Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2641-1687
Case report(ISSN: 2641-1687) 
What do we know about Treatment of Post-Circumcision Penile Ischemia. Case report and Review of Literature Volume 4 - Issue 3
kopytek Weronika*, Sassine Antoine, Schulman Claude, Cogan Elie, Chatzopoulos Charles
- Department of Urology, DELTA Hospital, CHIREC Brussels, Belgium
Received: May 15, 2023; Published: May 31, 2023
Corresponding author: Kopytek Weronika, Department of Urology, DELTA Hospital, CHIREC Brussels, Belgium
DOI: 10.32474/JUNS.2023.04.000189
Abstract
Circumcision for therapeutic and non-therapeutic purposes is one of the most frequently performed male procedures worldwide in all age groups. In order to decrease post-operative pain dorsal penile block (DPNB) with a long-acting (bupivacaine) or intermediate-acting (lidocaine or mepivacaine) agent is the most common anaesthesia technique. Although circumcision remains a quick and simple procedure, it is not without risk, with complications rate from 1 to 4%. Penile ischemia is a rare but severe complication of circumcision that can lead to irreversible necrosis of the glans. The causal mechanisms remain unclear although several hypotheses have been suggested including, such as the use of vasoconstricting agents in local anaesthesia, arterial vasospasm due to needle microtrauma during dorsal penile nerve block (DPNB), hematoma, blood vessel binding, excessive use of monopolar cautery, a tight suture line, and/or a tight bandage applied to the circumcised area. Various therapeutic options were proposed, but so far there are no treatment guidelines. We report the case of a 10-year-old boy with penile ischemia after circumcision that resolved spontaneously after one month and present a current review of 23 other published cases.
Keywords: Penile ischemia; dorsal penile nerve block; hematoma; blood vessel binding
Introduction
Circumcision for therapeutic and non-therapeutic purposes is one of the most frequently performed male procedures worldwide in all age groups [1]. In order to decrease post-operative pain dorsal penile block (DPNB) with a long-acting (bupivacaine) or intermediate-acting (lidocaine or mepivacaine) agent is the most common anaesthesia technique [2-4]. Although circumcision remains a quick and simple procedure, it is not without risk, with complications rate from 1 to 4% [5]. Penile ischemia is a rare but severe complication of circumcision that can lead to irreversible necrosis of the glans. The causal mechanisms remain unclear although several hypotheses have been suggested including, such as the use of vasoconstricting agents in local anaesthesia, arterial vasospasm due to needle microtrauma during dorsal penile nerve block (DPNB), hematoma, blood vessel binding, excessive use of monopolar cautery, a tight suture line, and/or a tight bandage applied to the circumcised area [6]. Various therapeutic options were proposed, but so far there are no treatment guidelines [7]. We report the case of a 10-year-old boy with penile ischemia after circumcision that resolved spontaneously after one month and present a current review of 23 other published cases.
Case Report
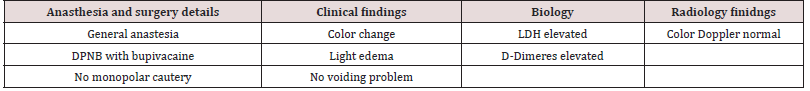
We present the case of a 10-year-old boy admitted for elective circumcision after recurrent balanitis and phimosis. The intervention was performed under general anaesthesia, including sevoflurane 4% O2/N2O 50/50 administered via mask. The technique of dorsal penile nerve block with bupivacaine 0.5% in 4 ml was used in order to decrease post-operative pain. The intervention lasted 16 minutes and was uneventful. The patient was sent home the same day. The day after parents called the surgeon to report the dark color of the glans. Physical examination showed a very dark necrotic appearance of the glans and light edema around the suture site (Figures 1A & 1B). No suggestive signs of infection were noted, and voiding function was normal. D-dimeres (1,23 microg/ mL*; 0,5 microg/mL) and LDH (242 U/L; norm 135-225) levels were slightly elevated in a blood test. The color Doppler ultrasound examination showed normal permeability of the penile arteries and no abnormalities of vascularization. We thus decided to adopt a conservative attitude. Clear improvement was noticed after a few days with normalization of the color of the glans (Figures 2A & 2B) with the complete normalization one month after the intervention.
Figure 1: Physical examination showed a very dark necrotic appearance of the glans and light edema around the suture site.
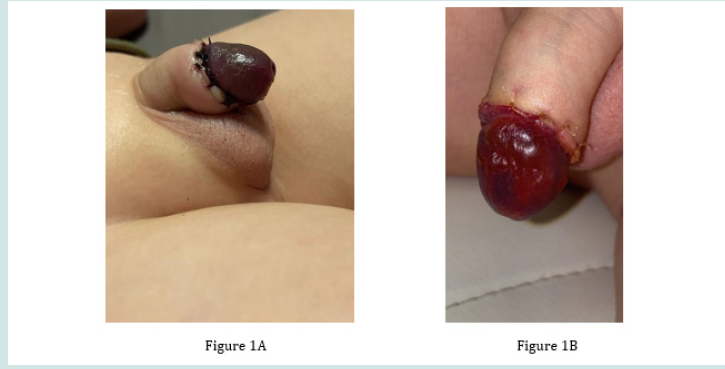
Figure 2: Clear improvement was noticed after few days with normalization of the color of the glans with the complete normalization one month after the intervention.
Discussion and review of literature
As penile ischemia can cause irreversible damage to the glans, the choice of the best treatment is of crucial importance. However, since no vascular anomaly had been demonstrated in our patient, we opted for a conservative attitude which was followed by a complete spontaneous resolution of the penile ischemia. In our case, we decided to choose conservative treatment as there was no vascular deficit that resulted in complete recovery of the glans. To the best of our knowledge, this is the fifth case described as being resolved spontaneously without any additional therapeutic methods. The cause of penile ischemia in our case remains unclear, as the color doppler ultrasound was normal, no adrenaline or other irritative agent was used, the volume of local anaesthesia was adequate to the body mass of the patient, and no monopolar cautery was used. We could also exclude penile ischemia due to tightened sutures, as it resolved spontaneously without any re-intervention. The penile ischemia post circumcision is in the first hypothesis secondary to the local anaesthesia technique, type of product used, and/or volume of solution injected. The dorsal penile nerve block is the technique of choice for analgesia in circumcision as it is easy to perform and a safe procedure with a low complication rate of 0.18% [8]. Numerous authors cited the DPNB technique as a cause of penile ischemia due to endothelium damage caused by needle introduction and induction vasospasm of penile vessels [9].
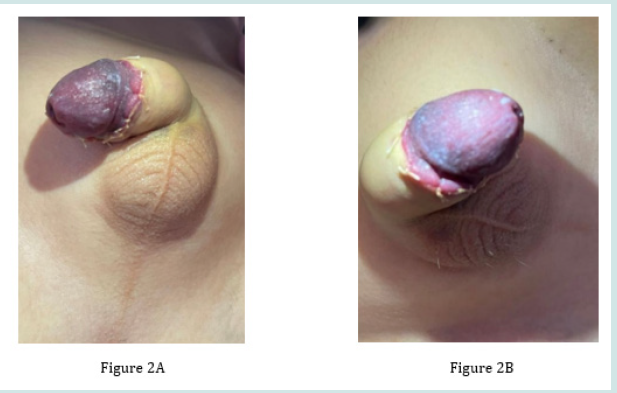
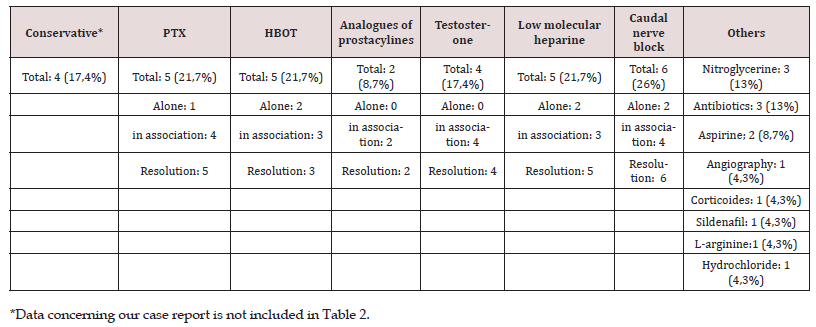
Table 1A & 1B contain data concerning anaesthesia and surgical procedures. The most frequently used agents for DPNB are lidocaine, bupivacaine, and mepivacaine, whereas the use of ropivacaine is controversial as it possesses intrinsic vasoconstrictive action, especially at low doses [10,11]. The following solutions were used for local analgesia in the cases studied: lidocaine, bupivacaine, mepivacaine, xylocaine, ropivacaine, and carbocaine. According to Sara and Lowry, the volume of solution alone cannot be responsible for vessel compression and damage that may provoke penile ischemia [12]. However, the discussion about the molecule used for local anaesthesia remains unanswered. Some considered that using a vasoconstrictor is contraindicated for anesthesia of extremities with terminal vascularization but remains a controversial issue. Only three of the 23 cases described in this review used a vasoconstrictor such as adrenaline for local analgesia [13,14]. Other potential causes of penile ischemia were tight sutures or too tight banding after intervention. Other hypotheses included concomitant use of an irritative substance such as thiopental or excessive use of monopolar cautery with an electrical current carried by the small diameter of the penis, which may lead to thermal injury [15].
Table 1: Numerical values denote the overall incidence of this element in data collected from literature.
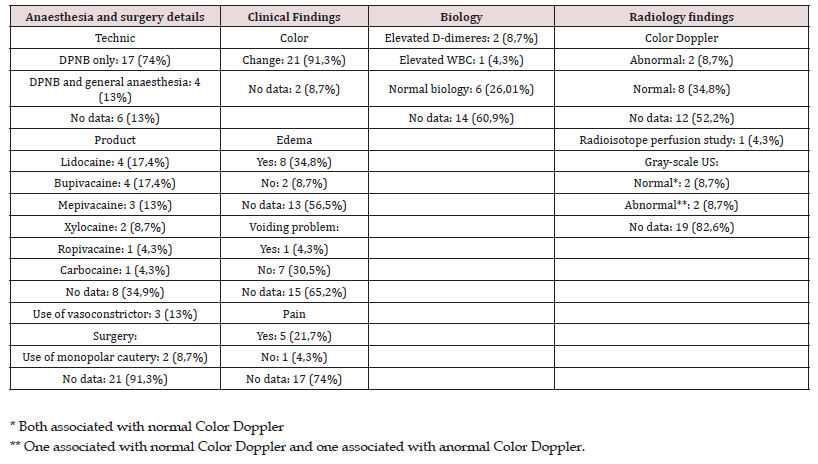
Table 1A & 1B integrates the clinical data and procedures used. (Details of individual cases are shown in Supplemental Table 1). Median age is 7 years (range from 13 days to 33 years), with only four patients over the age of 18. In 14 cases, the first symptoms were noticed less than 24 hours after surgery, in 6 cases between 48 hours and one-week post-operation, in two cases there is no data about the time of apparition [16,17], and in one case estimation was difficult because of the delay between observation of the symptoms and admission to the hospital. A clinical exam with signs of abnormal penile perfusion, such as dark color of the glans, acute pain, or flaccidity of the penis, is used to diagnose penile ischemia. However, not all of the patients were in pain or had penile edema; therefore, all of them presented pale or dark penile glans. No infection signs were detected, and voiding difficulty was described only in one case [18]. The most frequently performed additional exams were blood tests (D-dimeres, clotting profile, white blood cells, protein S and C, fibrinogen), and color-doppler of penile arteries. In 8 cases, there is no information concerning additional exams. However, the blood tests were within the normal range in most of the cases. D-dimeres were elevated in two cases, WBC were elevated in one, and LDH and D-dimeres were elevated in our case.
The results of the color doppler were mostly normal, except for one case. Gray-scale ultrasound was conducted in four cases, and in two of them, it revealed unexpected thickening and echogenicity of the surface of the glans penis, indicating more than simple edema. As a consequence, in those two cases, a diagnosis of superficial ischemia was proposed. Although the first case of postcircumcision penile ischemia was described in 1981 by Sterenberg et al., nowadays there are still no guidelines for optimal treatment of this rare complication. Nevertheless, the main objective of the treatment is to restore sufficient blood flow and oxygen delivery to ischemic tissue in the glans [19]. Hyperbaric oxygen therapy (HBOT), topical 10% testosterone undecanoate, intravenous or oral pentoxifylline (PTX), low-molecular-weight heparin (enoxaparin), intracavernous glycerol trinitrate and bupivacaine, intravenous infusions of prostaglandin analogues, antiplatelets, corticosteroids, nitroglycerol, antibiotics, surgical review and caudal nerve block. In our case, as in four others, treatment remained conservative, and evolution was favourable and led to complete resolution. In those cases, a comparison of patient data was conducted. Results showed that the age range of patients varied from 10 days to 10 years. In this study, the type of anaesthesia administered varied among the cases. In two cases, general anaesthesia with DPN with bupivacaine was used. In another case, lidocaine with epinephrine was administered, while information regarding the type of anaesthesia used in two other cases was not available. The precise time of the clinical apparition was not available in most cases.
After 24 hours, it was noticed in our case as well as another. In this review, it was observed that all patients were presented with a change in the color of their glans. Additionally, one patient exhibited a blister on the skin of their penile corpus. The lack of commonalities among those five cases makes it challenging to determine whether there was a specific reason for their spontaneous resolution. Pentoxifylline (PTX) is a non-selective PDE inhibitor used as a hemorheological agent that improves peripheral blood flow and decreases blood viscosity. PTX was chosen as a therapeutic option in 5 cases; in one case it was used alone [20], and in four other it was combined with other treatments such block or topical testosterone, nitroglycerin, HBOT and antibiotics, caudal block, topic treatment with nitroglycerin and antibiotics. In one case, administration of the combination of PTX and HBOT was preceded by an intracavernous injection of another phosphodiesterase inhibitor, papaverine, that showed immediate improvement of the glans condition and led to complete resolution of penile ischemia in 7 days [21]; Sildenafil is a selective inhibitor of 5-phosphodiesterase and was administered orally in one case in addition to intravenous L-arginine hydrochloride with unfractionated heparin following caudal epidural bloc, angiography with intraarterial injection of alprostadil and nitroglycerin [22] (Table 2).
Table 3: Treatment. Numeric values indicate the frequency of therapy administration in cases described in literature review.
Hyperbaric oxygen therapy raises the partial pressure of oxygen, improving oxygenation of ischemic tissues as well as increasing levels of growth factors, cytokines, and hormones via the intermediates of reactive oxygen and nitrogen, leading to neoangiogensis and healing of post-ischemic tissues. HBOT was chosen as the sole treatment in two cases, but the outcome was unsatisfactory due to the severe burn injury caused by monopolar electrocautery in one case, and plastic reconstruction was required in the other. However, in the case of this 13-day-old boy, first-line treatment was conservative, and de HBOT was administered only two days after the onset of penile necrosis [23]. In three cases HBOT was combined therapy with other therapeutic and was followed by complete resolution. Iloprost and alprostadil are analogues, respectively, of prostacyclin PGI2 and PGE1, whose actions consist of inhibition of platelet aggregation and vascular smooth muscle relaxation [24]. This method was used twice in combination with other therapy and lead do complete resolution. Testosterone is known for its potential beneficial impact on endothelial cells and vascular endothelial growth factor expression that leads to improvement of the penile blood supply and revascularization of the glans. In four cases this method in combination with other methods led to complete resolution. Anticoagulant therapy with low-molecular-weight heparin alone or in combination was used successfully in 5 cases.
proposed LMWH as a first-line treatment, especially in cases of elevated D-dimeres, as enoxaparin is a safe anticoagulant in primary prophylaxis and the treatment of thromboembolism in pediatrics. The effectiveness of using the caudal bloc alone to decrease sympathetic tone and enhance arterial supply was demonstrated successfully by Kaplanian et al. and Berenes. In four other cases association with other therapy led to complete resolution of the ischemia of the glans. Additional therapeutic solutions were surgical revision, antibiotics, nitroglycerine, acetylic acid, and corticoids. In four cases, surgical revision was done with restoration of the sutures, and in one case, digital subtraction angiography was performed. Nitroglycerine was used as a spasmolytic agent during digital subtraction angiography, as a topic, and as an intracavernous injection in addition to other therapeutic methods. Although in all cases neither clinical nor biological signs of infection were detected and the use of antibiotics was not necessary in most of the cases, in three of them topical gentamicin, oral levofloxacin, or amoxicillin with clavulanic acid were administered. Acetylic acid was used in addition to other therapeutic methods in two cases [25,26], and corticoids were used in one case. Out of 23 cases, 21 were managed successfully and led to complete resolution of penile ischemia, independent of the method that was chosen. In the two remaining cases treated ineffectively by HBOT, the possible causes of failure were delay of admission and severe thermal injury during circumcision.
Conclusions
In this review, we analyzed 23 heterogeneous cases in terms of age, circumcision technique, anaesthetic technique, delay of apparition, and delay of admission, therapeutic method. All details are contained in Table 3. As a consequence, it is difficult to make an association between therapeutic methods and their impact, as the outcome is probably multifactorial. Penile ischemia is an organ-threatening condition, and many practitioners did not take the risk to choose conservative treatment, it may be justified to limit therapeutic methods and avoid overtreatment. As mentioned, caudal block, PTX, and heparin infusion separately led to complete resolution in 5 cases, and in 3 other cases, recovery was obtained without any treatment. However, use of a vasoconstrictor in local anaesthesia is controversial and was mentioned as a potential explanation of penile ischemia; therefore, a vasoconstrictor agent was used only in three cases, so probably it is not the main cause of this condition.
Table 4: 23 heterogeneous cases in terms of age, circumcision technique, anaesthetic technique, delay of apparition, and delay of admission, therapeutic method.
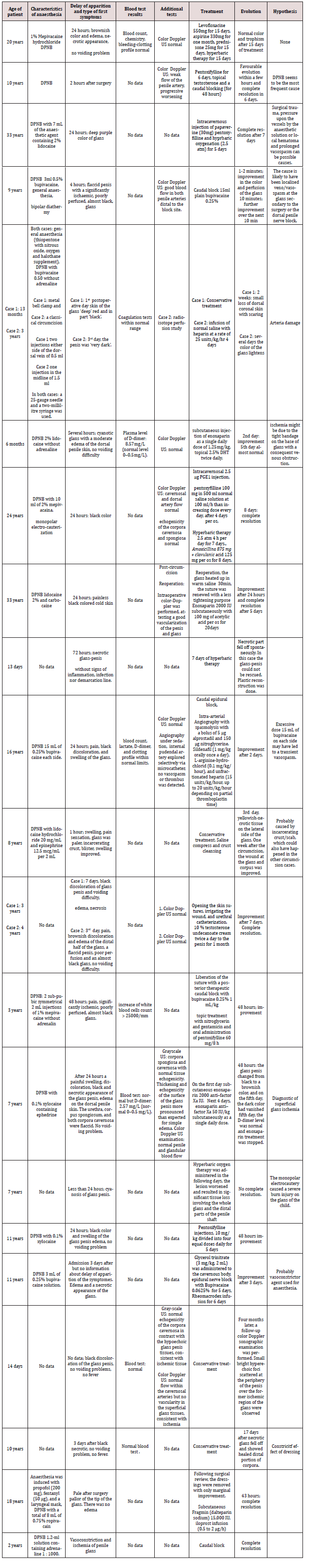
However, color doppler showed anormal blood flow only in one case, blood tests showed increased D-dimer and WBC only in three cases, and greyscale US was performed only in two cases, revealing signs of superficial ischemia; therefore, in eight cases out of 23, there was no information about complementary tests. As a consequence, we suggest doing color doppler, grayscale US, and blood tests with D-dimers and WBC in all patients with clinical suspicion of postcircumcision penile ischemia, as we need more data in order to conclude the pathogenesis and elaborate the therapy protocol. For future cases, it is essential to determine the precise volume and type of solution used for anaesthesia, the delay of the apparition of the symptoms, and the delay between the beginning of the treatment and clinical improvement in order to establish the protocol to follow in post-circumcision penile ischemia. In order to minimize the risk, we recommend avoiding the use of vasoconstrictive agents when performing a dorsal penile nerve block, preferring bipolar cautery during surgery, and not using a postoperative bandage.
References
- Miernik A, Hager S, Frankenschmidt A (2011) Complete removal of the foreskin--why? Urol Int 86(4): 383-387.
- Rossi S, Buonocore G, Bellieni CV (2021) Management of pain in newborn circumcision: a systematic review. Eur J Pediatr 180(1): 13-20.
- Gunter JB (2002) Benefit and risks of local anesthetics in infants and children. Paediatr Drugs 4(10): 649-672.
- Palinrungi MA, Palinrungi ALR, Christeven R, Faruk M (2021) Penile Ischemia as a Complication of Epinephrine Use in Penile Nerve Block: Truth or Myth? Res Rep Urol 13: 553-555.
- Prabhakaran S, Ljuhar D, Coleman R, Nataraja RM (2018) Circumcision in the paediatric patient: A review of indications, technique and complications. J Paediatr Child Health 54(12): 1299-1307.
- Migliorini F, Bianconi F, Bizzotto L, Porcaro AB, Artibani W (2018) Acute Ischemia of the Glans Penis after Circumcision Treated with Hyperbaric Therapy and Pentoxifylline: Case Report and Revision of the Literature. Urol Int 100(3): 361-363.
- Zvizdic Z, Anic D, Popovic N, Vranic S (2020) Acute glans ischemia after circumcision successfully treated with low-molecular-weight heparin and topical dihydrotestosterone: A case report. Medicine (Baltimore) 99(29): e21340.
- Kaplanian S, Chambers NA, Forsyth I (2007) Caudal anaesthesia as a treatment for penile ischaemia following circumcision. Anaesthesia 62(7): 741-743.
- Cárdenas Elías MÁ, Vázquez Rueda F, Jiménez Crespo V, Siu Uribe A, Murcia Pascual FJ, et al. (2016) [An unexpected complication: glans ischemia after circumcision. Review of the literature]. Cir Pediatr 29(3): 127-130.
- Garrido-Abad P, Suárez-Fonseca C (2015) Glans ischemia after circumcision and dorsal penile nerve block: Case report and review of the literature. Urol Ann 7(4): 541-543.
- D Burke, V Joypaul, MF Thomson (2000) Circumcision supplemented by dorsal penile nerve block with 0.75% ropivacaine: a complication. Reg Anesth Pain Med 25(4): 424-427.
- Sara CA, Lowry CJ (1985) A complication of circumcision and dorsal nerve block of the penis. Anaesth Intensive Care 13(1): 79-82.
- Efe E, Resim S, Bulut BB, Eren M, Garipardic M, et al. (2013) Successful treatment with enoxaparin of glans ischemia due to local anesthesia after circumcision. Pediatrics 131(2): e608-611.
- Berens R, Pontus SP (1990) A complication associated with dorsal penile nerve block. Reg Anesth 15(6): 309-310.
- Uzun G, Ozdemir Y, Eroglu M, Mutluoglu M (2012) Electrocautery-induced gangrene of the glans penis in a child following circumcision. BMJ Case Rep 2012: bcr-2012-007096.
- Barnes S, Ben Chaim J, Kessler A (2007) Postcircumcision necrosis of the glans penis: gray-scale and color Doppler sonographic findings. J Clin Ultrasound 35(2): 105-107.
- Ozzeybek D, Koca U, Elar Z, Olguner M, Hakgüder G (1999) Glycerol trinitrate plus epidural sympathetic block in the ischemia of glans penis. Anesth Analg 89(4): 1066.
- Aminsharifi A, Afsar F, Tourchi A (2013) Delayed glans necrosis after circumcision: role of testosterone in salvaging glans. Indian J Pediatr 80(9): 791-793.
- Pepe P, Pietropaolo F, Candiano G, Pennisi M (2015) Ischemia of the glans penis following circumcision: case report and revision of the literature. Arch Ital Urol Androl 87(1): 93-94.
- Aslan A, Karagüzel G, Melikoglu M (2005) Severe ischemia of the glans penis following circumcision: a successful treatment via pentoxifylline. Int J Urol 12(7): 705-707.
- Tzeng YS, Tang SH, Meng E, Lin TF, Sun GH (2004) Ischemic glans penis after circumcision. Asian J Androl 6(2): 161-163.
- Gnatzy R, Fuchs J, Siekmeyer M, Beeskow AB, Gosemann JH, et al. (2018) Glans Ischemia after Circumcision in a 16-Year-Old Boy: Full Recovery after Angiography with Local Spasmolysis, Systemic Vasodilatation, and Anticoagulation. European J Pediatr Surg Rep 6(1): e66-e69.
- Polak N, Fishelev G, Lang E, Wang Z, Neheman A, et al. (2021) Hyperbaric Oxygen as Salvage Therapy for Neonates Suffering from Critical Ischemia of the Glans Penis After Circumcision. Urology 149: e48-e51.
- Tesloianu DN, Morosanu C, Roata EC, Sorodoc L (2016) Comparison Between Alprostadil and Iloprost in Intravenous Treatment of Patients with Chronic Peripheral Arterial Disease. Maedica (Bucur) 11(3): 186-190.
- Mittino I, Sangalli M, Fabbri F, Sozzi F, Ghezzi M, et al. (2018) Ischemia of the glans 24 hours after circumcision: A case report and therapeutic solution. Urologia 85(4): 174-176.
- Sterenberg N, Golan J, Ben-Hur N (1981) Necrosis of the glans penis following neonatal circumcision. Plast Reconstr Surg 68(2): 237-239.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...