
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Review Article(ISSN: 2643-6760) 
Surgical Treatment of Severe Early Onset Scoliosis (Idiopatic and Associated with Rare Diseases) Volume 5 - Issue 5
Tiziana Greggi*
- Head Department of Spinal Deformity Surgery, Rizzoli Orthopaedic Institute, Bologna Italy
Received: August 29, 2020; Published: September 10, 2020
Corresponding author: Tiziana Greggi, Head Department of Spinal Deformity Surgery, Rizzoli Orthopaedic Institute, Bologna Italy
DOI: 10.32474/SCSOAJ.2020.05.000222
Abstract
Background: Early-onset scoliosis (EOS) is defined as a spinal deformity which occurs clinically before the age of 5 years. It can be divided into idiopathic, neuromuscular/syndromic, and congenital etiologies. Many patients may have congenital spinal malformations. Others have severe scoliosis, rapidly evolving , which occurs early as a phenotypic feature of rare diseases with major comorbidities or serious health problems. Treatment of non-idiopatic spine deformities in young children is very demanding. Rare syndromes are various clinical conditions, heterogeneous in terms of clinics but associated with spinal deformities in a large percentage of cases. Scoliosis is the most common early onset deformity, sometimes present at birth and often rapidly evolving.
Methods: The literature on the treatment of EOS was summarized, in addition to our experience.
Results: Conventional management tools, such as bracing and fusion, are not always effective. The natural syndromic scoliosis is highly dependent on the natural history of the underlying disorder. Scoliosis often involves the life of children early, creating situations of discomfort and isolation, making it difficult to treat the problem and sometimes opening the way to difficult and ineffective paths.
Conclusion: While lack of treatment has been shown to lead to increased mortality, extensive early definitive fusion may lead to thoracic insufficiency. There are a number of surgical techniques to treat severe and developmental spine deformities (eos) without the need for fusion to control growth and delay definitive surgery with fusion. Delaying definitive surgery and the use of growing instrumentation may provide benefit in maintaining pulmonary health.The genetic and molecular study of syndromic diseases associated with rapidly evolving scoliosis may lead to early diagnosis. Even the study of idiopathic scoliosis (certainly of a polygenic nature) will help to deal with the pre-symptomatic situation and better control the severity of the evolution.
Clinical relevance: Multidisciplinary collaboration with translational research will bring more specialized fields closer to new knowledge on on severe early onset scoliosisis associated with rare diseases.
Introduction
Early onset scoliosisis (EOS) is defined as scoliosis diagnosed before age five (Figure 1A& 1B). It can be classified into idiopathic, neuromuscolar/syndromic and congenital etiologies. These patients may have congenital spinal malformations, associated with rare diseases with thoracic malformations, such as fused or missing ribs, neuromuscular syndromes with severe breathing difficulties; but they may also have normal vertebrae formation as idiopathic in childhood. It is an infrequent pathology: the incidence of idiopathic scoliosis is 1.5% and childhood idiopathic scoliosis accounts for 4% of this population. However, early-onset scoliosis is an important health issue. These children develop spinal deformities at a young age and, if not treated, are at risk of rapid progression of the deformity, with impaired physiological growth, aesthetic appearance and especially lung failure. It is reported that, in patients with untreated scoliosis, the mortality rate increases. This occurs more frequently in scoliosis with childhood onset (first 5 years of life), followed by juvenile scoliosis (6 to 10 years), mainly due to respiratory failure. Eos often leads to severe deformities at an early age. Clinically, most of them are deformities of the spine with double main curves and some have significant thoracolumbar hyperkyphosis [1-5] (Figures 2A-2D).
Figure 1A: F 3 years: severe congenital scoliosis in a rare disease (epiphyseal spondyle dysplasia): clinical picture.
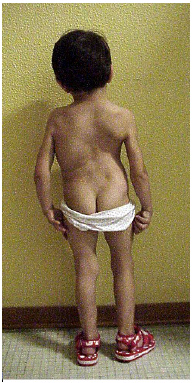
Figure 1B: F 3 years: severe scoliosis in a rare disease (epiphyseal spondyle dysplasia): imaging 3D CT.
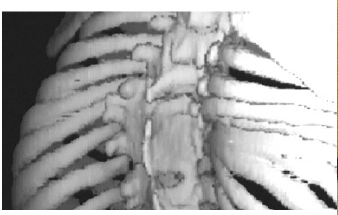
Figure 2C:F 26 months: severe idiopathic infantile scoliosis, post-op radiographic picture. Instrumentation with a magnetic extendable bar.

Figure 2D: F 26 months: severe idiopathic infantile scoliosis, clinical appearance 3 days post-op. after intrevento through mini access.

The Treatment
There are no guidelines for treatment. Most clinicians, in children with mild deformities presenting non-congenital progressive curves, are limited to observation, prescription of physical activity or treatment with brace. Unfortunately it is known that the treatment with orthopedic braces and plaster casts in the treatment of congenital and neuromuscular scoliosis is not effective. This is especially true for those patients with a costo-vertebral angle (Metha angle)> 20°, indicative of a highly progressive curve. The orthopedic corset is commonly used for minor angular curves in the 20° to 30° Cobb range. Treatment with orthopedic corsets requires prolonged use, especially in patients with early scoliosis, and effectiveness often depends on the collaboration of patients and families. In many cases, the orthopedic corset is not accepted or is poorly tolerated, especially when small patients with proximal thoracic curves require the use of a tall Milwaukee type corset [5-8].
Vertebral Fusion
Definitive early fusion (or vertebral arthrodesis) has been
advocated in the past for children with severe progressive scoliotic
curves and particularly for congenital ones. However, there is a
growing consensus that early spinal fusion produces (excluding
very selected congenital deformities) adverse pulmonary
consequences [9]. Most spine surgeons who are experienced
in scoliosis now use fusion as a last resort in pediatric patients.
Also examined in the literature, the long-term results of fusion in
patients with early scoliosis showed that from 37.2% to 39.3% of
cases it was necessary to re-intervene for the progression of the
deformity. This has also occurred in some patients treated with
anterior and posterior fusion during growth (to theoretically
achieve circumferential stability) [10,11]. In addition to the failure
of fusion to control spinal deformity, fusion can have negative
consequences on the overall growth of the child. Prof. A. DiMeglio
has performed numerous studies on spinal growth and has verified
that the fastest period of spinal growth occurs in the first five years
of life, when the spine increases by 50% of its length. It was also
found that between the ages of five and ten, the spine continues to
grow, albeit at a slower rate. The height of the thoracic spine is on
average 11 cm in the newborn, 18 cm from the age of five and 22 cm
at the age of ten [12].
All of this makes it clear why treating early scoliosis with spinal
fusion in a five-year-old child can result in a loss of spinal growth
of more than 12.5 cm. Additionally, the presence of congenital rib
fusions associated with congenital scoliosis in growing children
can lead to arrested lung development. This leads to chest failure
syndrome, or the inability of the chest to sustain normal breathing
[13,14].
Pulmonary function has been observed in patients who have
undergone early spinal fusion for scoliosis, and inhibition of normal
thoracic growth was found. The normal development of the lungs
in children is determined, in fact, by an increase in the number
of alveoli in the first years of life and an increase in lung volumes
up to adolescence [15,16]. For this reason, surgery with definitive
arthrodesis of the spine at this age can create a great limitation in
lung development [17-24].
Growing Rods To address the limitations of the spine or fusion
for early scoliosis, growth-friendly implant 0073 have long been
developed. The instrumentation techniques initially included those
of the last century systems such as the Harrington system (widely
studied and used as an extendable bar by the Italian Masters
Marchetti and Faldini), that of Cotrel-Dubousset or Luque. More
recently, the friend and colleague Pof. B. Akbarnia (San Diego Center
of Spinal Disorders, University of California, former president of
SRS) disseminated the technique of the dual growing rod (first
mechanical then magnetic control) [25,26]. The mechanical dual
growing rod system (which we have been using for over 10 years)
consists of 2 extendable bars that are applied (according to our
personal technique: via a minimally invasive subfascial route) to a
spinal segment with deformity, where no fusion. The anchors for
the bars are only at the proximal and distal part of the segment,
with hooks or pedicle screws. Distraction of the bars for lengthening
over time occurs with minimally invasive surgical access, usually
every six to eight months. Once maximum spinal growth or skeletal
maturity is reached, the final fusion surgery is performed. With this
approach, the stretchable bars control the progression of the spinal
deformity and gradually correct the deformity.
Vertical expandable prosthetic titanium rib (VEPTR) When the
main deformity is not the spinal one, but is already associated with
an important thoracic defomity in the pediatric age, a specific spinocostal
device VEPTR (Vertical Expandable Prosthetic Titanium),
developed by R. Campbell in 2004, can be used. VEPTR is then
surgically lengthened with planned measures such as the growing
rod. Clearly, a treatment path with extendable systems is very
demanding for the patient and the family, especially for scheduled
repeated surgeries, to be added to unscheduled ones, caused by
mechanical failures (mobilization and breakage of the bars) [27-
29]. The need of repeated surgery under general anesthesia, for the
growing- rods and VEPTR, is a major drawback. A high number of
operations determines a greater number of anesthetic and surgical
complications. In addition, the mechanical extending systems
technique is associated with various socioeconomic concerns,
including longer periods of hospitalization and more time away
from school for the child and time away from work for the parents.
Repeated operations, hospitalization, and the appearance of a
cosmetically unacceptable surgical scar can also affect the child’s
psychological well-being [30].
Magnetically Controlled Growing Rods (MGR)Due to the
aforementioned limitations related to the use of mechanical extendable bars, technological development in the last decade has
led to the construction of systems that allow lengthening without
surgery. It is a system that reproduces the effectiveness of the
mechanical growing rod, controllable by an external magnet. This
procedure eliminates frequent hospitalizations of young children
and frequent interventions under general anesthesia, thus reducing
the complications of wounds, and psychological and socio-economic
problems (Figure 1). Stretching is performed in clinics with the
patient awake in a few minutes, on average every 2 months [31-
33]. The negative aspect of the magnetic system, at the moment, in
addition to the cost of the implant is the contraindication to be used
in patients who need high intensity MRI controls (for example for
myeloradicular malformations associated with scoliosis). However,
there are studies that have shown that there are no harmful effects
of MRI on MCGR and even head and neck imaging for distortion of
acquired images [34].
Conclusion
Early onset scoliosis is a difficult challenge. These patients are young with significant growth potential. Therefore, due to this scoliosis they can develop progressive deformities, with extremely negative consequences on their aesthetic-functional and cardiopulmonary appearance. Treatment of non-idiopatic spine deformities in young children is very demanding. Rare syndromes are various clinical conditions, heterogeneous in terms of clinics but associated with spinal deformities in a large percentage of cases. Scoliosis is the most common early onset deformity, sometimes present at birth and often rapidly evolving. Conventional management tools, such as bracing and fusion, are not always effective. Additionally, fusion can also cause significant inhibition of normal spinal and thoracic growth [35-39]. Extendable bars are currently the substantial treatment of early scoliosis with the ability to allow for periodic distractions to allow for growth. However, the need for repeated interventions is associated with an exponential increase in complications. With the development of the magnetic extendable system, non-invasive stretches can be performed, reducing the need for frequent interventions and consequently the aforementioned negative aspects for children and parents. However, as with any new technology, more studies are needed to further reduce complications and improve outcomes in children undergoing treatment for early-onset scoliosis [40,41]. Scoliosis often involves the life of children early, creating situations of discomfort and isolation, making it difficult to treat the problem and sometimes opening the way to difficult and ineffective paths. Confronting with other experts and discussing the state of the art of super-specialized pathologies is always a constructive scientific activity. I believe that providing information to patients and families, to other doctors of other specialist addresses, can be an added value for our conferences. The growing systems are good devices which have proved effective in the treatment of early onset scoliosis associated with rare syndromes, when deformities are very aggressive on account of the peculiar features of the syndromes and, subsequently, are difficult to be controlled conservatively. Both clinical and instrumental evaluation performed specifically for each patient were of the utmost importance, since the peculiar features of each syndrome had to be assessed together with the common characteristics of scoliosis shared by all patients. PFR evaluates the young patients’ life quality indirectly; cardio-US and abdominal US are useful in the study of visceral malformations; brain and spine MRI can detect spinal cord malformation, that is to say contraindications to surgery, and is mandatory for thorough preoperative planning. The indication for traditional Growing Rod, or Magnetic rod, rather than VEPTR should be given according to patient’s age and considering the presence of thoracic hyper kyphosis or chest deformities. Multidisciplinary collaboration with translational research will bring more specialized fields closer to new knowledge on scoliosis and in particular on severe early onset ones. The genetic and molecular study of syndromic diseases associated with rapidly evolving scoliosis may lead to early diagnosis. Even the study of idiopathic scoliosis (certainly of a polygenic nature) will help to deal with the pre-symptomatic situation and better control the severity of the evolution. The use of the most modern “Imaging” technology, such as dynamic MRI for the study of the thorax, will take us a step forward for the correct assessment of thoracic involvement in eos. Innovative surgical techniques have brought important positive changes in the treatment of severe scoliosis. Even the “non fusion” techniques are currently a viable way for the treatment of eos. However, we must not be discouraged, because complications are still significant. This situation , as Prof Akbarnia says, suggests what happened at the initial time of the “organ transplants” [42]. A lot of effort must be made to improve results, aggregating strengths and experiences with national and international collaborations [43,44].
References
- Campbell RM (2009) Spine deformities in rare congenital syndromes: clinical issues. Spine 34: 1815-1827.
- Karol, Lori A (2019) The Natural History of Early-onset Scoliosis Journal of Pediatric Orthopaedics 39: S38-S43.
- Johnston CE (2011) Early onset scoliosis: editorial comment. Clin Orthop Relat Res 469(5): 1315-1316.
- Scott JC, Morgan TH (1955) The natural history and prognosis of infantile idiopathic scoliosis. J Bone Joint Surg Br 37: 400-413.
- Stefano Giacomini, Tiziana Greggi, Elena Maredi, Mario Di Silvestre, Francesco Vommaro, et al. (2017) Treatment of early onset scoliosis associated with rare diseases 2nd World Congress on Rare Diseases and Orphan Drugs.
- Mehta MH (1972) The rib-vertebra angle in the early diagnosis between resolving and progressive infantile scoliosis. J Bone Joint Surg Br 54: 230-243.
- McMaster MJ, Ohtsuka K (2012) The natural history of congenital scoliosis. J Bone Joint Surg.
- Fletcher ND, McClung A, Rathjen KE (2012) Serial casting as a delay tactic in the treatment of moderate-to-severe early-onset scoliosis. J Pediatr Orthop 32: 664-671.
- Dubousset J, Herring JA, Shufflebarger H (1989) The crankshaft phenomenon. J Pediatr Orthop 9: 541-550.
- Goldberg CJ, Moore DP, Fogarty EE (2002) Long-term results from in situ fusion for congenital vertebral deformity. Spine 27: 619-628.
- Chang DG, Kim JH, Ha KY (2015) Posterior hemivertebra resection and short segment fusion with pedicle screw fixation for congenital scoliosis in children younger than 10 years: greater than 7-year follow-up. Spine 15: E484-E491.
- Dimeglio A, Bonnel F (1990) Le rachis en croissance. Springer, Paris.
- Yaszay B, O’Brien M, Shufflebarger HL (2006) Efficacy of hemivertebra resection for congenital scoliosis.
- Bollini G, Docquier PL, Viehweger E (2006) Lumbar hemivertebra resection. J Bone Joint Surg Am 88: 1043-1052.
- Campbell RM, Smith MD, Mayes TC (2003) The characteristics of thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. J Bone Joint Surg Am 85: 399-408.
- Burri PH, McDonald JA. (1997) Structural aspects of prenatal and postnatal development and growth of the lung. Lung Growth and Development. New York, NY: Dekker, USA, p. 1-35.
- (1982) Thurlbeck WM. Postnatal human lung growth. Thorax 37: 564-571.
- Day GA, Upadhyay SS, Ho EK (1994) Pulmonary functions in congenital scoliosis. Spine 19: 1027-1031.
- Goldberg CJ, Gillic I, Connaughton O (2003) Respiratory function and cosmesis at maturity in infantile-onset scoliosis. Spine 28: 2397-2406.
- Karol LA, Johnston C, Mladenov K (2014) Pulmonary function following early thoracic fusion in non.
- Winter RB, Lonstein JE (2009) Ultra-long-term follow-up of pediatric spinal deformity problems: 23 patients with a mean follow-up of 51 years. J Orthop Sci 14: 132-137.
- Phillips JH, Knapp DR, Herrera-Soto J (2013) Mortality and morbidity in early-onset scoliosis surgery. Spine 38: 324-327.
- Akbarnia BA, Pawalek JB, Cheung KM (2014) Traditional growing rods versus magnetically controlled growing rods for the surgical treatment of early-onset scoliosois: a case-matched 2-year study. Spine Deform 2: 493-497.
- Johnston CE, Tran DP, McClung A (2017) Functional and radiographic outcomes following growth-sparing management of early-onset scoliosis. J Bone Joint Surg Am 99:1036-1042.
- Akbarnia BA (2007) Management themes in early onset scoliosis. J Bone Joint Surg Am 89(25): 42-54.
- Marchetti PG, Faldini A (1978) “End Fusion” in treatement of some progressive or severe scoliosis in childhood or early adolescence. Orthop Trans 2: 271.
- Campbell RM, Hell-Vocke AK (2003) Growth of the thoracic spine in congenital scoliosis after expansion thoracoplasty. J Bone Joint Surg Am 85: 409-420.
- Campbell RM, Smith MD, Mayes TC, Mangos JA, Willey-Courand DB, et al. (2003) The characteristics of thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. J Bone Joint Surg Am 85: 399-408.
- Campbell RM, Smith MD, Hell-Vocke AK (2004) Expansion thoracoplasty:the surgical technique of opening-wedge thoracostomy.Surgical technique. J Bone Joint Surg Am 86(A): 51-64.
- Greggi T, Lolli F, Di Silvestre M (2012) Complications incidence in the treatment of early onset scoliosis with growing spinal implants. Stud Health Technol Inform 176: 334-337.
- Bess S, Akbarnia BA, Thompson GH (2010) Complications of growing-rod treatment for early-onset scoliosis: analysis of one hundred and forty patients. J Bone Joint Surg Am 92(15): 2533-2543.
- Klyce W, Mitchell SL, Pawelek J (2020) Characterizing Use of Growth-friendly Implants for Early-onset Scoliosis: A 10-Year Update. J Pediatr Orthop 40(8): e740-e746.
- Upasani VV, Parvaresh KC, Pawalek JB (2016) Age at initiation and deformity magnitude influence complication rates of surgical treatment with traditional growing rods in early-onset scoliosis. Spine Deform 4: 344-350.
- Budd HR, Stokes OM, Meakin J (2016) Safety and compatibility of magnetic-controlled growing rods and magnetic resonance imaging. Eur Spine J 25: 578-582.
- Pehrsson K, Larsson S, Oden A (1992) Long-term follow-up of patients with untreated scoliosis: a study of mortality, causes of death, and symptoms. Spine 17: 1091-1096.
- Phillips JH, Knapp DR, Herrera-Soto J (2013) Mortality and morbidity in early-onset scoliosis surgery. Spine (Phila Pa 1976). 38: 324-327.
- Thorsness RJ, Faust JR, Behrend CJ (2015) Nonsurgical management of early-onset Scoliosis. J Am Acad Orthop Surg 23: 519-528.
- Bakaloudis G, Lolli F, Di Silvestre M (2011) Thoracic pedicle subtraction osteotomy in the treatment of severe pediatric deformities. Eur Spine J 20(1): S95-S104.
- Thompson GH, Lenke LG, Akbarnia BA (2007) Early onset scoliosis: future directions. J Bone Joint Surg Am 89(1): 163-166.
- Vitale MG, Gomez JA, Matsumoto H (2011) Variability of expert opinion in treatment of early-onset scoliosis. Clin Orthop Relat Res 469:1317-1322.
- Tis JE, Karlin LI, Akbarnia BA (2012) Early onset scoliosis: modern treatment and results. J Pediatr Orthop 32: 647-657.
- Akbarnia Behrooz A, Yazici, Muharrem Thompson (2016) The Growing SpineManagement of Spinal Disorders in Young Children George H. (Eds.).
- Pastorelli F, Di Silvestre M, Plasmati R (2011) The prevention of neural complications in the surgical treatment of scoliosis: the role of the neurophysiological intraoperative monitoring. Eur Spine J 20: 105-114.
- Alvarez AG, Dearn KD, Lawless BM, Lavecchia CE, Vommaro F, et al. (2018) Design and mechanical evaluation of a novel dynamic growing rod to improve the surgical treatment of Early Onset Scoliosis. Materials and Design 155: 334-345.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...






