Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Research Article(ISSN: 2643-6760) 
Therapeutic Management of Iliac Anuerysmas are Open Operation Still Indicated? Volume 6 - Issue 1
Masoud Mirzaie*, Zaur Guliyev and Sheila Fatehpur
- Department of Vascular Surgery, University Hospital Lemgo, Germany
Received: September 24, 2020; Published: October 05, 2020
Corresponding author:Masoud Mirzaie, Head of the Department of Vascular Surgery University Hospital of Lemgo, Lemgo, Germany
DOI: 10.32474/SCSOAJ.2020.06.000227
Abstract
Objective: Isolated aneurysms of the iliac artery are relatively rare (7% of all intra-abdominal aneurysms), but also pose a great therapeutic challenge in combination with aortic aneurysms. As a rule, iliac aneurysms with a size of > 3 cm are treated independently of the abdominal aortic aneurysm, in the interventional setting. In case of contraindications due to anatomical findings and patient-specific contraindications, such patients have to undergo a complex revascularization operation.
Patientsand Methodology: For this study, between 2007 and 2017, 28 patients with complicated BAA with irrigation of the iliac arteries or with isolated iliac aneurysms in contraindications to interventional therapy underwent surgery. All patients underwent multi-detector row CT with three-dimensional (3D) reformation in 3 mm slices. In addition, peripheral blood flow was determined in all patients by measuring ABI. Primary and secondary outcome of patients was determined after 30 days, after 3 months, and then every 6 months.
Results: The extension of the aneurysm of the a. iliaca required in all cases the implantation of a Y-prosthesis, in 22 cases bifemoral, in 4 cases biiliac, in 2 cases with unilateral aneurysm of the a. iliac, unilateral anastomosis iliac and 2nd anastomosis femoral. In 26 cases an internal iliac artery revascularization was performed, in 3 cases even both arteries. Iliacae internae. The interponent to the revascularizing internal iliac artery was always implanted in the opposite leg of the Y-prosthesis. In 2 cases the internal iliac artery was unilaterally ligated and the reciprocal internal iliac artery revascularized. In 4 cases, the inferior mestric artery was reimplanted in the left prosthesis leg, in 3 cases, with revascularization of both arteries. Iliacae internae ligated. In 21 patients this was closed. To illustrate the surgical techniques
Conclusion: One of the patients with a perforated aneurysm of the internal iliac artery died of urosepsis shortly after his discharge, all other patients survived the operation very well. Postoperativegluteal ischemia did not occur in any of the patients. The duplex sonographic anastomoses to internal iliac artery were inconspicuous to date. Postoperative mesenteric ischemia did not occur in patients with ligature of the internal mesenteric artery. The surgical procedure presented here, which is adapted to the anatomic conditions of each patient, represents a demanding form of therapy which, in case of contraindications to conventional therapy, represents the only possibility for the treatment of such patients.
Keywords: Open surgery, ilical aneuryms
Introduction
With about 7% of intraabdominal anuerysms, isolated aneurysms of the iliac artery are a rarity [1-4]. In most cases (80%), iliac aneurysm involves the infrarenal aorta[5]. Incredibly, iliac aneurysms occur twice as often on the left side as on the right side [6]. The indication for treatment of isolated iliac aneurysms is considered to be larger than 3 cm, although there are reports of perforation of small aneurysms [7-9]. Previously established surgical therapy of isolated iliac aneurysms is increasingly being replaced by endovascular therapy [10-12]. Especially in the first post-interventional years, interventional procedures have advantages over open procedures, which show a mortality rate of 7-11% for elective operations and more than 50% for emergencies [13,14]. In addition, anatomical variants as well as pathological findings such as ectasia or aneurysm of the iliac artery lead to the formation of an endoleak type Ib in 15% of EVAR-treated patients with an iliac aneurysm [15,16]. To avoid this, unilateral or bilateral embolization of the internal iliac artery is recommended [17-19]. This procedure often leads to pelvic claudication, sexual disorders, circulatory disorders of the spinal cord and ischemic colitis. Newly developed stent prostheses with one side arm for the internal iliac artery and new techniques such as the sandwich technique are limited in the proximal landing zone in ectasia of the comm. iliac artery [20-24]. Intentional therapy of all types of iliac aneurysms (I-V) involves embolization of the iliac artery, in types IV and V the affected pelvic axis may even be closed, and blood flow to the extremities of the affected side is restored using a crossover bypass [14]. The site branch methods available to reduce complications caused by occlusion of the internal iliac artery require a considerably longer period of operation, which despite the primary success can lead to occlusion of the internal iliac artery with all its consequences[21,25-32]. Often complicated isolated iliac aneurysms or large BAA with involvement of iliac arteries must be adequately treated by complicated surgical procedures. The present study describes the surgical deficiency of such patients using several examples.
Material and Methods
Patients
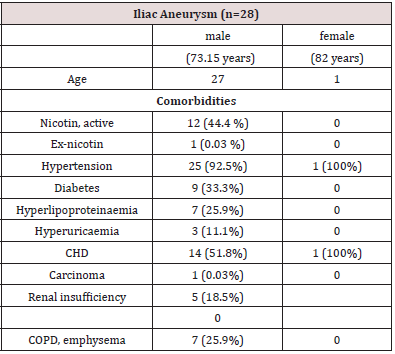
Between 2007 and 2017, 28 patients with complicated BAA with irrigation of the iliac arteries or with isolated iliac aneurysms in contraindications to interventional therapy underwent surgery. Patient data are shown in Table 1.
PreproceduralImaging
All patients underwent multi-detector row CT with CT and three-dimensional (3D) reformation in 3 mm slices to accurately measure the proximal and distal length and extent of the aneurysm. In addition, peripheral blood flow was determined in all patients by measuring ABI. In patients with intermittent claudication, the walking distance without symptoms was measured on a treadmill at a speed of 3.5 km/h with a 3.5% increase.
Followup Protocol
The primary outcomes were determined by mortality within 30 days of the operation, then after 3 months and from then on, every 6 months. All procedure-dependent and aneurysm dependent as well as minor and major pelvic ischemia were considered.Secondary outcomes were determined by checking blood flow, duplex sonographic imaging of the anastomoses, treadmill examination and in rare cases with unclear findings by CT angiography.
Surgicalindications
The indication for surgery was given for combined BAA with an iliac aneurysm for fusiform aneurysms with a size > 5 cm, or a growth tendency of 1 cm/year, for a saccular aneurysm independent of the size or for combined BAA and iliac aneurysm for smaller BAA < 5 cm, for an aneurysm size of the A. iliaca > 3cm. The isolated iliac aneurysms were only operated on if the size of the aneurysm was > 3 cm or in case of complications. The indication for conventional elimination of the aneurysms was only given after exclusion of the interventional therapy in an interdisciplinary conference. The exclusion criteria for the interventional elimination of the aneurysms were: lack of possibility for proximal placement of the stentin type III and IV according to Sakamoto et al. [14], unilateral closure of the A iliaca interna, bilateral aneurysms of the internal iliac artery with involvement of the internal iliac artery or bilateral aneurysms of the internal iliac artery, severe renal insufficiency with a GFR of less than 30 ml/, and KM allergy.
Results
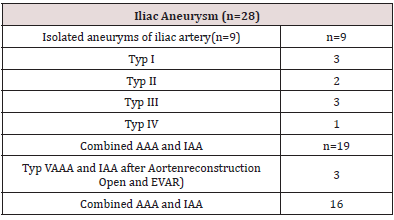
There were 9 patients with isolated iliac aneurysms, 2 patients with a perforated Re-BAA combined with an iliac aneurysm after application of a Y-prosthesis, one patient with a perforated Re-BAA combined with an iliac aneurysm after EVAR, and 16 patients with a combined BAA and iliac aneurysms. In 3 of these 16 patients there was a surgical indication even without an iliac aneurysm with a BAA size >5 cm (Table 2).
Operating techniques
As shown in Table 2, the extension of the aneurysm of the a. iliaca required in all cases the implantation of a Y-prosthesis, in 22 cases bifemoral, in 4 cases biiliac, in 2 cases with unilateral aneurysm of the a. iliaca, unilateral anastomosis iliac and 2nd anastomosis femoral. In 26 cases an internal iliac artery revascularization was performed, in 3 cases even both arteries. Iliacae internae. The interponent to the revascularizing internal iliac artery was always implant2ed in the opposite leg of the Y-prosthesis. In 2 cases the internal iliac artery was unilaterally ligated and the reciprocal internal iliac artery revascularized. In 4 cases, the inferior mestric artery was reimplanted in the left prosthesis leg, in 3 cases, with revascularization of both arteries. Iliacae internae ligated. In 21 patients this was closed. To illustrate the surgical techniques, 3 cases are presented as examples.
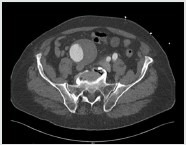
Case 1: 74-year-old patient with a randomly determined infrarenal BAA of 4.6 cm and a 4.4 aneurysm of the iliac artery comm. An interventional elimination of the aneurysm was not possible due to the extension of the aneurysm of the iliac artery comm. The aneurysms were resected, and a Y-prosthesis was implanted, on the right side to the A. iliaca comm. shortly before the iliac bifurcation and on the left side to the A iliacaexterna. The left internal iliac artery was revascularized by an interponate to the right leg of the Y- prosthesis (Figures 1 & 2):
Figure 1: 3-d CT-angiography of aorta: infrarenal BAA of 4.6 cm and a 4.4 aneurysm of the left iliac artery com.

Figure 2:resection of aneurysms and implantation of a y-prosthesis aorto-biiliac and revascularization of left iliac interna artery with an interponat to right leg of y-prosthesis.

Case 2: The 83-year-old patient was admitted emergency under the clinical picture of hypovolemic shock with severe abdominal pain. The immediately performed CT angiography of the aorta with KM in 3 mm slices showed a covered perforated aneurysm of the right internal iliac artery. He underwent emergency surgery. The perforated aneurysm of the internal iliac artery was uncovered, and all vessels were ligated after the aorta and the left iliac artery were disconnected. The segment of the common iliac artery with the exit of the internal iliac artery was resected and the common iliac artery anastomosed end-to-end (Figure 3).
Figure 3: 3-d CT-angiography of aorta: covered perforated aneurysm of the right internal iliac artery.

Case 3: In the 82-year-old patient, in addition to a considerable elongation of the aorta, an aneurysm of the right common iliac artery and the left internal iliac artery had been known for some time. During a urological follow-up examination, the aneurysm of the right common iliac artery had shown a considerable size progression to 7 cm and the internal iliac artery to 4 cm. An interventional elimination of these findings was not possible due to the necessary revascularization of the right internal iliac artery. Therefore, the aneurysms were resected, and a Y-prosthesis was implanted between the aorta and the external arteries on both sides. The internal iliac artery on the left side. In addition, was revascularized by on interponat to the right prosthetic leg, and the right internal iliac artery by on another interponat to the first interponent(Figures 4-7).All of these patients underwent a followup examination. In addition to the peripheral blood flow, the blood flow of the internal iliac artery was measured by duplex sonography. One of the patients with a perforated aneurysm of the internal iliac artery died of urosepsis shortly after his discharge, all other patients survived the operation very well. Postoperative gluteal ischemia did not occur in any of the patients. The duplex sonographic anastomoses to internal iliac artery were inconspicuous to date. Postoperative mesenteric ischemia did not occur in patients with ligature of the internalmesenteric artery.
Figure 6: 3-d CT-angiography of aorta considerable elongation of the aorta, a 7 cm aneurysm of the right common iliac artery and 4 cm aneurysm of left internal iliac artery.
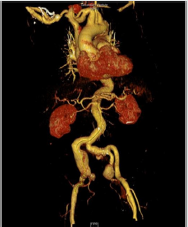
Figure 7: Intraoperative situs: implantation of a y-prosthesis was implanted between the aorta and the external arteries on both sides, revascularization of the left interna iliac artery by an interponat to the right prosthetic leg, and revascularization of the right internal iliac artery by an another interponat to the first interponat.

Discussion
The more than 80% of cases of iliac aneurysms associated with BAA or occurring in isolation are still a major therapeutic challenge, not only because of the considerable risk of perforation and the associated mortality and morbidity [33-35]. Even for electively treated patients with aneurysms larger than 5 cm, mortality, and morbidity rates of 11-13% are reported [36,37]. The current treatment concepts for isolated and combined iliac aneurysms are covered in current guidelines for the treatment of BAA, so that the consensus on the explicit indication size for iliac aneurysms was derived from observation cases of perforated iliac aneurysms. Accordingly, an aneurysm size of >3 cm is considered to be the intervention size [38,39]. The indication for surgical therapy in case of contraindications to interventional therapy isgiven in case of a size of 3 cm, a growth tendency > 5 mm/year and the occurrence of symptoms and complications [39-42]. Different factors such as the aneurysm morphology (size, shape, uni- or bilateral), wall pathologies of the aneurysm sac (thrombi, calcification), the existence of a landing zone (length, diameter), the perfusion conditions of the aneurysm. iliaca interna and the anatomy of the pelvic arteries (vessel diameter, angulation, elongation, kinking, tortuosity) and their wall pathologies (calcification and thrombus load) are taken into account in the considerations of technical realization, the choice of materials and the planning of the procedure[43].
Due to high morbidity and mortality rates, endovascular procedures are preferred, although open and interventional therapy procedures do not differ from each other over the long term in terms of mortality, openness, and complication rates. Only in terms of 30-day mortality, inpatient length of stay and transfusion frequency is there an advantage in favour of endovascular procedures[44-47].The maintenance of perfusion of the internal iliac artery is ensured by the sandwich and iliac sidebranch technique, particularly in the frequent type I and III aneurysms according toPfabe et al. [48-55].Together with the procedures described above, the bell-bottom technique is also expected to reduce the risk of serious complications of a perfusion failure of the internal iliac artery such as gluteal necrosis, impotence, ischemic colitis, ileus and sepsis[56-59].The lack of a proximal anchorage of the prosthesis, distal torsion of the internal iliac artery and accompanying stenoses lead to significantly longer operating times, radiation exposure, leading to early closure of the branch, thus the induction of pelvic ischemia[27].Thus, the very demanding surgical procedure represents an alternative method of treating these patients. As we were able to show with 3 examples, a reconstruction procedure was developed for each patient individually according to the anatomic conditions and pathological findings, which, in addition to the anatomic reconstruction of the pelvic tract, ensures the revascularization of the internal iliac artery. In cases with clear contraindications to interventional therapy, the procedure presented here is the only therapeutic procedure. Follow-up examinations showed an acceptable postoperative result even after 10 years. None of the patients showed signs of ischemia based on the internal iliac artery. Only the surgical technique makes high demands on the surgeon, which despite enormous progress in interventional therapy procedures is part of the repertoire of vascular surgeons.
Conflict of Interest
I hereby declare that there were no financial or other interests in the execution and evaluation of this work.
References
- Fann JI (2002) Descending thoracic and thoracoabdominal aortic aneurysms. Coronary Artery Disease 13(2): 93-102.
- Etheredge SN, Yee J, Smith JV, Schonberger S, GoldmanMJ (1955) Successful resection of a large aneurysm of the upper abdominal aorta and replacement with homograft. Surgery 38(6): 1071-1081.
- Cambria RP, Clouse WD, Davison JK, Dunn PF, Corey M et al. (2002) Thoracoabdominal aneurysm repair: results with 337 operations performed over a 15-year interval. Annals of Surgery 236(4): 471-479.
- Orr N, Minion D, Bobadilla JL (2014) Thoracoabdominal aortic aneurysm repair: Current endovascular perspectives. Vascular Health and Risk Management 10: 493-505.
- Armon MP, Wenham PW, Whitaker SC, Gregson RH, B R Hopkinson BR (1998) Common iliac artery, aneurysms in patients with abdominal aortic aneurysms. Eur J Vasc Endovasc Surg 15(3): 255-257.
- Wilhelm BJ, Sakharpe A, Ibrahim G, Baccaro LM, Fisher J (2014) The 100-Year Evolution of the Isolated Internal Iliac Artery Aneurysm. Ann Vasc Surg 28(4):1070-1077.
- Huang Y, Gloviczki P, Duncan AA, Kalra M, Hoskin TL et al. (2008) Common iliac artery aneurysm: expansion rate and results of open surgical and endovascular repair. J Vasc Surg 47(6): 1203‐1210.
- Santilli SM, Wernsing SE, Lee ES (2000) Expansion rates and outcomes for iliac artery aneurysms. Journal of Vascular Surgery 31(1): 114‐121.
- Soury P, Brisset D, Gigou F, Saliou C, Angel F et al. (2001) Aneurysms of the Internal Iliac Artery: Management Strategy. Ann Vasc Surg 15(3): 321-325.
- Dubost C, Allary M, Oeconomos N (1952) Resection of an aneurysm of the abdominal aorta: Reestablishment of the Continuity by a preserved human arterial graft, with result after five months. JAMA Surgery 64(3): 405-408.
- Najibi S, Terramani TT, VJ Weiss, MJ Mac Donald, PH Lin et al. (2002) Endoluminal versus open treatment of descending thoracic aortic aneurysms. J Vasc Surg 36(4): 732-737.
- Makaroun MS, Dillavou ED, Wheatley GH, Cambria RP (2008) Five-year results of endovascular treatment J Vasc Surg 47(5): 912-918.
- Antoniou GA, Antoniou SA, Torella F (2020) Endovascular vs. Open Repair for Abdominal Aortic Aneurysm: Systematic Review and Meta-analysis of Updated Peri-operative and Long-Term Data of Randomised Controlled Trials. Eur J Vasc Endovasc Surg 59: 385-397.
- Machado RM, Cunha Rego DN, Pinto de Oliveira PNF, Fernandes de Almeida RMG (2016) Endovascular Treatment of Internal Iliac Artery Aneurysms: Single Center Experience. Braz J Cardiovasc Surg 31(2): 127-131.
- Bosanquet DC, Wilcox C, Whitehurst L, Cox A, Williams IM et al. (2017) Systematic review and meta‐ analysis of the effect of internal iliac artery exclusion for patients undergoing EVAR. Eur J Vasc Endovasc Surg 53(4): 534-548.
- Cannavale A, Lucatelli P, Corona M, Nardis P, Basilico F et al. (2020) Evolving concepts and management of endoleaks after endovascular aneurysm repair: where do we stand in 2019? Clin Radiol 75(3): 169-178.
- Fatima J, Correa MP, Mendes BC, Oderich GS (2012) Pelvic revascularization during endovascular aortic aneurysm repair. Perspect Vasc Surg Endovasc Ther 24(2): 55-62.
- Tefera G, Turnipseed WD, Carr SC, Pulfer KA, Hoch JR et al. (2004) Is coil embolization of hypogastric artery necessary during endovascular treatment of aortoiliac aneurysms? Annals of Vascular Surgery 18(2): 143‐146.
- Wu Z, Raithel D, Ritter W, Qu L (2011) Preliminary embolization of the hypogastric artery to expand the applicability of endovascular aneurysm repair. J Endovasc Ther 18(1): 114-120.
- Bosanquet DC, Wilcox C, Whitehurst L, Cox A, Williams IM, et al. (2017) Systematic review and meta‐ analysis of the effect of internal iliac artery exclusion for patients undergoing EVAR. Eur J Vasc Endovasc Surg 53(4): 534‐548.
- Verzini F, Parlani G, Romano L, Rango P, Panuccio G et al. (2009) Endovascular treatment of iliac aneurysm: concurrent comparison of side branch endograft versus hypogastric exclusion. J Vasc Surg 49(5): 1154‐1161.
- Smeds MR, Wilensky JA, Lyons LC, Ali AA, Moursi MM (2014) Preservation of pelvic perfusion in endovascular aneurysm repair. J Ark Med Soc 111(2): 43-45.
- Oderich GS, Greenberg RK (2011) Endovascular iliac branch devices for iliac aneurysms. Perspect Vasc Surg Endovasc Ther 23(3):166‐172.
- Lobato AC, Camacho-Lobato L (2013) The sandwich technique to treat complex aortoiliac or isolated iliac aneurysms: Results of midterm follow-up. J Vasc Surg 57(2): 26-34.
- Parlani G, Verzini F, Rango P, Brambilla D, Coscarella C et al. (2012) Long‐term results of iliac aneurysm repair with iliac branched endograft: a 5‐year experience on 100 consecutive cases. Eur J Vasc Endovasc Surg 43(3): 287‐292.
- Taudorf M, Gronvall J, Schroeder TV, Lonn L (2016) Endovascular aneurysm repair treatment of aortoiliac aneurysms: can iliac branched devices prevent gluteal claudication? J Vasc Interv Radiol 27(2): 174‐180.
- Donas KP, Inchingolo M, Cao P, Pratesi C, Pratesi G et al. (2017) Secondary procedures following iliac branch device treatment of aneurysms involving the iliac bifurcation: the pELVIS registry. J Endovasc Ther 24(3): 405‐410.
- Ghosh J, Murray D, Paravastu S, Farquharson F, Walker MG et al. (2009) Contemporary management of aorto‐iliac aneurysms in the endovascular era. Eur J Vasc Endovasc Surg 37(2): 182‐188.
- Fargion A, Pratesi C, Masciello F, Dorigo W, Pratesi G (2019) Hypogastric Artery Management During Open and Endovascular Aortoiliac Repair in Challenges and Difficult Cases. Tshomba, Yamume, Baccellieri, Domenico, Chiesa, Roberto (Eds.), Visceral Vessels and Aortic Repair (412): 91-103.
- Mehta M, Veith FJ, Darling RC, Roddy SP, Ohki T et al. (2004) Effects of bilateral hypogastric artery interruption during endovascular and open aortoiliac aneurysm repair. J Vasc Surg 40(4): 698‐702.
- Rayt HS, Bown MJ, Lambert KV, Fishwick NG, McCarthy MJ et al. (2008) Buttock claudication and erectile dysfunction after internal iliac artery embolization in patients prior to endovascular aortic aneurysm repair. Cardiovasc Intervent Radiol 31(4): 728‐734.
- Behrendt CA, Sedrakyan A, Rieß HC, Heidemann F, Tilo Kölbel T (2017) Short-term and long-term results of endovascular and open repair of abdominal aortic aneurysms in Germany. Ann Vasc Surg 66(6): 1704-1711.
- Scheinert D, Schröder M, Steinkamp H, Ludwig J, Biamino G (2018) Treatment of Iliac Artery Aneurysms by Percutaneous Implantation of Stent Grafts. Circulation 102(3): 253-258.
- Kim JY, Kim DH, Quan C, Suh YJ, Ann HY et al. (2019) Treatment options for isolated iliac artery aneurysms and their impact on aortic diameter after treatment. Ann Surg Treat Res 96(3): 146-151.
- Parker LP, Powell JT, Kelsey LJ, Lim B, Ashleigh R et al. (2019) Morphology and Hemodynamics in Isolated Common Iliac Artery Aneurysms Impacts Proximal Aortic Remodeling. Arterioscler. Thromb Vasc Biol 39(6): 1125-1136.
- Joviliano EE, Vieira D, Moreira LdS, Foroni Al (2019) Endovascular treatment of bilateral isolated aneurysm of the internal iliac artery. J vasc bras 18: 167-173.
- Leon Jr LR, Mills JL, Psalms SB, Goshima K, Son T et al. (2007) A safe approach to the treatment of iliac artery aneurysms: aortobifemoral bypass grafting with exclusion of the aneurysm. J Vasc Surg 45(6): 1244-1248.
- Xiang Y, Chen X, Zhao J, Huang B, Yuan D et al. (2019) Endovascular Treatment Versus Open Surgery for Isolated Iliac Artery Aneurysms: A Systematic Review and Meta-Analysis. Vasc Endovasc Surg 53 (5): 401- 407.
- Melas N, Saratzis A, Dixon H, Saratzis N Lazaridis J et al. (2011) Isolated Common Iliac Artery Aneurysms: A Revised Classification to Assist Endovascular Repair. J Endovasc Ther 18(5): 697-715.
- Richards T, Dharmadasa A, Davies R, Murphy M, Perera R et al. (2009) Natural history of the common iliac artery in the presence of an abdominal aortic aneurysm. J Vasc Surg 49(4): 881-885.
- Kotsis T, Louizos LA, Pappas E, Theodoraki K (2014) Complex Common and Internal Iliac or Aortoiliac Aneurysms and Current Approach: Individualized Open-Endovascular or Combined Procedures. Int J Vasc Med 178610.
- Kirkwood ML, Saunders A, Jackson BM, Wang GJ, Fairman RM et al. (2011) Aneurysmal iliac arteries do not portend future iliac aneurismal anlargement after endovascular aneurysm repair for abdominal aortic aneurysm. J Vasc Surg 53(2): 269-273.
- Kaladji A, Daoudal A, Duménil A, Göksu C, Cardon A et al. (2017) Predictive Models of Complications after Endovascular Aortic Aneurysm Repair. Ann Vasc Surg 40: 19-27.
- Zhorzel S, Busch A, Trenner M, Reutersberg B, Salvermoser M et al. (2019) Open Versus Endovascular Repair of Isolated Iliac Artery Aneurysms. Vasc Endovas Surg 53(1): 12-20.
- Patel NV, Long GW, Cheema ZF, Rimar K, Brown OW et al. (2009) Open vs. endovascular repair of isolated iliac artery aneurysms: A 12-year experience. J Vasc Surg 49(5): 1147-1153.
- Uberoi R, Tsetis D, Vivek Shrivastava V, Morgan R, Belli AM (2010) Standard of practice for the interventional management of isolated iliac artery aneurysms. Cardiovasc Intervent Radiol 34(1): 3-13.
- Rana MA, Kalra M, Oderich GO, Duncan AA, Cha SS et al. (2014) Outcomes of open and endovascular repair for ruptured and nonruptured internal iliac artery aneurysms. J Vasc Surg 59(3): 634-644.
- Parlani G, Verzini F, De Rango P, Brambilla D, Coscarella C et al. (2012) Long-term Results of Iliac Aneurysm Repair with Iliac Branched Endograft: A 5-Year Experience on 100 Consecutive Cases. Eur J Vasc Endovasc Surg 43(3): 287-292.
- G Simonte G, Parlani g, Farchioni L, Isernia G, Cieri E et al. (2017) Lesson Learned with the Use of Iliac Branch Devices: Single Centre 10 Year Experience in 157 Consecutive Procedures. Eur J Vasc Endovasc Surg 54(1): 95-103.
- Karathanos C, Kaperonis E, Xanthopoulos D, Konstantopoulos T, Exarchou M et al. (2013) Endovascular Treatment of Isolated Iliac Artery Aneurysms with Anaconda Stent Graft Limb. Case Rep Vasc Med 2013: 527492.
- Hwang HP, Yang JD, Jeong JH, Han YM, Yu HC et al. (2011) Endovascular Treatment of an Internal Iliac Artery Aneurysm Using Amplatzer. Vascular Plug: 2 Case Reports Korean J Vasc Endovasc Surg 27: 120- 124.
- Bischoff MS, Peters AS, Meisenbacher K, Böckler D (2014) Challenging access in endovascular repair of infrarenal aortic aneurysms. J Cardiovasc Surg (Torino) 55(2) :75-83.
- Gonçalves FB, Oliveira NF van Rijn MJ, Ultee KHJ, Hoeks SE et al. (2017) Iliac Seal Zone Dynamics and Clinical Consequences After Endovascular Aneurysm Repair. Eur J Vasc Endovasc Surg 53(2): 185-192.
- Parker L, Doyle B, Powell J, Kelsey L, Koncar I et al. (2019) Morphology and Computational Flow Dynamics Support a Novel Classification of Isolated Common Iliac Aneurysms, with Impact on Aneurysm Prognosis. Eur J Vasc Endovasc Surg 58(6): 212.
- Rouby AF, Kuntz S, Delay C, Thaveau F, Georg Y et al. (2019) Volume Change after Endovascular Treatment of Common Iliac Arteries ≥ 17 mm Diameter: Assessment of Type 1b Endoleak Risk Factors. Eur J Vasc Endovasc Surg 59(1): 51-58.
- Greenberg RK, Qureshi M (2010) Fenestrated and branched devices in the pipeline. J Vasc Surg 52: 15- 21.
- Boules TN (2006) Endovascular management of isolated iliac artery aneurysms. J Vasc Surg 44: 29-37.
- Mansukhani NA, Havelka GE, Helenowski IB, Rodriguez HE, Hoel AW et al. (2017) Hybrid Endovascular Aortic Aneurysm Repair: Preservation of Pelvic Perfusion with External to Internal Iliac Artery Bypass. Ann Vasc Surg 42: 162-168.
- Marcos FA, de la Torre AG, Perez MA, Garcia-Cosio Mir JM, Garcia FV (2013) Use off aortic extension cuffs for preserving hypogastric blood flow in endovascular aneurysm repair with aneurysmal involvement of common iliac arteries. Ann Vasc Surg 27(2): 139-145.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...