Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Testicular Torsion in Adolescent: A Dilemma in Early Diagnosis Lead to Infarction of Testis Volume 4 - Issue 5
Pankaj Srivastava1*, Shalini Srivastava2, Dhirendra Ray3, Ram Jeet Maurya4, Neeraj Arora5, Richu Grover5 and Sagar Srivastava6
- 1Surgery, Om Surgical Center & Maternity Home, Varanasi, India
- 2Om Surgical Center & Maternity Home, Varanasi, India
- 3Sirona Diagnostika, Varanasi, India
- 4Om Surgical Center & Maternity Home, Varanasi, India
- 5Rama Medical College and Research Hospital, Kanpur, India
- 6Clinical research Coordinator, Om Surgical Center & Maternity Home, Varanasi, India
Received: February 26, 2020; Published: April 30, 2020
Corresponding author: Pankaj Srivastava, Laparoscopic, Thoracic, Thoracoscopic & VATS Surgeon, Om Surgical Center & Maternity Home, SA 17/3, P-4, Sri Krishna Nagar, Paharia, Ghazipur Road, Varanasi, UP, India
ORCID ID: https://orcid.org/0000-0002-7321-614X
DOI: 10.32474/SCSOAJ.2020.04.000199
Abstract
Testicular torsion is an acute emergency condition that warrants urgent diagnosis to save the testis from fatal infarction. We herein report a case of Testicular infarction due to testicular torsion in a 15 years old young boy. The purpose of presenting this case is to emphasize the early intervention of Color Doppler study of scrotum to avoid delayed surgical corrective measures which, if taken on time, could have saved the testis. We strongly recommend that Testis must be examined by the consulting physician in all patients presenting with nausea, vomiting and abdominal pain and if found tender, the immediate ultrasonography of the scrotum with color doppler imaging should be done. It should also be included in the differential diagnosis of the any lower abdomen pain on either side irrespective of absence of testicular tenderness or any local complaints.
Keywords: Testis, Torsion, Infarction, Testicular torsion, Acute scrotum, Testicular pain, Color doppler, Adolescent
Introduction
Testicular torsion is considered one of the important causes of acute scrotum. The first reported case of torsion of an undescended testis was published in 1840 [1]. The original and schematic illustrations of testicular torsion was first published and classified in 1894 [2]. Torsion of the testicular appendix was first described by Colt [3]. It occurs in about 1 in 4,000 to 1 per 25,000 males per year before 18 years of age [4]. Sixty two percent of cases occur in patients aged 12–18 years and 89% below the age of 25 years [5]. Although its overall incidence is not high, it remains the most common cause of testicular loss in these age groups. However, torsion may occasionally occur in men of 40-50 years old [6]. The classic presentation is acute, severe scrotal pain at rest. Testicular torsion is the cause of 16–39.5% of cases of acute scrotum in childhood [7]. Testicular torsion is the most common cause of acute scrotum in the first year of life (83%) [8]. For testicular salvage, time is of the essence-the earlier the surgical intervention, the higher the likelihood of testicular salvage [9]. The two most important factors determining testicular damage are the time from the onset of symptoms to the reduction of torsion and the degree of twisting in the cord [10].
Case Presentation
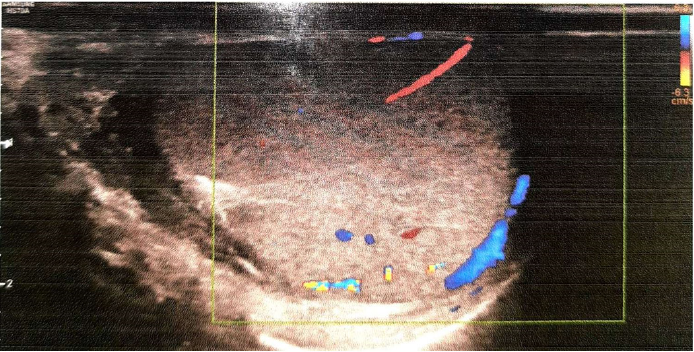
A 15-years-old non-smoker, non-alcoholic, boy presented with pain in right lower abdomen with few episodes of vomiting one day back. The pain in abdomen was started at 2 am night which was very severe in nature and associated with vomiting. The patient consulted nearby hospital for the same and he was given pain killer injections twice at different time interval after that he got some relief but again he developed pain. Next day in evening, he consulted to our hospital and narrated the same symptoms. His oral temperature was 98.40 F, pulse rate was 76/minute, Blood Pressure was 110/70 mmHg, Respiratory rate was 18/min. On examination, tenderness was present in right iliac fossa which increased on deep palpation. There was no organomegaly or palpable lump in whole abdomen. Provisional diagnosis of acute appendicitis was made and he was advised for admission but anyhow attendants refused; therefore, he was given antibiotics with anti-inflammatory orally and liquid diet only. Next day morning, he came again to the hospital and repeated same complains but additionally he was also complaining of heaviness in his right testis despite of all medications. The vitals were still normal but abdomen was tender in right iliac fossa region. His scrotum was also examined which was absolutely normal except tenderness present in right testis. There were no signs of inflammation. On the basis of high index of suspicion, ultrasonography (USG) of the abdomen and scrotum was advised with color doppler (CD) study particularly of the testis and epididymis. There was no abnormality detected in USG abdomen but USG scrotum revealed bulky right tetis (38x33x29mm) and epididymis with heterogeneous echotexture. There was absent vascularity in right testis on color Doppler study (Figure 1). Left testis with appendages was absolutely normal. On the basis of history, examination and CD study of scrotum, the diagnosis of torsion of right testis was made and patient was planned for emergency exploration.
Figure 1: CD study of scrotum revealed bulky right testis (38x33x29mm) with bulky epididymis with heterogeneous echotexture and no vascularity.
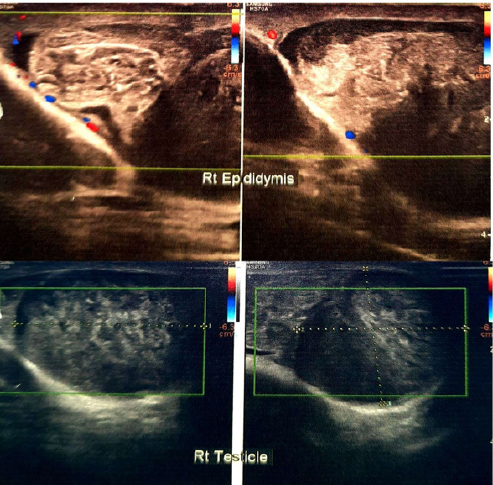
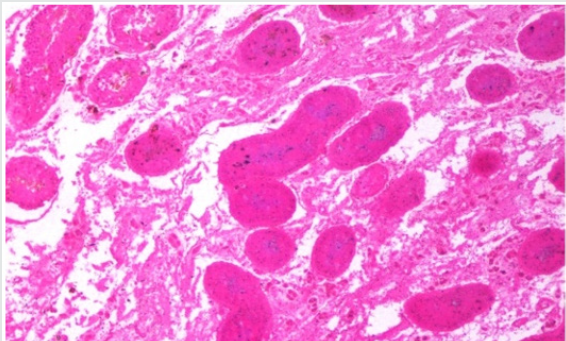
Under spinal anesthesia, the scrotum was opened through midline raphe incision. The right testis was explored after meticulous dissection and found bit swollen, deep blue to black in color with two and a half circle (~900°) anticlockwise rotated. The testis was then derotated and was examined for viability. As there were no sign of viability, decision of orchidectomy was taken by labelling testis as infracted one. Testis was then removed with epididymis. Contralateral fixation of testis was not performed because of severe necrosis of the twisted right testis. Wound was thoroughly washed with warm saline and closed in layers. The cut section of the test is revealed hemorrhagic black parenchyma with dark red colored blood collection (Figure 2). Postoperative period was uneventful. Patient was discharged after 48 hours of operation. Scrotal stitches were removed on day 7 postoperatively. Gross examination of the test is revealed specimen weight 41gm. Whole specimen measuring 6.0 x 4.0 x 2.5cm. Testis measuring 4.5 x 4.0 x 2.5cm. Spermatic cord measuring 3.0 x 2.0 cm. Cut surface shows hemorrhagic areas. Histologic examination revealed testicular tissue with marked hemorrhage and congested vessels (Figure 3). Histomorphological findings are compatible with torsion of the testis.
Figure 2: The cut section of the testis revealed hemorrhagic black parenchyma with dark red colored blood collection.
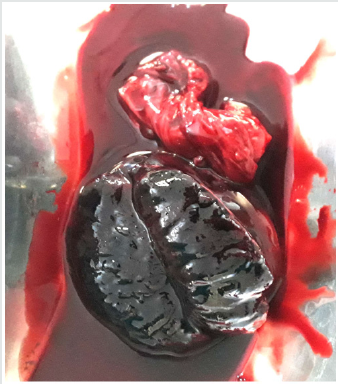
Figure 3:Histologic examination revealed testicular tissue with marked hemorrhage and congested vessels.
Discussion
Testicular torsion should be suspected in neonates and peripubertal boys presenting with acute scrotum; torsion of a testicular appendage is more common in prepubertal boys, and epididymitis most often develops in postpubertal boys [11]. The most common and alarming complaint is generalized testicular pain at rest. However, the presentation is variable and there may or may not be any history of trauma or physical activity. Nausea and vomiting can occur. Dysuria and fever are not common [9]. Testicular torsion pain is of acute and severe in nature and usually begins to reduce after 6 hours of onset [12]. Epididymitis or appendiceal torsion causes moderate pain [11]. Abdominal pain may be the presenting symptom in 5–25% of patients [5,12]. Nausea and vomiting may be present in 26–60% of testicular torsion cases. Nausea has a positive predictive value of 96% and vomiting 98% for torsion, but both have lower sensitivity [13,14]. 5–7% of patients may present with urinary symptoms. The symptoms are typically slight frequency and dysuria. Past history of similar pain episodes that resolved spontaneously is suggesting intermittent torsion with spontaneous detorsion [13,15]. Fever, scrotal edema and induration are also the presenting features and all denote the bad prognosis regarding testicular viability.
On examination, diffuse testicular tenderness is universal.
Abnormal lie and absence of a cremasteric reflex are also common.
It has been observed that there is a 100% correlation between the
presence of the cremasteric reflex and the absence of testicular
torsion, and the presence of the cremasteric reflex is the most
valuable clinical finding for ruling out testicular torsion whilst its
absence increases suspected diagnosis [16]. CD study is the first
line diagnostic tool for evaluating testicular perfusion in suspected
testicular torsion cases. In case of testicular torsion, normal echotexture
of the test is strongly suggests its viability. CD study is
both highly specific and sensitive in diagnosing torsion as well as
other pathologies that can cause the acute scrotum. CD findings
consistent with testicular torsion include reduced or absent
testicular blood flow and parenchymal heterogeneity compared
with the contralateral testis [17]. It has a prognostic value as well.
Other investigation tools include near infra-red spectroscopy,
scintigraphy, and scrotal dynamic contrast-enhanced subtraction
MRI but these are always not available and time consuming too.
Differential diagnosis of acute scrotum includes most
commonly scrotal trauma where patient usually gives history of
blunt or penetrating trauma followed by swelling, tenderness, or
ecchymosis. Hematocele may be present. Testicular torsion needs
high index of suspicion because of its dreaded outcome in which
patient experiences severe acute pain that begins to diminish after
6 hours. Abdominal pain, nausea, or vomiting may be present. Color
Doppler scrotal ultrasound shows absence of any intratesticular
vascularity. Epididymo-orchitis usually presents as more gradual
and progressive onset of pain. History of urinary tract infection or unprotected sexual intercourse may be present. Color Doppler
scrotal ultrasound may show hypervascularity and enlargement
of the epididymis with normal or increased testicular blood flow.
Torsion of appendages presents as hard tender nodule, sometimes
visible through the skin in the upper pole, commonly known as
“blue dot sign”. Other rare causes are summarized in Table 1 [18].
Testicular torsion is a true surgical emergency requiring
early surgical intervention for successful salvage. The decision for
orchidectomy is made intraoperatively, usually by testicle color
and lack of blood flow. It is a commonly held belief that a testicular
torsion for more than 6 hours is difficult to salvage. If treated within
6 hours of the presenting pain, there is a good chance of saving the
affected testicle, as 90–100% of the testicles would be saved. If
treated within 6–12 hours, 20–50% of the testicles would be saved,
and if treated within 12–24 hours, 0–10% of the testicles would be
saved [18].
In confirmed cases of testicular torsion immediate prophylactic
fixation of the opposite testis is highly recommended. But contrary
to this if severe necrosis of the twisted testis sets in, the prophylactic
fixation of the opposite normal testis should be postponed until
ipsilateral wound healing is complete. We did the same in our case
and follow up CD study revealed normal left testis echo-texture and
vascularity (Figure 4).
Conclusion
Testicular torsion leading to orchidectomy is a major mental and physical trauma to the patient and his family. Associated subfertility with the one sided orchidectomy, causes further apprehension in patient’s life. Sometimes misleading history and examination delay the correct diagnosis in early phase. Patients in our country usually do not report to specialist in first instance and take consultation to their family physician that unnecessarily losses valuable time. Therefore, we recommend high index of suspicion for the early diagnosis and timely treatment to save the affected testicle.
Acknowledgements
None
Conflict of Interest
None
References
- Delasiauve LJF (1840) Late descent of the left testicle, misdiagnosed as strangulated hernia [in French]. Rev med franc et etrang 1: 363-375.
- Lauenstein C (1894) Testicular torsion [in German]. Sammlung Klin Vortr 92: 1.
- Colt GH (1922) Torsion of the hydatid of Morgagni. Brit J Surg 9: 464.
- Sharp VJ, Kieran K, Arlen AM (2013) Testicular torsion: diagnosis, evaluation, and management. American Family Physician 88(12): 835-840.
- Anderson JB, Williamson RC (1988) Testicular torsion in Bristol: a 25-year review. Br J Surg 75: 988-992.
- Ibrahim Alnadhari, Ausama Abdulmuhsin, Omar Ali, Ahmad Shamsodini, Morshed Salah, et al. (2019) Case Reports in Urology. P. 3.
- Marcozzi D, Suner S (2001) The nontraumatic, acute scrotum. Emerg Med Clin North Am 19: 547-568.
- Kamal Z Shaeer, Osama K Shaeer, Mohamed W Ragab (2016) Testicular torsion in adolescents. Human Androl 6: 79-85.
- Grace S Hyun (2018) Testicular Torsion. Rev Urol 20(2):104-106.
- Visser AJ, Heyns CF (2003) Testicular function after torsion of the spermatic cord. BJU Int 92: 200-203.
- Galejs LE (1999) Diagnosis and treatment of the acute scrotum. Am Fam Physician 59: 817-824.
- Sparks JP (1971) Torsion of the testis. Ann R Coll Surg Engl 49: 77-91.
- Skoglund RW, McRoberts JW, Ragde H (1970) Torsion of the spermatic cord: a review of the literature and an analysis of 70 new cases. J Urol 104: 604-607.
- Jefferson RH, Perez LM, Joseph DB (1997) Critical analysis of the clinical presentation of acute scrotum: a 9-year experience at a single institution. J Urol 158 (P2):1198-1200.
- Cass AS, Cass BP, Veeraraghavan K (1980) Immediate exploration of the unilateral acute scrotum in young male subjects. J Urol 124: 829-832.
- Rabinowitz R (1984) The importance of the cremasteric reflex in acute scrotal swelling in children. J Urol 132: 89-90.
- Waldert M, Klatte T, Schmidbauer J (2010) Color Doppler sonography reliably identifies testicular torsion in boys. Urology 75: 1170-1174.
- Ahmed M Al-Kandari, Elijah O Kehinde, Salah Khudair, Hamdy Ibrahim, Mohammed S ElSheemy, et al. (2017) Intermittent Testicular Torsion in Adults: An Overlooked Clinical Condition. Med Princ Pract 26: 30-34.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...