Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Research Article(ISSN: 2643-6760) 
Skin Grafts Vs. Local Skin Flaps in Management of Contracted Scar Finger Volume 4 - Issue 5
Khaled Noureldin, Ahmed Shalaby* and Marwa Badawi
- Assistant lecturer at General surgery department, Faculty of medicine, Cairo University Hospitals, Egypt
Received: April 22, 2020; Published: May 04, 2020
Corresponding author: Ahmed Shalaby, Assistant lecturer at General surgery department, Faculty of medicine, Cairo University Hospitals, Egypt
DOI: 10.32474/SCSOAJ.2020.04.000200
Abstract
Purpose: In our study, we reviewed the outcome of using skin grafts and different regional flaps of the hand in order to correct flexion contractures of the Proximal Interphalangeal (PIP) joints of fingers. In both techniques, vigorous postoperative exercises were advised for an interval of time between 3-6 months.
Patients and Methods: 16 patients were included in our study. All the scar tissue was excised, and the resultant raw area was covered. In Group A consisting of 8 patients, skin grafts were used. Split thickness grafts were selected in 3 cases and full thickness grafts in 5 cases. While in group B, Z-plasty and Cross finger regional flaps were used in 4 cases per each flap. The cause of the contracture was thermal burn in 8 patients, mechanical trauma in 7 cases, and a case of contracture secondary to dupytrene’s disease. The mean follow-up period was 6 months.
Results: The mean flexion contracture/further flexion in the joints were improved markedly at the last follow-up. More extension was gained by exercising after the operation. Near full ROM was achieved in 15 cases with strong hand grip and cosmetic satisfaction. There were no major complications.
Conclusion: Wise selection between different skin grafts and regional skin flaps is important, in order to achieve best outcome in managing finger contractures and gain satisfactory ROM. Choosing the best reconstruction method depend on the size, extent and depth of the raw area. Exposure of the deep structures is an indication to use skin flaps over grafts. Vigorous extension exercise is mandatory to have the best results.
Keywords: Flexion contracture, finger, surgical release, skin grafts, regional skin flap, Vigorous extension exercise
Introduction
The Hand is a very vital part of the human body. A full
functioning hand should be supple (moving with ease) and sensate.
Hand injuries represent 5-10% of the A&E visits with a risk of
serious handicap as an outcome that will in turn affect the quality
of life for the patient. Thus, there should be good understanding of
the hand anatomy and mechanism of its function. It is important
to do proper initial physical examination and take wise decision
regarding the timing and method of reconstruction [1].
Longstanding and severe flexion contractures of the proximal
interphalangeal (PIP) joint of fingers significantly impair hand
function. Several anatomical structures, including the skin layers,
long flexors of the hands, palmar plate, and collateral ligaments,
become foreshortened. Usually, surgery is required to regain the
hand function. The human body is liable to different modes of
injury; penetrating, blunt and thermal. The outcome of the healing
process results in scar tissue with migration of specialized cells into
the wound site [2]. Hand injuries account for 10% of the hospital
trauma area. Lacerations contribute to the vast majority by (45%),
followed by contusion (30%), then fractures and infections by
20% and 5% respectively. Contractures are defined as a chronic
deformity with inability to perform full range joint movement [3].
The goal of reconstruction is maximum restoration of the
full hand function with cosmetic acceptance after excision of
the contracting scar. The aim of our work is to restore the hand
function with cosmetic satisfaction of the surgical outcome after
the excision of the scar tissue and achieve full functioning mobile interphalangeal and metacarpophalangeal joints with adequate
strength to resist the forces of other fingers. Plus, correcting the
posture of the fingers with a wide web space and the intrinsic
muscles to aid comprehension [4]. Wide range of surgical methods
have been assigned to cover the raw area left after excising the
scar tissue ,and reconstruct the finger functions after flexion
contractures of the PIP joints.
These techniques can be divided in to 2 groups; different
thickness-skin grafts and locally used skin flaps. Recently, some
surgeons have achieved accepted outcomes by utilizing a gradual
distraction using an external fixator to fix flexion contracture
secondary to traumatic injuries. However, they excluded patients
with flexion contractures combined with scar tissue around the
joints. However, in these patients, surgery is mandatory in order
to restore function and the raw gap should be covered with
stable skin to prevent recurrence [5]. The aim of this study was to
evaluate the results of both main techniques (grafts and regional
flaps) after excision of contracted tissue, followed by strong course
of postoperative extension exercise in order to gain of adequate
degree of extension and range of movement (ROM).
Materials and Methods
A prospective study was done; it included 16 patients presented to the plastic outpatient clinic with contract fingers were managed over one year from the 1 September 2015 to 1st of September 2016, at Cairo University hospital. The average interval of time for their presentation in clinic was ranged one year to two years from the primary injury. They were 9 males and 7 females .8 of them came after thermal burn, while 7 cases had traumatic lacerations in the hands.one boy, 17 years old had dupytren’s disease as a cause for his flexion contracture. It was notice that the 9 out of 16 patients injured their no dominating hands with percentage 57%, while 43% of the injured their dominant hand. It was found that 7 males were injured in their working field .On the other hand; the seven females got injured during their domestic activities.
Figure 2: The regional accepted functional and cosmetic results in respect to skin elasticity and skin texture and colour.
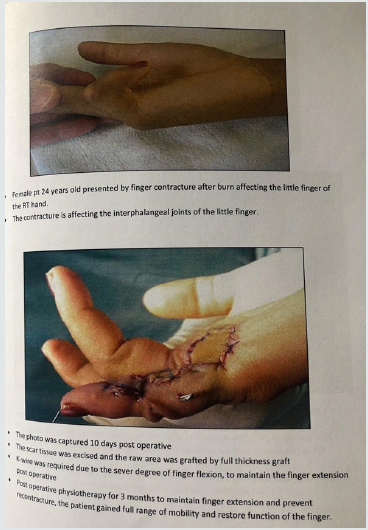
Excision of the scar tissue was done. Then, intraoperative decision for the reconstruction was made based on, the size of the defect, the depth of the tissues affected and the exposure of the underlying structure. Group A, are those 8 patients whose raw areas were covered by grafts, full thickness graft was used in 5 patients and split thickness for the other 3 cases. While in group B, Z-plasty was utilized in 4 patients and cross finger flap was used in the same number of patients.
Results
The results were assessed based on, the cosmetic results,
patient satisfaction, and regain of finger function with full range
of flexion and extension, plus good hand grip. Another factor was
the resultant complications and the graft take and the donor site
complications. In Group A, 5 patients with full thickness graft and
3 patients with split thickness graft, the mean angle of flexion
contractures has improved markedly .It was 68.4 preoperatively and that was improved was 26.8.While the further flexion of the
PIP was 81.2 before the correction ,and this became 91.5 after the
graft application.
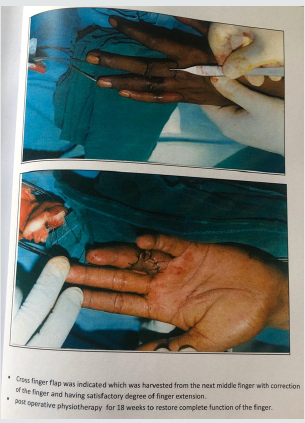
In Group B, Z-plasty was used in 4 cases; the mean angle of
flexion improved from 65.8 to 25.The further flexion was released
from 82 to 95. Cross finger flaps, this was used for the other 4
cases. The mean angle of flexion decreased from 63.4 to 26.5 and
the further flexion from 86.7 to 94. Near full ROM was obtained
in 15 cases. All patients were satisfied with the final results,
functionally and cosmetically .This was achieved by the vigorous
extension exercise for average 6 month period of time. There were
no major complications documented such as neurovascular injury
or recurrence of the pathology, or graft rejection or flap ischemia.
Three patients had mild infections at the recipient site. This
was treated by topical creams and antibiotics for 5 days. A small
hematoma was observed in 1 patient in group B, which healed with
no intervention at postoperative6 days. In group A, one patient
complained of pain an serous discharge at the donor site of full
thickness graft
Discussion
The hand anatomy is very unique with complex sophisticated
moves in order to put the fingers in different positions hands
also must be coordinated in order to perform fine tasks precisely.
The structures that form and move the fingers require proper
alignment and control for full normal hand function. The skin
is the largest organ of the human body. It contributes to 16% of
the total body weight with different forms of functions. On the
other side, wound healing goes through three stages, these are
inflammatory, proliferative and remodeling. Collagen is exposed in
the wound, thus, it activates the clotting cascades which trigger the
inflammatory process and scar formation [6].
Contracture is the inability to perform full range of joint
movement due to abnormal scar tissue formation. This puts the
patients at risk for medical and functional problems and alters
the quality of their lives in a negative aspect. Scar Contracture is
defined as impairment caused by replacement of the skin by a
pathological in scar tissue of insufficient extensibility and length
which in turn hinder the mobility and result in loss of tissue
alignment of the associated joint or the anatomical structures at the
affect region [7]. Finger contracture has many etiologies: Burn and
trauma are the leading causes, While inflammatory factors, such as
scleroderma, rheumatoid arthritis, other autoimmune factors and
tumors contribute as well [7].
As regard to reconstruction after excision of the scar tissue,
the decision is guided by the depth of the found, the surface area
of the defect and the exposure of the deep structures like bones,
tendons and neurovascular bundles [8]. The Skin grafts choice is
influenced by the vascularity of the bed as of at most importance
for the survival of the grafts, with some exceptions as rarely skin
grafts taken to be placed on bones, cartilages or tendons without
the presence of periosteum or perichondrium [9]. Split thickness
graft can tolerate less ideal conditions for survival and it has
much broader range of application. On the other side, it’s fragile
and delicate especially when it is placed over areas with small soft
tissue bulk and it cannot withstand subsequent radiotherapy. They
contract more during the healing phase and tend to be soother and
shiner than normal surrounding skin because of the absent skin
appendages. As for the full thickness grafts, they retain more of the
normal skin characters like color, texture, thickness and undergo
less contraction while healing [10].
The use of the skin flaps not only imports its vascular tissue,
but also allow for the integration of fascial layers between the
mobile gliding structures, which in turn improves the mobility of
the finger due to decreased adhesions formation between the skin
layers and the tendons. Local skin flaps such as Z-plasty and V-Y
plasty are frequently used. But other random pattern flaps were
proven to be useful and provide aesthetically and functionally
excellent outcome. Cross finger flaps can be used in sever flexion
contractures with scarring of the proximal interphalangeal joint of
the fingers followed by postoperative exercise to obtain satisfactory
degree of joint extension. The first dorsal metacarpal artery flap
has its constant anatomy and easy dissection. It has low donor site
morbidity, with god functional and aesthetic outcme.it is considered
the best choice for defects at the proximal phalanx and the proximal
part of the distal phalanx of the thumb (zone 4) [11-14].
In our study, 16 patients were selected with severe flexion
contractures of the PIP joints combined with palmer scarring.
In these patients, tethering by the scar tissue and contractures
of the palmer plates and the collateral ligaments were the main
cause of contracture. Patients were evaluated by history taking,
physical examination, investigation, consent taking, photographs
and surgical intervention. In all patients, surgical excision of the
scar tissue was inevitable to obtain maximal extension of the
joint during the operation [15-18]. The resultant skin defect was
covered by grafts (split thickness/ full thickness) or local flaps. The
decision whether to use grafts or flaps in covering the raw area was
according to the depth of the raw area. When bone, tendons, or the
neurovascular bundle was exposed, the decision was to choose
local skin flaps for covering the defect. Skin grafts were saved for
the shallow defects. The group A of eight patients in which the
defect area was covered by grafts, full thickness graft was used in
five patients, and it was harvested from the inner side of the arm. As
for the split thickness graft, it was used in three patients, and it was
harvested from the anteromedial surface of the thigh. The graft size
ranged from (2-8cm in width and same for length) according to the
defect size. Local skin flaps were used for eight patients in group
B.Z-plasty used in four patients. In the other four patients of group
B, cross finger flap was selected. Postoperative physiotherapy was advised immediately after sutures removal after first week. The
vigorous exercise had a great role in improving the flexion angle.
Thus we believe that early exercise is an adjunct to the surgical
reconstruction in order to obtain excellent clinical exercise [19].
The management of the patients and the decision making
by the clinician, in this series, was affected by the cultural and
environmental background. Most of the patients lived remotely
in peripheral rural areas and they commute long distance to our
tertiary center. Thus the compliance with physiotherapy sessions
and follow up clinics was therefore likely to be poor. Thus, the
surgical option options were with a view to providing a robust
result in a single hospital admission, and urge on the patient to
follow up in outpatient clinic and physiotherapy sessions [20].
It is important to stress on the importance of good adequate
management of thermal injuries in the acute stages by
multidisciplinary team with intensive inputs from the surgeon,
physiotherapist and the occupational therapist.97% of the patients
with superficial burns and 81% of deep dermal injuries will have
normal hand function at the end of their treatment. Adjuncts,
such as electro physical agents, diathermy, ultrasound waves,
transcutaneous electric nerve stimulation, laser therapy and
thermotherapy, can be used. Combination of one or more of these
modalities to the physiotherapy plus patient increased awareness
regarding the regular lifestyle physical exercise , will have positive
impact on the outcome and decrease the risk of recurrence and
possible joint comorbidities.
Conclusion
Conclusion
Skin grafts are the reliable for release of the contractures involving the hand fingers. They offer satisfactory functional and cosmetic outcome with donor site shows minimal morbidities. On the other side, Local skin flaps are excellent for finger contractures that affect deeper tissues and the excision exposes bones, tendons and neurovascular bundles. The regional accepted functional and cosmetic results in respect to skin elasticity and skin texture and color. But the risk of complications and its severity are much higher than those for skin grafts. It is also highly recommended to add postoperative physiotherapy exercise to gain the best outcome.
References
- Diao E, Eaton RG (1993) Total collateral ligament excision for contractures of the proximal interphalangeal joint. J Hand Surg Am 18: 395-402.
- Houshian S, Chikkamuniyappa C (2007) Distraction correction of chronic flexion contractures of PIP joint: comparison between two distraction rates. J Hand Surg Am 32: 651-656.
- Watson HK, Light TR, Johnson TR (1979) Checkrein resection for flexion contracture of the middle joint. J Hand Surg Am 4: 67-71.
- Chasmar Leslie R (2007) The versatile rhomboid (Limberg) flap. Can J Plast Surg 5(2):67.
- Ulkür E, Acikel C, Karagoz H, Celikoz B (2005) Treatment of severely contracted fingers with combined use of cross-finger and side finger transposition flaps. Plast Reconstr Surg 116: 1709-1714.
- Ghidella SD, Segalman KA, Murphey MS (2002) Long-term results of surgical management of proximal interphalangeal joint contracture. J Hand Surg Am 27:799-805.
- Bayat A, Mc Grouther DA, Ferguson MWJ (2003) Skin Scarring. BMJ 326: 88-92.
- Friedrich JB, Katolik LI, Vedder NB (2009) Soft tissue reconstruction of the hand. J Hand Surg Am 34(6):1148-1156.
- Lorea P, Medina Henriquez J, Navarro R, Legaillard P, Foucher G (2007) Anterior tenoarthrolysis for severe flexion contracture of the fingers (the "TATA" operation): a review of 50 cases. J Hand Surg Eur 32: 224-229.Curtis RM (1970) Surgical restoration of motion in the stiff interphalangeal joints of the hand. Bull Hosp Joint Dis 31:1-6.
- Curtis RM (1964) Capsulectomy of the interphalangeal joints of the fingers. J Bone Joint Surg Am 36(A): 1219-1232.
- Curtis RM (1964) Treatment of injuries of proximal interphalangeal joints of fingers. Curr Pract Orthop Surg 23:125-139.
- Gibraiel EA (1977) A local finger flap to treat post-traumatic flexion contractures of the fingers. Br J Plast Surg 30: 134-137.
- Gould JS, Nicholson BG (1979) Capsulectomy of the metacarpophalangeal and proximal interphalangeal joints. J Hand Surg Am 4: 482-486.
- Harrison DH, Newton J (1991) Two flaps to resurface the basal flexioncrease of the finger area. J Hand Surg Br 16: 78-83.
- Houshian S, Gynning B, Schrøder HA (2002) Chronic flexion contracture of proximal interphalangeal joint treated with the compass hinge external fixator. A consecutive series of 27 cases. J Hand Surg Br 27: 356-358.
- Jackson IT, Brown GE (1970) A method of treating chronic flexion contractures of the fingers. Br J Plast Surg 23: 373-379.
- Sprague BL (1976) Proximal interphalangeal joint contractures and their treatment. J Trauma 16: 259-265.
- Harrison DH (1977) The stiff proximal interphalangeal joint. Hand 9: 102-108.
- Brüser P, Poss T, Larkin G (1999) Results of proximal interphalangeal joint release for flexion contractures: midlateral versus palmar incision. J Hand Surg Am 24: 288-294.
- Houshian S, Schrøder HA (2004) Distraction with external fixator for contractures of proximal interphalangeal joints: good outcome in 10 cases. Acta Orthop Scand 75: 225-228.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...