Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Research Article(ISSN: 2641-1687) 
Therapeutic Effect of Barley Grains powder (Hordeum vulgare L.) Among Sudanese Patients with Proteinuria Admitted at Ibn Sina Hospital in Khartoum State - Pilot study 2018 Volume 2 - Issue 5
Nahla A Khairy1, Ibrahim A Ali2*, Mohamed I Eisa3, Shihab Eldin S Dishean4 and Omer A Musa5
- 1Department of Physiology, Faculty of Medicine, Bayan college of Science and Technology, Sudan
- 2Department of Physiology, Faculty of Medicine, The National Ribat University, Sudan
- 3Department of Medicine, Faculty of Medicine, Sudan International University, Consultant Physician and Nephrologist and Director General , Ibn Sina Hospital, Sudan
- 4Department of Nephrology, Ibn Sina Hospital, Sudan
- 5Department of Physiology, Faculty of Medicine, The National Ribat University, Sudan
Received:April 03, 2020; Published: June 23, 2020
Corresponding author: Ibrahim A Ali, Department of Physiology, Faculty of Medicine, The National Ribat University, Sudan
DOI: 10.32474/JUNS.2020.02.000148
Abstract
Background: Proteinuria is very common in Glomerular diseases like membranous glomerulonephritis, focal segmental glomerulonephritis and minimal change disease. Severe proteinuria can cause nephrotic syndrome in which there is worsening swelling of the body. Barley grains were used to treat the proteinuria but not been recommended formally to be used.
Objectives: This study aimed to determine the effect of Barley grains powder (Hordeumvulgare L.) among Sudanese patients with Proteinuria admitted at Ibn Sina hospital in Khartoum state.
Methods: This is an analytical, cross-sectional hospital based study performed in Ibn Sina hospital in Khartoum state capital of Sudan during 2018-2019 in Sudanese patients above of age range (20 - 80 years old) who have documented renal impairment with significant proteinuria and have no extra renal cause of proteinuria. The patients were given barley for one week. In a dose of full tea glass of barely in three tea glasses of water (one tea glass equal 750 ml of water and 50 mg of barely). 24 hour’s urine and Blood samples for each patient was collected before and after barley administration and then the samples were sent to the laboratories for urinary protein estimation, serum albumin and renal functions test.
Results: The mean of urinary proteins before the barley administration was found to be 300.1389 mg/dl SD while the mean after barley administration was 248.74. With regards to 24 hours urine proteins; before intervention the mean was found to be 3.3934 g/day while the mean after intervention was 2.6433 g/day with significant p value (0.016). The level of serum albumin was found to be higher after administration of Barley with mean (2.6083 g/dl) compared to the mean after intervention (3.0500 g/dl) with significant p value 0.031.
Conclusion: Barley was found to be effective therapy for treatment of patients with proteinuria
Keywords: Barley; Proteinuria; Sudan
Introduction
A. Barley (Hordeumvulgare L.) is the world’s fourth most
important cereal crop after wheat, rice and maize [1]. It is readily
available with reasonable cost and has the highest amount of
dietary fiber among the cereals which may be beneficial for the
metabolic syndrome. Numerous studies showed that whole
grains containing a high amount of soluble fiber, such as oats, are more effective in lowering blood cholesterol than grains
containing predominantly insoluble fibers, such as wheat or
rice [2,3].
B. The US Food and Drug Administration Allows the health
claim statement that, depending on the β-glucan content,
consumption of soluble fiber from oats or psyllium in a diet
low in saturated fat and cholesterol may reduce the risk of
Coronary Vascular Disease (CVD) [4].
C. Proteinuria is presence of even relatively small amounts
of protein or albumin in the urine is an important early sign
of kidney disease and is a strong predictor of an increased risk
for cardiovascular mortality and morbidity in certain high-risk
groups within the general population [5].
D. The possibility that proteinuria may accelerate kidney
disease progression to end-stage renal failure has received
support from the results of increasing numbers of experimental
and clinical studies. Evidence indicating that this process
occurs through multiple pathways, including induction of
tubular chemokine expression and complement activation
that lead to inflammatory cell infiltration in the interstation
and sustained fibro genesis is reviewed [6].
E. Proteinuria is not only a well‐recognized sign of kidney
disease, but it is also an independent risk factor for the
progression of renal failure. Understanding the underlying
mechanisms and structural changes leading to a leaky
glomerular ‘barrier’ is therefore of outmost importance. In
the kidney glomeruli some 180 L of primary urine are filtered
daily from the plasma, with almost total exclusion of plasma
proteins of the size of albumin and larger. Morphologically the
filtration barrier consists of three layers: (a) the fenestrated
endothelium, (b) the glomerular basement membrane
(GBM) and (c) the podocytes (epithelial cells) with their
interdigitating foot processes that are separated by an ultrathin
slit diaphragm. The main macromolecular barrier function
was previously assigned to the GBM, but studies carried out
during the last few years have led to new findings showing that
the podocytes and their slit diaphragms actually have a central
role in retaining plasma proteins in the circulation [7].
F. Effect of Barley on lipids Long-term feeding studies
incorporating β-glucan have shown reductions in plasma
cholesterol in hypercholesterolemia men [4,8]. A diet low in
saturated fat and high in viscous polysaccharides, including
β-glucan, resulted in a 7.5% reduction of serum cholesterol
in hyperlipidemia men and affect other parameters of lipid
profile [9-13].
G. Barley leaves have also a high antioxidant activity that
might be useful in metabolic syndrome prevention or therapy,
as well as diseases caused by oxidative stress damage. This
property is mainly attributed to saponarin, a flavonoid with
potent antioxidant activity found in young green barley leaves
[11].
H. Barley is a rich source of magnesium, a mineral that acts
as a co-factor for more than 300 enzymes, including those
involved in glucose metabolism and insulin secretion. Barley
is also a very good source of fibers and selenium and a good
source of phosphorus and copper [14].
I. It was found that constant consumption of whole grains
decreased the risk of type II diabetes by 31%, pointing out
that whole grains extend special benefits in motivating healthy
blood sugar control [12]. According to Nilsson and coworkers,
eating whole grain barley by human can regulate blood sugar
for up to 10 h after consumption [15]. What seems to have
been responsible for barley’s effectiveness in regulating blood
glucose is probably its soluble fiber content [16].
J. Barley has been found to be a kidney-friendly and
diabetes-friendly food. It can help control diabetes and kidney
damages so as to help reduce high Creatinine levels to a
certain degree. The study aimed to investigate the potential
therapeutic effect of barley on Sudanese adult patients with
proteinuria admitted at Ibn Sina hospital in Khartoum State.
Materials and Methods
a. This was an analytical, cross-sectional hospital-based
study performed at Ibn Sina hospital in Khartoum state capital
of Sudan during 2018-2019 in Sudanese patients documented
to had renal impairment with significant proteinuria and have
no extra renal cause.
b. The patients who agreed to participate in the study were
interviewed. The objectives of the study were explained to all
individuals participating in the study. Written consent was
being obtained from all participants after fully explaining to
them the project.
c. An interview questionnaire was be filled by all volunteers
to obtain the data about age, address, occupation ,level of
education , medical history, family history , history of NSAIDs
and any other drugs use, marital status, smoking, lifestyle,
Weight, height, BMI and blood pressure, was measured with
standard techniques. All techniques and equipment were
standardized and performed twice (before and following
barley administration).
d. The sample was then convenient sample. The patients
were given barley for one week. In a dose of full tea glass of
barely in three tea glasses of water (one tea glass equal 750 ml
of water and 50 mg of barely).
e. 24 hour’s urine sample for each patient was collected before
and after barley administration and then the samples were
sent to the laboratories for protein estimation. Measurement
of a 24 hour urine sample was done by colorimetric method.
All study participants were provided a conventional 24-hour
urine container. For each study participant; two separate urine
collections were obtained. The first sample was taken with
conventional 24-hour urine collection instructions. For the
first sampling participants were asked to start urine collection
at 9 o’clock in the morning, after discarding first morning urine.
After that, entire volume of urine throughout the day collected
in the container to determine volume, and protein levels. Urine
protein levels were determined with the turbidimetric method
with the aid of benzethonium chloride.
f. Five ml of venous Blood sample was collected in EDTA
container for measurement of serum albumin and renal
functions test. Measurement of serum Creatinine was done
by biosystem 350 and mindary BS -200 using Jaffees reaction
(normal rang: serum Creatinine 0.1-1.5mg/dl). Measurement
of urea was done by colorimetric method using end-point
determination Urease – Berthelot Reaction (normal range:
urea=15-40mg/dl).
g. The study was approved by the research ethics committee
of the Faculty of Medicine, The National Ribat University and
ethical approval was taken from Ibn Sina Hospital.
h. The collected data was analyzed using SPSS (Statistical
Package for Social Sciences), Version 25, (T-test for mean and
P value for significance). P value ≤ 0.05 will be statistically
significant.
Results
A. The study covered twenty Sudanese adult patients
admitted at Ibn Sina hospital in Khartoum state. The patients
were known to be suffering from proteinuria [16]. of
participants were males and [4] were females and their age
were ranging between (20-80) years old. 20% of them were
between (20 and 40) years old,65% of them were between (40
and 60) years and the other 15% were between (60 and 80)
years.
B. 80% [16] of the patients were males and 20% [4] were
females.
C. In the majority of patients, the renal problems that caused
the proteinuria was nephrotic syndrome such as membranous
glomerulonephritis, focal segmental glomerulonephritis and
minimal change disease.
D. There was a positive family history of diabetes and
hypertension in 65% and 35% of patients respectively.
E. In regard to BMI among the group the majority were
found to be within the normal category while 10% were under
weight and only 5% were obese.
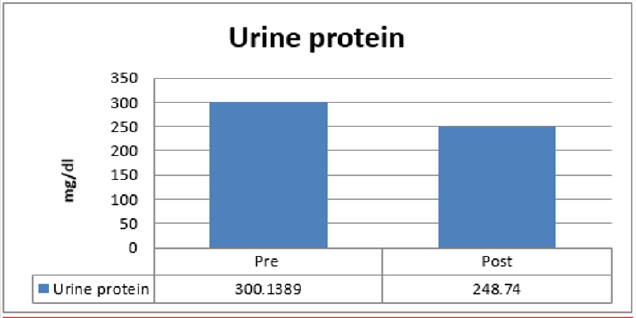
F. The mean of urinary proteins before intervention
was found to be 300.1389 mg/dl SD while the mean after
intervention was 248.74 (Figure 1).
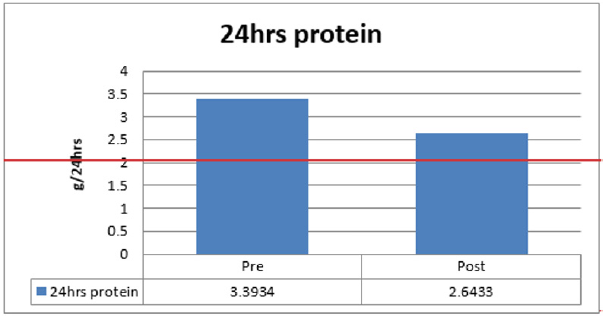
G. With regards to 24 hours urine proteins; before
intervention the mean was found to be 3.3934 g/day while the
mean after intervention was 2.6433 g/day with significant p
value (0.016) (Figure 2).
H. When protein is evaluated by number of crosses it was
found that the average before intervention was 2.9 crosses
while after intervention was 1.9 (similarly significant to the
result of mg/ dl).
I. The level of serum albumin was found to be higher after
administration of Barley with mean (2.6083 g/dl) compared
to the mean after intervention (3.0500 g/dl) with significant p
value 0.031 (Table 1).
Table 1: Tests Correlations (Paired Samples Statistics) pre and post barley administration.
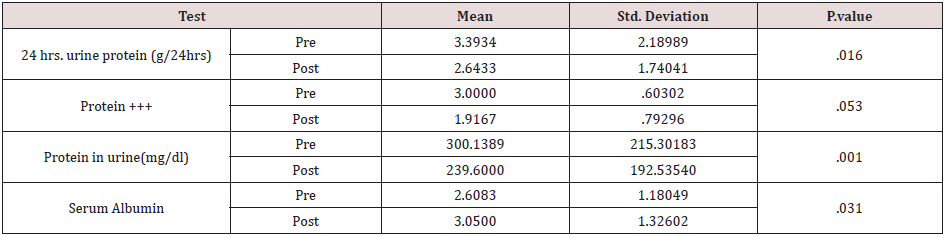
• T-test p-value less than 0.05 is considered statistically significant.
• T-test p-value more than 0.05 is considered statistically insignificant.
Discussion
A. This study aimed to know the effect of Barlay on protein
in urine where we found the use of Barlay for a weak working
on the decrease of protein in the urine. There is no similar
previous data studying the effect of barley on proteinuria.
B. We found most of the Patients (65%) suffering from
proteinuria between the ages of 20-40 and the numbers of
men were four times that of woman.
C. Regardless to causation, the association between
administration of barley and reduction in proteinuria was
significant P value (0.016) but it was not accompanied by
significant change in urine volume (insignificant P value 0.90).
D. This may raise the question the need for further study to
confirm the effect of barley in reduction of protein in the urine.
The study also showed a positive effect in all age group. So,
these indicate barley could be safely administered to all age.
E. With regard to gender; male showed significant response
than female. This also raised a question of the relationship of
gender response in association with barley administration
specially a lack of literature in this issue.
Conclusion
Admission of barely to patients with renal disease is found to be associated with reduction of protein in urine as well as increase in serum albumin.
References
- National Cholesterol Education Program (NCEP) (2002) Third Report of the NCEP Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). National Heart Lung and Blood Institute pp. 1–284.
- William F Keane, Garabed Eknoyan, MD for the Committee (1999) Proteinuria, albuminuria, risk, assessment, detection, elimination (PARADE): A position paper of the National Kidney Foundation. AKD 33(5): P1004-1010.
- Mauro Abbate, Carla Zoja, Giuseppe Remuzzi (2006) How Does Proteinuria Cause Progressive Renal Damage? JASN 17 (11): 2974-2984.
- K Tryggvason, E Pettersson (2003) Causes and consequences of proteinuria: the kidney filtration barrier and progressive renal failure. J Intern Med 254: 216–224.
- Anderson JW, Tietyen-Clark J (1986) Dietary fiber: Hyperlipidemia, hypertension and coronary heart disease. Am J Gastroenterol 81 (10): 907–919.
- Kritchevsky D (1987) Dietary fiber and lipid metabolism. Int J Obes 11(1): S33–S43.
- Oscarsson M, Andersson R, Aman P (1998) Effects of cultivar, nitrogen fertilization rate and environment on yield and grain quality of barley. J Sci Food Agric 78: 359–366.
- Van Horn LV, Parker D (1986) Serum lipid response to oat product intake with a fat-modified diet. J Am Diet Assoc 86(6): 759–764.
- Gold KV, Davidson DM (1988) Oat bran as a cholesterol-reducing dietary adjunct in a young, healthy population. West J Med 148(3): 299–302.
- Anderson JW, Story L, Sieling B (1984) Hypocholesterolemic effect of oat-bran or bean intake for hypercholesterolemic men. Am J Clin Nutr 40(6): 1146–1155.
- Prentice N, Qureshi AA, Burger WC, Elson CE (1982) Response of hepatic cholesterol, fatty acid synthesis and activities of related enzymes to rolled barley and oats in chickens. Nutr Rep Int 26(4): 597–604.
- Qureshi AA, Burger WC, Elson CE, Benevenga NJ (1982) Effects of cereals and culture filtrate of Trichodermaviride on lipid metabolism of swine. Lipids 17(12): 924–934.
- Newman RK, Lewis SE, Newman CW, Boik RJ (1989) Hypocholesterolemic effect of barley foods on healthy man. Nutr Rep Int 39: 749–760.
- Schneeman BO (1998) Dietary fiber and gastrointestinal function. Nutr Res 18(4): 625–632.
- Lia A, Hallmans G, Sandberg AS (1995) Oat beta-glucan increases bile acid excretion and a fiber-rich barley fraction increases cholesterol excretion in ileostomy subjects. Am J ClinNutr 62(6): 1245–1251.
- Marlett JA (1997) Sites and mechanism for the hypocholesterolemic actions of soluble dietary fiber sources. AdvExp Med Biol 427: 109–121.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...