidence of other adverse effects such as nausea, vomiting and itching were more in the control group because of higher opioid use in them. The requirement of rescue analgesia was less in ibuprofen and paracetamol groups, but no statistically significant difference was found in any of the three groups regarding adverse effects.
The contemporary literature hosts many studies regarding pre-emptive and multi-modal analgesia techniques to reduces postoperative pain and concurrent opioid consumption. Recently, Celik et al [24] have reported more analgesic effect and less opioid consumption for 12 hours postoperatively with pre-emptive dose of 800 mg ibuprofen compared to 1 g of paracetamol in patients treated for septorhinoplasty. Gozeler et al [25] suggested that pre-emptive dose of 800 mg IV ibuprofen, 30 min before septorhinoplasty is beneficial in reducing pain score and opioid consumption. In studies performed on other surgical procedures, Southworth et al [26] found that 800 mg IV ibuprofen was more efficient in reducing pain and opioid use than 400 mg IV ibuprofen and placebo in patients treated for orthopedic and abdominal surgeries. In patients treated with elective orthopedic surgery, Singla et al [27] reported 31% reduction in opioid consumption and pain levels with pre-emptive administration of IV ibuprofen. In multi-centered placebo-controlled trail by Martinez et al [28] for abdominal and orthopedic surgeries, they reported significant reduction in opioid use (52%) and reduced pain levels with 800 mg of IV ibuprofen. Moss [29] reported a reduction of postoperative fentanyl use with pre-emptive dose of 800mg IV ibuprofen in pediatric tonsillectomy. In laparoscopic cholecystectomy, Ahiskalioglu et al. [30] found that pre-emptive single dose of 400 mg IV ibuprofen significantly reduced the postoperative pain and opioid consumption compare to placebo.
In studies comparing the pre-emptive effect of ibuprofen and paracetamol, Ekinci et al. [31] found that IV ibuprofen resulted in lower pain scores and lower opioid use in comparison with IV acetaminophen (paracetamol) in first 24 hours postoperatively in patients treated with laparoscopic cholecystectomy surgery. Similar finding has been reported by Ciftci et al. [32] in patient after laparoscopic sleeve gastrectomy. In oral surgical procedures, Viswanath et al [33] have found that pre-emptive analgesia with 800 mg IV ibuprofen is more effective than 1 g acetaminophen in reducing postoperative pain and opioid use after third molar surgery. However, Kayhan et al. [34] reported that in comparison to IV acetaminophen, IV ibuprofen did not significantly reduce the postoperative opioid consumption but reduced the severity of pain in bariatric surgery. The studies have employed ibuprofen and paracetamol separately for clinical evaluation. Since both of these drugs are efficacious and have established safety profile, they can be co-administration or used in combination. Gupta et al [35] have reported that 800 mg IV ibuprofen combined with 1 g IV acetaminophen significantly decreased pain level, opioid consumption and opioid-related adverse effects in patients undergoing knee or hip arthroplasty. In lower wisdom tooth extraction, combination of 400 mg ibuprofen and 1000 g paracetamol have shown to provide better analgesic effect than 200 mg ibuprofen and 500 mg paracetamol or 400 mg ibuprofen or 1 g paracetamol [36]. There are few limitations to this study. Fixed dose of 800 mg ibuprofen and 1 g paracetamol were used irrespective of the weight and profile of the patient. Ibuprofen is available in 400 and 800 mg forms. Further studies can be planned with different dose combinations. Studies involving co-administration of IV ibuprofen and paracetamol in patients treated for septorhinoplasty can be done. The sample size was calculated based on opioid requirement, the primary aim. Studies with large sample size might be required to study the adverse effects of experimental drugs. The cost of postoperative care and length of hospital stay has not been evaluated in this study. Since all patients received 0.5 mg/kg methyl prednisolone in the postoperative period, the analgesic efficiency of steroid was not considered or evaluated. Also, this study did not evaluate the reduction of swelling and bruising in patients postsurgically which is an important factor for their early return to normal daily routine. Further research can be done considering the limitations of the present study.
Conclusion
In concluding this study, I have found that a single-dose pre-emptive IV administration of 800 mg ibuprofen and 1 g paracetamol before septorhinoplasty contributes significantly in postoperative pain reduction and opioid consumption in these patients. On comparing ibuprofen with paracetamol, postoperative VAS pain scores are lower with ibuprofen for the first 6 hours after which the difference is non-significant. In terms of postoperative rescue analgesia usage, the opioid consumption was less in the ibuprofen group for the 0-6 hours after the surgery as compared to paracetamol. No serious adverse effects were observed with any of the study drugs. Thus, the author recommended the use of preemptive analgesia strategies involving IV ibuprofen or paracetamol to achieve adequate analgesic and reduce opioid requirement in patients being treated for septorhinoplasty.
References
- Sener M, Yilmazer C, Yilmaz I, Caliskan E, Donmez A, et al. (2008) Patient-controlled analgesia with lornoxicam vs. dipyrone for acute postoperative pain relief after septorhinoplasty: a prospective, randomized, double-blind, placebo-controlled study. Eur J Anaesthesiol 25: 177-182.
- Szychta P, Antoszewski B (2010) Assessment of early post-operative pain following septorhinoplasty. J Laryngol Otol 124: 1194-1199.
- Kehlet H, Holte K (2001) Effect of postoperative analgesia on surgical outcome. Brish J Anaesth 87: 62-72.
- Koh W, Nguyen KP, Jahr JS (2015) Intravenous non-opioid analgesia for peri- and postoperative pain management: a scientific review of intravenous acetaminophen and ibuprofen. Korean J Anesthesiol 68(1): 3-12.
- Oderda GM, Said Q, Evans RS (2007) Opioid-related adverse drug events in surgical hospitalizations: Impact on costs and length of stay. Ann Pharmacother 41: 400-406.
- Benyamin R, Trescot AM, Datta S (2008) Opioid complications and side effects. Pain Physician 11: S105-S120.
- (2012) American Society of Anesthesiologists Task Force on Acute Pain Management. Practice guidelines for acute pain management in the perioperative setting: an update report by the American Society of Anesthesiologist Task Force on acute pain management. Anesthesiology 116: 248.
- Crile GW (1913) The kinetic theory of shock and its prevention through anoci-association. Lancet 185: 7-16.
- Ong CK, Lirk P, Seymour RA, Jenkins BJ (2005) The efficacy of preemptive analgesia for acute postoperative pain management: a meta-analysis. Anesth Analg 100(3): 757-773.
- Kelly DJ, Ahmed M, Brull SJ (2001) Preemptive analgesia I: physiological pathways and pharmacological modalities. Can J Anaesth 48(10): 1000-1010.
- Scott LJ (2012) Intravenous ibuprofen: in adults for pain and fever. Drugs 72: 1099-1109.
- Song K, Melroy MJ, Whipple OC (2014) Optimizing multimodal analgesia with intravenous acetaminophen and opioids in postoperative bariatric patients. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy 34(S1): 14S-21S.
- Bebenista MJ, Nowak JZ (2014) Paracetamol: Mechanism of action, applications and safety concern. Acta Pol Pharm 71(1): 11-23.
- Bonnefont J, Courade JP, Allaoui A, Eschalier A (2003) Mechanism of the antinociceptive effect of paracetamol. Drugs 63: 1-4.
- Aydil U, Yilmaz M, Akyildiz I, Bayazit Y, Keseroglu K, et al. (2008) Pain and safety in otorhinolaryngologic procedures under local anesthesia. J Otolaryngol Head Neck Surg 37: 851-855.
- White PF (2005) The changing role of non-opioid analgesic techniques in the management of postoperative pain. Anesth Analg 101(5 suppl): S5-S22.
- Hogg RP, Prior MJ, Johnson AP (1999) Admission rates, early readmission rates and patient acceptability of 142 cases of day case septoplasty. Clin Otolaryngol Allied Sci 24: 213-215.
- Nguyen BK (2019) Perioperative analgesia for patients undergoing septoplasty and rhinoplasty: An evidence-based review. Laryngoscope 129(6): E200-E212.
- Kroll PB (2012) Intravenous ibuprofen for postoperative pain. Pain Manag 2: 47-54.
- Kelley BP, Bennett KG, Chung KC, Kozlow JH (2016) Ibuprofen may not increase bleeding risk in plastic surgery: a systematic review and meta-analysis. Plast Reconstr Surg 137: 1309-1316.
- Bonnefont J, Courade JP, Alloui A, Eschalier A (2003) Antinociceptive mechanism of action of paracetamol. Drugs 63: 1-4.
- Arslan M, Çiçek R, Celep B, Yılmaz H, Üstün-Kalender H (2011) Comparison of the analgesic effects of intravenous paracetamol and lornoxicam in postoperative pain following thyroidectomies. Agri 23: 160-166.
- Meraj TS, Bresler A, Zuliani GF (2020) Acute pain management following facial plastic surgery. Otolaryngol Clin N Am 53(5): 811-817.
- Celik EC, Kara D, Koc E, Yayik AM (2018) The comparison of single-dose preemptive intravenous ibuprofen and paracetamol on postoperative pain scores and opioid consumption after open septorhinoplasty: a randomized controlled study. Eur Arch Otorhinolaryngol 275(9): 2259-2263.
- Gozeler MS, Sakat MS, Kilic K (2018) Does a single-dose preemptive intravenous ibuprofen have an effect on postoperative pain relief after septorhinoplasty? Am J Otolaryngol 39(6): 726-730.
- Southworth S, Peters J, Rock A, Pavliv L (2009) A multicenter, randomized, double-blind, placebo-controlled trial of intravenous ibuprofen 400 and 800 mg every 6 hours in the management of postoperative pain. Clin Ther 31(9): 1922-1935.
- Singla N, Rock A, Pavliv L (2010) A multi-center, randomized, double-blind placebo controlled trial of intravenous-ibuprofen (IV-ibuprofen) for treatment of pain in post-operative orthopedic adult patients. Pain Med 11(8): 1284-1293.
- Gago Martínez A, Escontrela Rodriguez B, Planas Roca A, Martínez Ruiz A (2016) Intravenous ibuprofen for treatment of post-operative pain: a multicenter, double blind, placebo-controlled, randomized clinical trial. PLoS One 11(5): e0154004.
- Moss JR, Watcha MF, Bendel LP, McCarthy DL, Witham SL, et al. (2014) A multicenter, randomized, double-blind placebo-controlled, single dose trial of the safety and efficacy of intravenous ibuprofen for treatment of pain in pediatric patients undergoing tonsillectomy. Paediatr Anaesth 24(5): 483-489.
- Ahiskalioglu EO, Ahiskalioglu A, Aydin P, Yayik AM, Temiz A (2017) Effects of single-dose preemptive intravenous ibuprofen on postoperative opioid consumption and acute pain after laparoscopic cholecystectomy. Medicine 96(8): e6200.
- Ekinci M (2020) A Randomized, Placebo-Controlled, Double-Blind Study that Evaluates Efficacy of Intravenous Ibuprofen and Acetaminophen for Postoperative Pain Treatment Following Laparoscopic Cholecystectomy Surgery. J Gasterointest Surg 24(4): 780-785.
- Ciftci B (2019) Comparison of Intravenous Ibuprofen and Paracetamol for Postoperative Pain Management after Laparoscopic Sleeve Gastrectomy. A Randomized Controlled Study. Obes Surg 29(3): 765-770.
- Viswanath A, Oreadi D, Finkelman M, Klein G, Papageorge M (2019) Does Preemptive administration of IV ibuprofen (Caldolor®) IV acetaminophen (Ofirmev®) reduce postoperative pain and subsequent narcotic consumption following third molar surgery? J Oral Maxillofac Surg 77(2): 262-270.
- Erdogan Kayhan G, Sanli M, Ozgul U, Kirteke R, Yologlu S (2018) Comparison of intravenous ibuprofen and acetaminophen for postoperative multimodal pain management in bariatric surgery: A randomized controlled trial. J Clin Anesth 50: 5-11.
- Gupta A, Abubaker H, Demas E, Ahrendtsen L (2016) A Randomized Trial Comparing the Safety and Efficacy of Intravenous Ibuprofen versus Ibuprofen and Acetaminophen in Knee or Hip Arthroplasty. Pain Physician 19(6): 349-356.
- Bailey E, Worthington H, Coulthard P (2014) Ibuprofen and/or paracetamol (acetaminophen) for pain relief after surgical removal of lower wisdom teeth, a cochrane systematic review. Br Dent J 216(8): 451-455.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...