Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Case Report(ISSN: 2641-1687) 
Primary Carcinoid of the Kidney- A Rare Case of An Asymptomatic Abdominal Mass Volume 2 - Issue 1
Suraj Hegde1, Amulya Cherukumudi2*, Rajeev T P3 and Narendra Pai4
- 1Associate Professor, Department of Urology, KS Hegde Medical Academy, Mangalore, India
- 2Junior Resident, Department of General Surgery, KS Hedge Medical Academy, Mangalore, India
- 3Professor and Head, Department of Urology, KS Hedge Medical Academy, Mangalore, India
- 4Assistant Professor, Department of Urology, KS Hedge Medical Academy, Mangalore, India
Received: June 06, 2019; Published: June 13, 2019
Corresponding author: Amulya Cherukumudi, Junior Resident, Department of General Surgery, KS Hegde Medical Academy, Mangalore, India
DOI: 10.32474/JUNS.2019.02.000127
Abstract
Carcinoid tumors originate from neuroendocrine cells and have an indolent course. Primary carcinoid of the kidney is rare, as renal parenchyma is lacking in the enterochromaffin cells. The aetiopathogenesis is not properly understood as there are very few cases. There are several tests that can be performed pre-operatively, with octreotide scintigraphy being specific. Histopathology helps confirm the diagnosis, and this is further supplemented by immunohistochemistry. IHC stains positive for cytokeratin and synaptophysin in case of carcinoid tumors. While medical treatment helps manage the syndromes that maybe associated with a carcinoid tumor, surgery remains the treatment of choice. These tumors have a low malignant potential, and post-operative chemoradiotherapy is often not indicated. Here we present a case of a middle-aged female with an incidentally detected carcinoid of the kidney. Post-surgery, she remains asymptomatic and has not shown any signs of recurrence thus far.
Keywords: Primary Carcinoid; Renal Parenchyma; Neuroendocrine; Immunohistochemistry
Introduction
Carcinoid tumors arise from the neuroendocrine cells and are usually low-grade in nature. These are predominantly located in the gastrointestinal tract and tracheobronchial tree and liver. However, primary carcinoid of the kidney is rare in occurrence, with less than 100 cases being reported in published literature. They are known to be slow growing in comparison with renal cell carcinoma; however, they are known to metastasize to draining lymph nodes, bones and liver. Imaging by contrast enhanced computed tomography of the abdomen helps in identifying the lesion; however, histopathology is confirmatory for the same. Immunohistochemistry markers are performed on the histopathological specimen to confirm that it is a carcinoid tumor. Surgical treatment in the form of partial nephrectomy or radial nephrectomy is considered the treatment of choice, with good post-operative outcomes. However, regular follow up is necessary to look for any recurrence or metastasis. Here we present a unique case of a middle-aged female with carcinoid of the left kidney.
Case Report
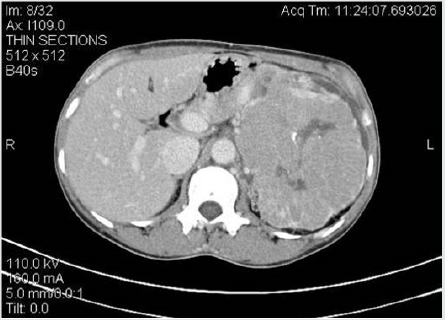
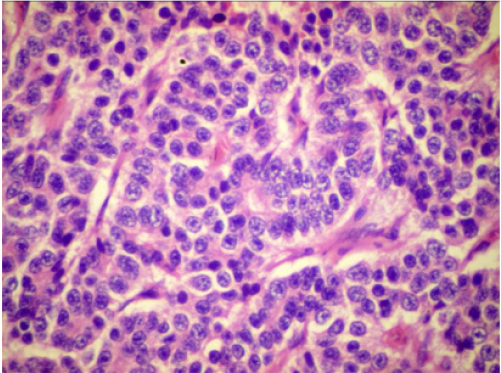
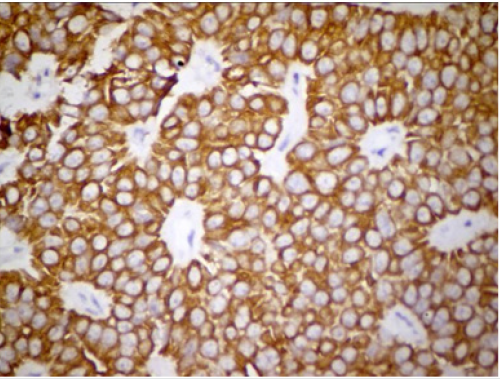
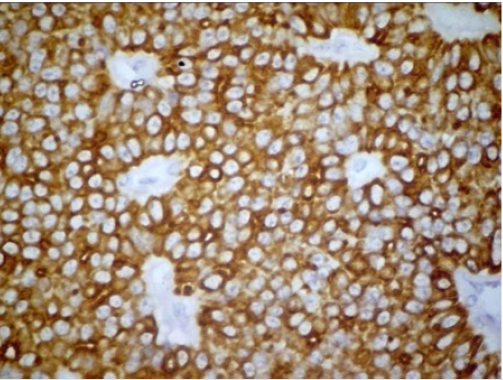
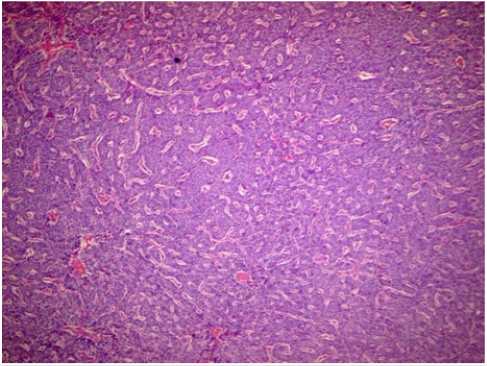
A 46-year-old female patient presented to our Urology OPD with left dull aching flank pain intermittently since five years along with a swelling in the left flank since two months. She had no other gastrointestinal or urinary complaints, and had no history of anorexia, fatigue, weight loss, backache or bony pain. The patient was known hypertensive, being managed with single pharmacological agent. On examination, abdomen was soft and non-tender with an 8x6 cm mass palpable in left hypochondrium extending to lumbar region, which moved with respiration, was bimanually palpable and ballotable. There was no renal angle tenderness or fullness noted on the right side. The rest of the systemic examination was appropriate for the age of the age of patient. The patient was then evaluated extensively to identify the nature of the mass. Routine blood investigations were done, reports of which were normal with Serum creatinine being 0.9 mg/dL. USG Abdomen and pelvis was done, which revealed a heteroechoic lesion of size 15x 4 cm in Left Kidney. To confirm the diagnosis, CECT Abdomen and Pelvis was done, which revealed a large mass measuring 12.5x8.8x15 cm, heterogeneously enhancing with calcifications in retroperitoneum on left side with internal non enhancing low density areas in upper half of anterior part of Left Kidney (Figure 1). It was noted that the Left adrenal gland not visible separately from the mass and the interface between mass and adjacent renal parenchyma is more or less well defined, extending to left renal hilum with no obvious obstruction of renal pelvis. The lower half of Left kidney was reported to be normal with compression, but not extension, of the left renal vein or inferior vena cava. The mass was found to be pushing pancreas, splenic vein forward, displacing stomach, abutting spleen, aorta and left psoas muscle (Figure 2). For the above-mentioned lesion, the patient underwent left open nephrectomy under general anesthesia. A left 11th rib cutting, flank incision was made, and the left kidney was accessed via a Transperitoneal approach. Intraoperatively, there was a 15x10 cm mass palpable in the upper part of left kidney with multiple collaterals. The left adrenal gland, however, appeared to be normal and seemingly uninvolved. There was no evidence of enlarged lymph nodes along the draining lymphatics. Histopathology of the left renal mass revealed a well-differentiated neuroendocrine tumor with eosinophilic trabeculae intermixed with nests of small, monotonous, cuboidal tumor cells consistent with carcinoid tumor (Figures 3 & 4). Immunohistochemistry markers were done on the histopathological specimen, which was found to be positive for Cytokeratin and Synaptophysin, while being negative for CD 99 (Figures 5 & 6).Post-operative period was uneventful in this patient, with removal of the abdominal drain on POD 3, and was discharged on POD 6. Patient came for follow up after 2 weeks, and there was no evidence of surgical site infection. Patient came back after 3 months, and a repeat CECT abdomen was done, which showed no evidence of residual tumor or recurrence.
Figure 2: CECT abdomen and pelvis showing left renal mass displacing stomach, abutting the spleen, aorta and left psoas muscle.
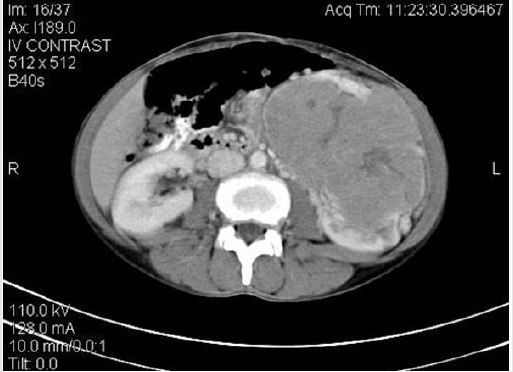
Figure 3: Hematoxylin and eosin staining- microscopy (low power view) showing well differentiated neuroendocrine tumor with cells in nests and clusters with eosinophilic trabeculae.
Discussion
Carcinoid tumors are indolent neuroendocrine tumors, with low grade malignant potential found usually in the gastrointestinal tract, tracheobronchial tree, and liver etc., but rare in the genitourinary tract. There are less than 100 cases reported in English literature [1]. They arise from the enterochromaffin cells or APUD cells, located predominantly in the bladder trigone, ureter, renal pelvis and prostate, but not in the renal parenchyma. It is suggested that there may be trapping of the neural crest cells within the developing metanephros or due to the present of totipotent cells within the renal parenchyma. This could also be due to metaplasia of the pyelocaliceal urothelium secondary to chronic inflammation or due to metastasis from an occult primary tumor [2]. Carcinoid tumors are found to have an association with horseshoe kidney with an incidence of 17.8% of the reported cases [1,2]. Certain case reports have shown association of renal carcinoid with renal dysplasia and teratomas, indicating an aberration of differentiation of cells during embryological development [3,4]. These tumors are not clinically apparent, often discovered on routine abdominal scans. They have an indolent course, are slow growing and seldom manifest with symptoms of vague abdominal pain or flank pain, constipation, fever or visible/ palpable abdominal mass. Apart from the symptoms related to the abdominal mass and its pressure effect on the surrounding structures, there can be symptoms due to the production of active hormones in circulation [5,6]. The most common of these is carcinoid syndrome (secretion of excess of serotonin), consisting of flushing, diarrhea and bronchoconstriction etc. the other associated symptoms are Glucagon induced constipation, Cushing syndrome, Verner Morrison Syndrome and Zollinger Ellison syndrome. There are several laboratory tests available for the identification of neuroendocrine secretory products in the serum or urine. This is 24 hour urinary 5-HIAA (5-hydroxyindoleactic acid) and serum chromogranin A. Radiologically, it has minimal to poor enhancement on contrast enhanced computed tomography, correlating with the lack of vascularity in such lesions on renal angiography. Octreotide Scintigraphy is a sensitive and specific imaging method for carcinoid tumors, especially in those with elevated serum serotonin [7,8]. Carcinoid tumors are usually positive for Cytokeratin (broad spectrum and low molecular weight) and Synaptophysin on Immunohistochemical staining. Other markers that show positive staining for carcinoids are neuron-specific enolase, chromogranin and Leu-7. While medical management has been attempted in such cases to manage symptoms, surgical excision remains the treatment of choice for carcinoid tumors. Since carcinoid tumors are indolent and have low malignant potential, there remains a role for Nephron sparing surgery in such cases; unless the mass is occupying the entire kidney [9]. However, for this, there must be a strong clinical suspicion of a carcinoid tumor pre-operatively. With the advancement of immunohistochemistry, there are several markers that can be applied on the histopathological specimen. Since these tumors are slow growing, regular imaging after surgery might be sufficient. The prognosis is considered to be favorable even in the setting of a horseshoe kidney, considering there is a higher predominance of the same. However, since there are such few cases reported in published literature, the epidemiological details and overall disease survival is unknown, and hence, the management remains to be a challenge.
Conclusion
Primary renal carcinoids are rare tumors originating from the neuroendocrine cells. Surgery remains the treatment of choice, and immunohistochemistry is used to confirm the diagnosis. Further studies are required to assess the treatment options and follow-up protocols for the same.
Acknowledgement
I would like to thank the department of Urology for the opportunity provided to draft this case report.
References
- Raslan WF, Ro JY, Ordonez NG (1993) Primary carcinoid of the kidney: immunohistochemical and ultrastructural studies of five patients. Cancer 72: 2660-2666.
- Di Sant Agnese PA (1998) Neuroendocrine cells of the prostate and neuroendocrine differentiation in prostatic carcinoma: a review of morphologic aspects. Urology 51(suppl 5A): 121-124.
- Di Sant Agnese PA, Cockett ATK (1994) The prostatic endocrine-paracrine (neuroendocrine) regulatory system and neuroendocrine differentiation in prostatic carcinoma: a review and future directions in basic research. J Urol 152: 1927-1931.
- Capella C, Usellini L, Buffa R, Frigerio B, Solcia E (1981) The endocrine component of prostatic carcinomas, mixed adenocarcinoma-carcinoid tumours and nontumour prostate: histochemical and ultrastructural identification of the endocrine cells. Histopathology 5: 175-192.
- Resnick ME, Unterberger H, McLoughlin PT (1966) Renal carcinoid producing the carcinoid syndrome. Med Times 94: 895-896.
- Isobe H, Takashima H, Higashi N (2000) Primary carcinoid tumor in a horseshoe kidney. Int J Urol 7: 184-188.
- Begin LR, Guy L, Jacobson SA, Aprikian AG (1998) Renal carcinoid and horseshoe kidney: a frequent association of two rare entities-a case report and review of the literature. J Surg Oncol 68: 113-119.
- Krishnan B, Truong LD, Saleh G (1997) Horseshoe kidney is associated with an increased relative risk of primary renal carcinoid tumor. J Urol 157: 2059-2066.
- Kawajiri H, Onosa N, Ohira M (2004) Carcinoid tumor of the kidney presenting as a large abdominal mass: report of a case. Surg Today 34: 86-89.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...