
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Versatility of Extended Lateral Forehead Flap in Coverage of Full Thickness Facial Burns- A Case Report Volume 6 - Issue 3
Vijay Yashpal Bhatia1*, Shailendra Bhrigunath Singh1, Sruja Dipakbhai Narola2, Kena Maheshbhai Patel2, Ranjit Raghubhai Zapadiya2 and Rahul kaushik2
- 1Consultant plastic surgeon, Sterling Hospital, Ahemdabad, India
- 2Resident doctor , NHL Municipal medical college , Ahemdabad, India
Received: May 18, 2021 Published:June 02, 2021
Corresponding author: Vijay Yashpal Bhatia, Consultant Plastic Surgeon, Sterling hospital, Ahmedabad, Gujarat, 380059, India
DOI: 10.32474/SCSOAJ.2021.06.000239
Abstract
Lateral forehead flap a versatile flap based on the superficial temporal artery is a perfect match for restoration of the facial defect, we present here a case where in this flap was used to cover the full thickness defect of the left cheek with loss of the left alveolar sulcus associated with ectropion of the left lower lid due to burns giving an adequate tissue cover and contour of the face.
Keywords: Facial Defect; Superficial Temporal Artery; forehead Flap
Introduction
Finding an ideal donor with perfect skin match for reconstruction of facial defect creates a tough problem for the operating surgeon. Recently reconstructive ladder or escalator is advocated where in the reconstructive solution has to be individualized to each patient and not based on any rigid approach. In the era of microsurgery we chose to go with forehead flap as it’s a dependable and gives anatomical likeness in case of reconstruction. Forehead flap is a versatile flap used here for primary closure of the full thickness check defect of the left side of the face. It is the best donor site for facial reconstruction procedures due to colour match and texture. Success and popularity of this flap is due to adequate blood supply and local availability of a constant feeder vessel [1].
Case Report
Figure 1: Pre operative defect on the left side of face involving full thickness cheek with inner mucosa, upper gingival sulcus with associated ectropion.
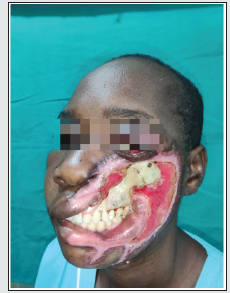
A 35 year old female patient presented with a full thickness defect of the left lateral cheek resulting from accidental flame burn four months back. Patient had lost consciousness and fell face first on a charcoal stove. The patient was taken to the nearest local hospital and required ventilator support for 4 days and treated conservatively for burns and referred to another hospital post extubation, for the defect but due to lack of expertise at the local hospitals, patient was referred to us for further management. Patient was assessed and had exposed maxilla, Zygoma on the left with loss of full thickness buccal mucosa, left upper outer gingival lining, left upper lip and left commissure. Decision was taken to use a lateral forehead flap [LFF] to cover the complex defect. Patient underwent relevant investigation preoperatively precise marking of the defect was marked and location of the superficial temporal artery [STA] with hand held Doppler on the left side was marked. A 20 *10 centimetres (cm) forehead flap was elevated ligating bilateral supra orbital and supra trochlear artery and contralateral frontal branch of superficial temporal artery, keeping the pedicle of the left STA secure. The left exposed maxillary and Zygomatic bone was chiselled to remove the dead and dried outer table to give us a vascularised recipient area over which the flap would survive and gain blood supply from. To reconstruct gingival sulcus, inner buccal mucosa, skin cover and ectropion release on the left side of face (Figure 1).
Operative Technique
The flap was raised based on left superficial temporal artery after marking it with a hand held doppler. The extended lateral forehead flap comprises whole of forehead just below the hairline superiorly and 1.5 cm above the eyebrow inferiorly, 1 cm lateral to the outer end of eyebrow and medially 1 cm in front of tragus. Tumescence was injected along the margins of flap and after a waiting period of 5-7 minutes incision was commenced from lateral end to base. The marginal incision is bevelled to give smooth transition from graft to surrounding skin. Flap elevated above the peri cranial layer/ sub fascial plane just superficial to the perisoteum of the frontal bone and the flap rotated over the lateral Zygomatic arch on the defect of the face; the flap was tailored to fit the defect of the face by turning the flap on itself to substitute the loss of buccal mucosa and creating an upper lip. The lower lip and upper lip gingival sulcus was formed by turning the forehead flap on itself and interdental wiring with stainless steel wire was used to hold the suture in place to form new gingival sulcus.
The forehead donor defect was covered with a single split thickness graft replacing the entire unit of forehead with a uniform graft. The flap was divided at 21 days and inset at the lower border to form a part of the missing lower lip. The patient was discharged uneventfully after the flap division and second inset. The patient was given RT Feeding for 21 days before the flap division to avoid tension on the sutures forming the inner lining of the cheek (Figure 2).
Discussion
The cheeks represent the largest surface area of the face and frame the central facial units. Reconstruction of defects involving the full thickness of the cheek implies reconstruction of all layers, while maintaining reasonable contour. [2] The extended lateral forehead flap is acknowledged as the ideal donor for midface reconstruction due to its colour and texture match, vascularity, and ability to resurface all or part of the reconstructed area. The flap is usually designed as an aesthetic unit and comprises the hairless skin of the forehead between the scalp and the eyebrows and extends laterally to the preauricular and temporal hair-bearing skin. The inferior border of the flap should lie immediately above the eyebrow, primarily to include the inferior branch of the superficial temporal artery but also to improve the donor site deformity by the use of a skin graft as a forehead aesthetic unit [3]. There are certain drawback with using lateral forehead flap like it requires two stage procedure, loss of eyebrow elevation, loss of forehead sensation, hairline distortion and resurfacing the donor area with split thickness graft can give a displeasing final result. However the advantages far outweigh the drawback like: [4].
The flap is easy to master, it has similar colour and texture to the face which follows the principle of replacing like with like.
The versatility of the flap helps us use it in diverse situations like malignancy trauma and it does not require any microsurgical expertise. The flap is less bulky and thus gives an ideal contour for oral and surface reconstruction. Faster harvest time make it useful in patients with morbid conditions. As the flap has a very robust blood supply, it is a reliable flap in case of possible future radiotherapy requirement in malignant cases and can be used as a salvage flap when primary reconstruction due to free flap fails. The patient complained of drooling of saliva which is a cause for social embarrassment and inability to contain liquids in the mouth and was not able to articulate certain words which required closure of the mouth preoperatively due to the large left facial defect. The patient was able to drink liquids, there was no dribbling of saliva and she could articulate plosive consonants in the postoperati.ve period. We echo here the same idea that Sir Harold Gillies and D. Ralph Millard had about the forehead flap “ The tint of forehead skin so exactly matches that of the face and nose that is must be the first choice” [5] (Figure 3).
Conclusion
Lateral forehead flap has a robust blood supply with less bulk on harvest makes it and ideal flap for a defect created after debridement of post burn raw area on the left side of the face. A single forehead flap is folded over itself to provide inner and outer lining. The advantage of the flap is that it is a reliable reconstructive option to giver cover to defects as far as the para mandibular region.
Declaration Of Patient Consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
References
- Rohrich RJ, Griffin JR, Ansari M, Beran SJ, Potter JK (2004) Nasal reconstruction beyond aesthetic subunits: A 15-year review of 1334 cases. Plast Reconstr Surg 114(6): 1405-1416.
- Mathes SJ, Henz VR, Jackson IT, et al. (2006) Plastic Surgery. (2nd Edn), Philadelphia, PA: Saunders Elsevier Inc, 345-391.
- Thorne CH, Beasley RW, Aston SJ, Bartlett SP, Menick FJ, et al. (2007) Grabb and Smith's Plastic Surgery. (6th Edn). Philadelphia, PA: Lippincott Williams & Wilkins, 389-396.
- Midya M, Galwa R, Goil P(2020) The utility of the lateral forehead flap in demanding reconstructive situations: our experience in a tertiary care centre. Nigerian J Plast Surg 16: 9-17
- Gillies H, Millard, R(1957) The Principles and Art of Plastic Surgery. Boston: Little , Brown.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...






