Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Specific Cases of Urgent Vascular Surgery and Peculiar Characteristics of Bypass Operations Volume 2 - Issue 1
Drozdova EV*
- Department of Surgery, Russia
Received: February 05, 2019; Published: February 15, 2019
Corresponding author:Drozdova EV, Department of Surgery, Russia
DOI: 10.32474/SCSOAJ.2019.02.000130
Part I
The Urgent Issues with Grafts Designed for the Hemodialysis
Until March 2018 the work with grafts for the hemodialysis had not posed any complications. Prosthetic devices were removed in connection with urgent suppurate processes or routinely, both when thrombosed grafts existed as a heterogeneous body and when they could prevent carrying out other arterio-venous fistulas. But during only one month – April 2018 there were diagnosed three cases of pulsating hematomas from arterio-venous grafts in the shoulders. In all these cases patients needed surgery. I, myself, performed 2 operations. In one case the patient was hospitalized to another clinic. In the first event the artery and anastomosis with a. braсhialis had a long linear rupture on the back side of the artery. The artery and graft were singled out in both directions from the zone of anastomosis and were taken on the holders. They were clamped but the bleeding did not stop. The situation was complicated by the anamnesis of the patient: there were numerous thromboses of vessels, diabetes type I, polyfactor thrombophilia; so we could not rely on the tourniquet for a long time, moreover the ejection fraction was reduced significantly, and if we had to clamp the artery for any long period then there could be only one way out - the amputation.
The graft turned out to be with multiple big, merging with each other point defects in its middle third part. Then the graft was knotted and extracted. The brachial artery was with ragged edges and a linear defect about 3 centimeters long. The artery could not be linked to its edges by stitching its walls together. That is why the autovein was singled out, the transplant was formed, and artery plastic was performed. Finally, the vessels were functioning properly.
Event II. Some Peculiarities
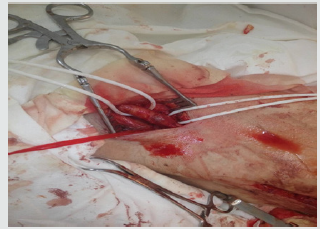
The patient was also with hard anamnesis: ankylosing spondylitis, polyfactor thrombophilia. The proximal part of the graft with the vein anastomosis was thrombosed for several days, because a pressure bandage had been applied because of bleeding from the graft after the session of hemodialysis. The paraprosthetic thrombotic masses were stifling the massive bleeding. With great technical difficulty the zone of artery anastomosis was singled out from the adhesions. The graft was with 2 linear defects: one began from the back wall of anastomosis and ran about 2 centimeters, and the other in its middle part. The graft and the a. brachial were taken in holders. The graft was knotted and extracted. The brachial artery was with ragged edges and a linear defect of about 2.5 centimeters long. And it could not be linked edge-to-edge by stitching the artery walls. So I had to single out a vein, form a patch and the artery plastic was performed. The vessels were functioning properly (Figures 1& 2).
Part II: Throbbing Hematomas Emanating from Femoral and Iliac Arteries
Pulsating hematomas are the consequence of various operative injuries but the most often they are the result of the fracture of atherosclerotic plaques while vessel stenting. But I would like to stress some features of the surgery of these kinds of pulsating hematomas. As usual, patients who are hospitalized for artery stenting are not young people regardless of the localization of their atherosclerotic lesion. The tissues` turgor in this case reduced significantly, that is why if your assistants are not able to make a temporary bleeding stop by pressing the vessels in the wound it will aggravate your work undoubtedly because as a rule there is no place to apply a tourniquet – a hematoma is higher of the inguinal fold and immediately after the skin incision the blood from the wound is rapidly pouring out. The next aggravating circumstance of this work is that the hematoma which existed for several days makes differentiation of the tissues very difficult: they are all graybrown and soldered to each other, but the place of the injury of the artery should be well-visualized All these pulsating hematomas which I operated on were located exactly on the bifurcation of the common, deep and superficial femoral arteries.
The defects of the arteries were always with smooth edges and length of no more than 2 cm and they were joined together by their own tissues. So only the vascular sutures were applied without using any patch. Absolutely otherwise pulsating hematomas manifest in a young organism. I operated on a pulsating hematoma which appeared as a result of the injury of the common iliac artery which occurred during the laparocentesis when the laparoscopic instruments were being introduced into the abdominal cavity. The turgor of the tissues was so high that the diagnosis of pulsating hematoma was difficult. Moreover, the injury of a vessel was suspected by the anesthesiologist, because of the short- term drop in blood pressure. There was no bleeding when we switched to laparotomy till, we entered the retroperitoneal space. Further more despite the defect of common iliac artery on its bifurcation and the length of the rupture over 1.5cm, the retroperitoneal space did not bulge. It took me 15 minutes to single out the artery because the tissues were in fact without hemorrhagic impregnation, and they could be distinguished easily. The defect of the artery was with smooth edges and could be closed without using a patch.
Part III: Particular Specificites of Bypass Operations
I want to make a brief overview of peripheral bypass. Since the grafts were designed for bypass and prosthetic surgery and the new trend in medicine has received a great support, and it is clear there is no reason to single out a vein – the future transplant, and spend time on its allocation, there is no problem with the comparison of the sizes of the vessels and transplants; each graft has its particular size. The overwhelming number of femoral-femoral, femoral-popliteal, femoral-tibial and poplitealtibial bypass operations today is made using grafts. There are common indications for bypass operations but there is only one recommendation to perform an autovenous bypass, that is: do not forget about this wonderful method. That is all. But, somehow, nobody speaks about the superior results of this method, especially in cases of diabetes and complex combined pathology. Previously, I used to apply prosthetic grafts with great pleasure. But later, after some time, patients with artificial prostheses would come back and complain about pain-free walking distance reduction. That was associated with the various causes: non-stop rhythm disorders, the defects of mitral valve, myocardial hypertrophy with the outcome of the cardiomegaly when heart operations cannot be carried out, and also post-stroke states, hypotension, and etc. And the question arises:
what happened with the grafts? Indeed, everything is obvious and simple. The grafts in locations of physiological curves, reduction of size, and compression of major muscle bundles change their cylindrical form - they become “warped” and finally - thrombosed. And I often saw it during the reconstruction operations, when the repeated operations were performed. Everything is simple and satisfies modern science. If there is an obstacle to the blood flow which leads to turbulence, it is the straight way to a thrombosis of the vessels. What is the qualitative difference between autovenous grafts and artificial vascular grafts? The difference is probably that a vein never changes its geometry - cylindrical form, does not cause graft versus host reaction, does not change its intimal lining with the time, and can respond to any treatment. And frankly, if we speak about any treatment, that means that we speak only about native, original tissues, not about grafts – it is impossible to treat polytetrafluoroethylene. And finally, a vein has an apparent advantage which may be crucial for the remote results – it is an angiogenesis.
Each vein possesses this unique natural peculiarity - a tendency to grow new vessels with numerous branches. Actually, due to this process of creating native active anastomoses the arterialized vein graft provides rich blood perfusion to the surrounding tissues. Based on my personal experience in carrying out these operations I want to note that notwithstanding this large tissues’ trauma, especially if we take into account the impossibility of the tunnel extraction of the vein because transplant could be damaged even by medical instruments and palpation, patients as a rule recover after this operation easily enough. We usually use NSAID in postoperative period, and patients are able to sleep, walk and take care of themselves without additional pain-relief medications the next day. If there is an insufficient blood flow, we usually perform a hybrid operation - simultaneous stenting of iliac artery (Figures 3-7).
Conclusion
A. Pulsating hematomas can come from the grafts designed for the hemodialysis due to their fracture, detachment from the anastomoses and as a result of the merger of the punctures defects.
B. In some cases, it requires emergency surgery such as removal of damaged grafts and plastic vessels.
C. Throbbing hematomas resulting from the artery stenting usually localize on the bifurcation with common, deep and superficial femoral arteries. They pose some difficulties while distinguishing the vessels and bleeding control but they do not need special types of artery plastic.
D. Young patients with the pulsating hematomas have a hidden bleeding pattern because of high turgor of the tissues and require a special attention in case when the injury of the vessels is suspected.
E. Bypass operation with using an autovein transplant is the best option for the patients with hard accompanying diseases such as diabetes, different rhythm disorders, defects of mitral valve and hypotension as a result of a various conditions and outcomes of the diseases.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...