Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4692
Research Article(ISSN: 2637-4692) 
Evaluation of Anti-Staining Property of Chlorhexidine with Anti-Discoloration System and Its Effect on Dental Plaque Reduction”- A Clinical Study Volume 3 - Issue 4
Anjana Yogesh1*, Megha Chethan2, Rashmi M3, Latha M4, Hema N5 and Karthik D Yadav6
- 1Department of Periodontics, Master of Dental surgery, KGF College of Dental Sciences, India
- 2Department of Conservative & Endodontics, Master of Dental surgery, KGF College of Dental Sciences, India
- 3Department of Public health Dentistry, Master of Dental surgery, KGF College of Dental Sciences, India
- 4Department of Oral pathology, Master of Dental surgery, KGF College of Dental Sciences, India
- 5Department of Pedodontics & preventive dentistry, Master of Dental surgery, KGF College of Dental Sciences, India
- 6Department of Oral medicine & Radiology, Master of Dental surgery, KGF College of Dental Sciences, India
Received:May 10, 2019; Published: May 17, 2019
Corresponding author:Anjana Yogesh, Department of Periodontics, Master of Dental surgery, KGF College of Dental Sciences, India
DOI: 10.32474/MADOHC.2019.03.000169
Introduction
Infections are not an uncommon incidence anymore and are prevalent in one form or the other in day to day life. They are highly opportunistic in nature and many microorganisms which are normal floral inhabitants are found to be pathogenic in nature when they are excess in nature. The lack of supra-gingival plaque control is the main cause for the high prevalence of gingivitis and periodontitis. The presence of plaque reflects the lack of qualitative care of the oral cavity of the individual and the use of oral hygiene appliance and their aids. Further, plaque control can be achieved by mechanical as well as chemical methods, or a combination of both as the incomplete removal and limited accessibility of the mechanical means is overcome by the chemical means [1,2].
An inflammatory disease affecting the supporting structures of the teeth which leads to the progressive loss of the connective tissue and the alveolar bone is termed as periodontitis. Even though microbial dental plaque is the primary factor responsible for periodontitis, but it is not the sole factor as it is multifactorial in nature [1]. Chlorhexidine is the most effective chemical antiplaque agent, which is well known for its broad-spectrum antimicrobial activity within the oral cavity. It has bactericidal action as well as prolonged bacteriostatic action partially by adsorption to pellicle coated enamel surface and by blockage of bacterial glyosidic and proteolytic enzymes, which in turn reduces the ability of bacteria in plaque to degrade host-derived proteins & glycoprotein for nutrition [3]. Chlorhexidine which is considered as gold standard in chemical debridement has its own drawbacks which include staining of teeth, taste alteration and form lesions that are desquamatory and erythematous in nature. After prolonged use, brownish pigmentation of the tooth surface, prosthesis and tongue can be appreciated [4].
The exact mechanism of action for chlorhexidine staining remains a myth. The tests available indicate the causes of staining to be non – enzyme browning or Millard reactions which release brown-staining substances known as Melanoidins. Staining is due to the result of local precipitation reaction occurring between toothbound chlorhexidine and chromogens found within foodstuffs and beverages [5]. Different formulations are added to chlorhexidine to reduce the brown pigmentation such as peroxyborate, polyvinyl pyrrolidone, sodium meta-bisulphite & ascorbic acid [4]. The purpose of this clinical study was to compare and evaluate the rate of stain formation with chlorhexidine and chlorhexidine with an anti-discoloration system (Curasept ADS*) and its effect on dental plaque reduction, after periodontal flap surgery.
Materials and Methods
A total of 30 patients fulfilling the inclusion and exclusion criteria were selected from the outpatient department of Periodontics, Krishnadevaraya College of Dental Sciences and Hospital, Bangalore.
An informed consent was taken from all the patients who were part of the study. The study was a split mouth, double-blind randomized clinical trial of 30 patients scheduled for periodontal flap surgery 30 patients with chronic periodontitis, requiring flap surgery were included in the study and were divided into 2 groups.
The sites selected were divided into (Table 1)
1. Group 1 (CHX group)-30 patients rinsed with 10ml of 0.2% chlorhexidine mouthwash following flap surgery twice daily for 2 weeks.
2. Group 2 (CHX ADS group) -30 patients rinsed with 10 ml of 0.2% chlorhexidine ADS following flap surgery twice daily for 2 weeks.
a) Inclusion Criteria:
I. Patients with chronic periodontitis requiring flap surgery in a minimum of two sextants with at least two teeth in each sextant.
II. Systemically healthy patients.
III. Patients willing to participate in the study.
b) Exclusion Criteria:
I. Patients allergic to chlorhexidine.
II. Patients with smoking and pan chewing habits.
III. Patients on any oral medications known to cause staining of teeth.
IV. Presence of fixed or removable orthodontic appliances, crowns and restorations.
The following observations will be made
a. Clinical parameters will be assessed for all the patients using plaque index, gingival index and bleeding on probing before and two weeks after periodontal flap surgery.
b. A photographic analysis will be made before and at two weeks after periodontal flap surgery (Table 2).
Assesment Protocol
Day 0 – The first time patient reported to the department, during which clinical parameters {PI (Plaque Index- Turesky Gilmore Glickman modification of the Quigley and Hein plaque index, 1970), GI (Gingival Index (Loe and Silness, 1963), and BOP (Ainamo and Bay index,1975)} were recorded and oral prophylaxis was done.
Day 14 – Clinical parameters were recorded.
I. Prophylaxis with low speed rubber cup was done.
II. Digital photographs were taken
III. Flap surgery was performed
-Patients were started on mouthwash (CHX / CHXADS) Day 28- Two weeks after flap surgery and after use of mouth wash
I. Clinical parameters (PI, GI, and BOP) were recorded
II. Digital photographs were taken
A wash out period of 2 weeks was given. After which the same procedure, clinical parameters (PI, GI, and BOP) and photographic analysis was carried out in the other quadrant (Graph 1).
Discussion
In the year 1940, Imperial Chemical Industries in England developed chlorhexidine and was investigated as an anti-plaque agent in 1969, after which Loe and Schiott in 1970 conducted a study for the same [6]. The capability of Chlorhexidine to effectively control plaque makes it the gold standard chemical antimicrobial agent. It is a very effective adjuvant to mechanical therapy.6 However, side effects such as yellow brown or black stains on tongue and teeth and burning sensation of the mouth due to the alcohol content are the drawbacks of the chemical agent. Further, the presence of alcohol in a mouth rinse is a topic of marked controversy as its presence may be related with the increased risk of oral cancer and is an absolute contraindication in patients with mucositis and head and neck irradiation. However, alcohol is used as a vehicle for the stability and activity of other active ingredients [4].
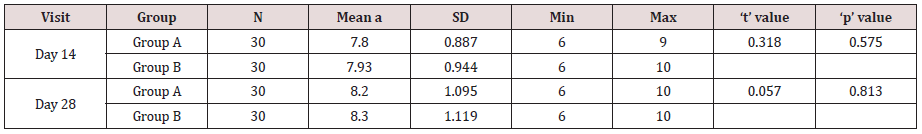
CHX ADS is an alcohol-free mouthwash, which prevents staining of teeth and tongue. It consists of sodium meta-bisulphite and ascorbic acid, which are active agents with a synergistic effect, increasing antiplaque activity and preventing staining of the teeth and tongue [5]. In the present study, intra group observations revealed a statistically significant reduction in plaque scores for both group A and group B. There was a statistically significant difference seen in the inter-group comparison of plaque scores with greater reduction in group A at all time intervals. The gingival index scores of the subjects included showed statistically significant reduction in both group A and group B at all time intervals with better results in group A. The results were found to be consistent with a study conducted by Arweiler, et al. where they concluded that conventional CHX is superior to CHX ADS in inhibiting plaque [7]. In our study the conventional (alcohol-containing) chlorhexidine solution proved to be the product with the greater plaqueinhibiting effects. Vigreant, et al. in his study has hypothesised that the reduced efficacy of chlorhexidine-ADS against plaque formation might be due to the absence of alcohol in CHX ADS which could be responsible for the potential stability and action of chlorhexidine [8.9] (Graph 2).
Arweiler, et al. has suggested that meta-bisulphite and ascorbic acid in CHX ADS, may compete against the chlorhexidine molecule and/or inhibit the adhesion of the positively charged molecule to the tooth substance or other intra-oral structures [10]. Clayton et al in his study found that reduction in the tendency to stain may be related to the loss of plaque inhibition [11]. The present study showed that there was no statistically significant difference in the pre-rinsing and post-rinsing L, a, b values in both the groups. These results are consistent with the study conducted by Addy, et al. (2005) where it was concluded that the CHX ADS rinse has the same staining potential as a conventional, well-established, alcohol-containing chlorhexidine solution [12,13].
In contrast to the study conducted by Cortellini, et al. and Bernaldi, et al. showed similar antiplaque efficacy and simultaneously lesser staining compared with a conventional 0.2% chlorhexidine mouthwash [4,5]. A possible explanation for the similar intensity of the colour of the teeth after rinsing with the CHX and CHX ADS mouthwash could be due to the inherent colour of the teeth in CHX ADS group and a lack of control over dietary chromogens [12,13]. Within the limits of the study both CHX and CHX ADS were effective in reducing plaque, gingival inflammation and bleeding on probing, however 0.2% CHX proved to be the product with greater plaque inhibiting effect when compared to CHX ADS. Both CHX and CHX ADS seemed to produce similar staining effect.
Conclusion
Effective plaque removal is very important to prevent any gingival/periodontal conditions. In our study the comparison between CHX and CHX ADS showed that CHX was more effective in reducing plaque formation than in comparison to CHX ADS. Hence, CHX is recommended for short term use as it is more efficacious but has the property of staining and CHX ADS can be used for long periods when the infections are not as severe or the oral hygiene levels are good.
References

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...