Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Research Article(ISSN: 2643-6760) 
Retrospective Cross-sectional Study of Aortic Aneurysm after Introducing Electronic Health System at King Hussein Medical Hospital Volume 4 - Issue 1
Rami Farraj*
- Department of Internal Medicine, Imperial College, Jordan
Received: November 28, 2019; Published: December 11, 2019
Corresponding author: Department of Internal Medicine, Imperial College, Jordan
DOI: 10.32474/SCSOAJ.2019.04.000178
Abstract
Objective: To evaluate the clinical presentation and current management of aortic aneurysm patients in a tertiary care hospital in Amman, Jordan.
Method: All patients diagnosed with aortic aneurysm at the King Hussein Medical Hospital using the electronic health records (EHR) database Hakeem were evaluated between May 2016 and May 2018. Patients were then categorized according to the time duration between their diagnosis date and definitive treatment into 3 categories: Emergent (treatment on the same day of presentation), urgent (within one week) or elective (scheduled appointment). Definitive treatment was defined as either endovascular repair or open surgical repair.
Results: There were 49 cases of aortic aneurysm cases found in the Hakeem EHR database during that 2-year time interval, of them 92% were male, 94% were above 50 years old, and 61% were smokers. Thoracic cases were 14%, thoraco-abdominal cases were 8% and abdominal cases were 78%. The mean abdominal aneurysm size at presentation was 6.8 cm. Patients that were discovered incidentally with the aneurysm, were 43%. Elective, urgent and emergent groups were not significantly different in frequency. 63% of treated patients had endovascular repair. Nine patients refused to accept the risk of endovascular or surgical treatment. CT angiogram was used in 55% as the first investigation. The mean stay in hospital was 10.7 days, with 2.3 days in ICU and 6.1 days post-operatively.
Conclusion: Our results show the increased risk of aortic aneurysm in male patients above the age of 50 year, especially with a positive smoking history. One third of the patients required same day surgery to avoid immediate mortality. This outlines the late presentation of these cases due to the absence of screening. Hence, we recommend a one lifetime screening abdominal ultrasound for male smokers. Considering the high rate of smoking and other prevalent risk factors for developing aortic aneurysms, more studies are needed to evaluate the ideal age of starting this screening in Jordan. Implementing the electronic health system Hakeem has increased the accessibility and accuracy of research data and has lead to the increased awareness of this important issue.
Keywords:Aortic aneurysm; presentation and screening
Introduction
An aneurysm is a widening or localized dilation that is
permanent and irreversible of a vessel.(1) It is considered
abdominal if sub diaphragmatic and thoracic if supradiaphragmatic.
(1) The normal diameter of the abdominal aorta varies with age,
sex, bodyweight, and decreases progressively from its entry into
the abdominal cavity to the iliac bifurcation [1]. The infrarenal
aorta ranges between 1.5cm and 2.4cm in the elderly group of 65
and 74 years old [2].
Abdominal aortic aneurysm (AAA) is defined as dilatation
that is focal and more than 50% of the normal size of the normal
diameter of aorta, or the size of the aorta is 1.5 times the normal size
of the aorta [3]. Other resources define AAA as a dilatation of three
cm or more of the abdominal aorta [4,5]. If this dilatation involves
all three layers of the aortic wall; it is considered a true aneurysm.
Most aneurysms are fusiform since the whole circumference of the
artery is affected, whereas an aneurysm that includes only a part of
the circumference is termed saccular. An inflammatory aneurysm is characterized by extensive perianeurysmal, retroperitoneal fibrosis
and dense adhesions to adjacent abdominal organs [1].
The prevalence of AAA increases with age. The US experience
showed; it is uncommon in persons younger than 50 years;
however, 12.5% of men and 5.2% of women 74 to 84 years of age
have AAA [4]. There is an increase in the number of diagnosed
cases through screening programs; especially programs that
pursue high risk populations. Many screens showed that AAA is
almost 5% prevalent in men and 1% in women over 60 years old
[6-8]. Deaths due to AAA rupture is around 15,000 per year in the
US population [9], and this showed only aortic rupture as cause
of death, not counting other causes of death due to associated
illnesses. Defined risk factors associated with the development of
AAA are advanced age, male sex, Caucasian race, a positive family
history, smoking, the presence of other large-vessel aneurysms,
and atherosclerosis [10,11]. The key risk factors for aneurysm
rupture include the diameter of aneurysm at first time diagnosis,
progression of aneurysm size, and male gender [12].Treatment of
AAA could be either through an open repair (aorto-bifemoral repair
graft) or through endovascular aortic repair (EVAR). Recent data
showed that EVAR is not cost‐effective compared with open repair
on the long term as noted in European centers [13]. On the short
term, EVAR appeared to be cost‐effective based on the OVER trial,
conducted in USA [13].
Methods
After institutional review board (IRB) approval, the research
protocol was submitted for consideration, comment, guidance
to the ethical committee of Jordanian Royal Medical Services. An
approval was given according to the regulations of the country and
the international standards before the study onset. All patients
diagnosed with aortic aneurysm at the King Hussein Medical
Hospital using the electronic health records (EHR) database Hakeem
were evaluated between May 2016 and May 2018. Retrospective
review of aortic aneurysm data using the electronic health records
(EHR) database Hakeem. Patients with the ICD-9 codes of aortic
aneurysms and its complications; 441.1 to 441.9 from the period of
May 2016 till May 2018, were included in the study. This includes
referred patients from non-military hospitals for treatment at King
Hussein Medical Hospital. The total number was 49 patients.
Patients were classified per sex, age group, site of the aneurysm
(abdominal, thoracic or both). Patients were then categorized
according to the time duration between their diagnosis date and
definitive treatment into 3 categories: Emergent (treatment on the
same day of presentation), urgent (within one week) or elective
(scheduled appointment). Definitive treatment was defined as
either endovascular repair or open surgical repair. Patients were
organized according to their first presenting symptom of diagnosis
into: incidental and symptomatic. Incidental patients presented
with a symptom not related to the aneurysm, e.g. a victim of motorvehicle-
accident. While patients presenting with related symptoms
to the aneurysm were considered symptomatic. The grey area here
was back pain with disc prolapse noted on lumbosacral CT, with an
incidental finding of abdominal aortic aneurysm. This patient was
considered incidental unless the size was more than 5.5cm, and
the patient underwent an urgent or emergent intervention, he was
considered as a symptomatic case. The same was applied for cases
presenting with non-specific abdominal pain.
Results
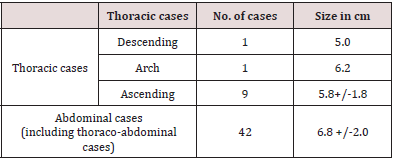
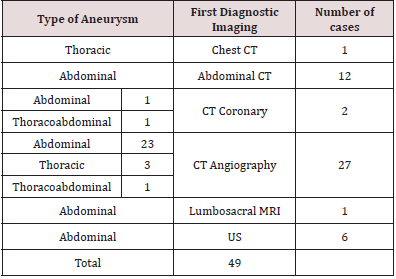
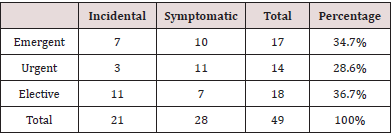
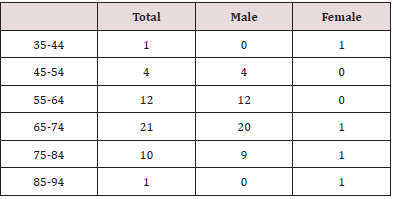
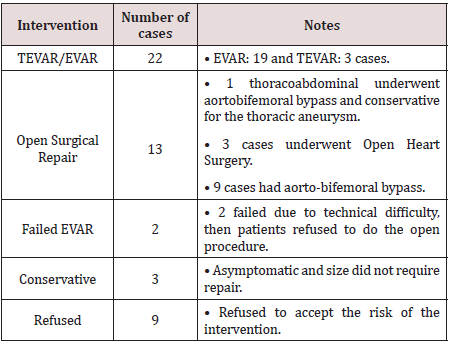
The forty-nine aortic aneurysm cases were as follows; 38 abdominal, 7 thoracic, and 4 thoraco-abdominal. The thoracic cases were as follows: 9 cases had ascending thoracic aorta aneurysm (average size was 5.8 +/-1.7 cm), one case of descending thoracic aorta, size 5 cm, one case of aortic arch aneurysm, size was 6.2cm. Average size of abdominal aortic aneurysm cases 6.8 +/-2.0 cm (Table 1) The imaging used at first diagnosis was as follows; one case first diagnosed with I.V. contrast chest CT (thoracic Aneurysm), 12 cases of abdominal CT (abdominal aneurysm), two cases of Coronary CT, of which 1 was abdominal and 1 had thoracoabdominal aneurysm, 27 cases of CT angiography (23 abdominal, 3 thoracic and one case of both thoracic and abdominal aortic aneurysm). Table 2 Numbers of cases per severity vs. mode of presentation are explained in Table 3. According to the situation by which the patients were diagnosed with aortic aneurysm, whether incidental or symptomatic. 21 cases were incidental (43%) of them, 4 were treated with observation, EVAR: 11, Open repair: 4, Refused: 2 and according to the severity; (elective: 11, emergent: 7, urgent: 3). The patents who were symptomatic 28 patients (57%) and managed as follows;(EVAR: 11, TEVAR:2, Open repair: 6, refused:9), according to severity (7 elective, 11 urgent, and 10 emergent (Table 4).
Table 4: The patents who were symptomatic 28 patients (57%) and managed as follows;(EVAR: 11, TEVAR:2, Open repair: 6, refused:9), according to severity (7 elective, 11 urgent, and 10 emergent.
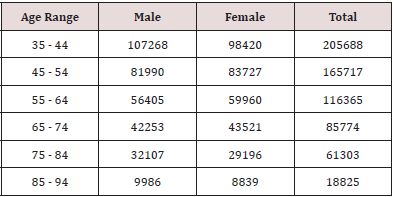
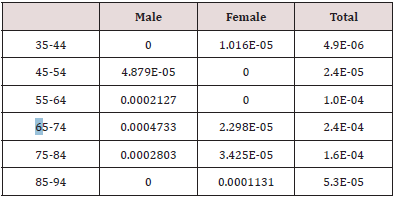
The demographics of the patients were; 45 male (92%) 4 Female (8%), Diabetes; 10 had diabetes (20%) and 39 cases did not (80%), hypertension; 31 cases has it 63%, 18 cases did not have 37%. IHD; 24 has IHD 49%, 25 no IHD 51%. Smoker 30(61%), 19 nonsmoker 39%. For calculating the incidence of aortic aneurysms among the population of patients at our tertiary hospital (King Hussein Medical Hospital), the whole patient population at the hospital were looked up and classified according to the age (Table 5a). Number of aneurysmal cases per age (Table 5b) and calculated age-related incidence (Table 5c). Total number of aneurysmal patients were not calculated as most were on the paper-document binders, hence prevalence was not calculated.
Table 6:A comparison between incidental and symptomatic per the age, medical history of diabetes Ischemic heart disease (IHD) and per social history of smoking.
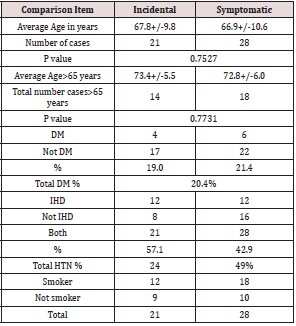
*DM: Diabetes Mellitus, HTN: Hypertension and IHD=Ischemic Heart Disease
The diagnoses used by the doctors according to the ICD code 9 were abdominal aortic aneurysm 57%, thoraco-abdominal aortic aneurysm 2%. Thoracic aortic aneurysm 4% and aortic aneurysm 37%. The age range of patients were; up to 39 years: 2%, 40-49: 4%, 50-64: 29% and more than 65 years old: 65%. The results of the endovascular aortic repair whether abdominal or thoracic were: 22, Open surgical repair: 13, trial of EVAR failed technically: 2, conservative treatment: 3, and refused to take the risk of procedure: 9 cases. A comparison between incidental and symptomatic per the age, medical history of diabetes Ischemic heart disease (IHD) and per social history of smoking (Table 6). ICD codes of the cases per their first presentation diagnosis is mentioned for each group (Table7) and abdominal pain, unspecified site ICD code 789.00, was seen in 17 patients.
Table 7:ICD codes of the cases per their first presentation diagnosis is mentioned for each group.
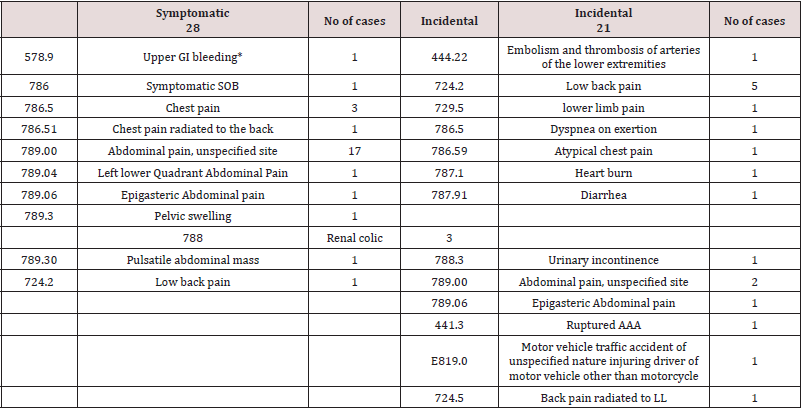
*History of EVAR, complicated with aorto-enteric fistula.
Table 8: Incidental cases were 6.4+/-1.3, elective cases were 5.6+/-1.5, urgent cases were5.8 +/-0.8 and emergent cases were 7+/-1.5 days.
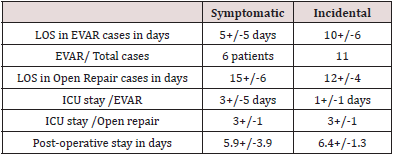
*LOS: length of stay, EVAR: Endovascular aortic repair, ICU: intensive care unit.
Length of stay (LOS) in hospital ranged from 1 to 25 days, with average 9+/-6 days. Symptomatic cases’ length of stay was 9+/-7 days. Average length of stay for the incidental cases was 9 +/-6 days. EVAR: 8+/- 6 days. Two cases of TEVAR averaged stay was 15 (one case was 5 and second was 25 days). Open repair was 13+/- 5days. LOS of stay post operatively was as follows in days; symptomatic cases were 5.9+/-3.9 days, Incidental cases were 6.4+/-1.3, elective cases were 5.6+/-1.5, urgent cases were5.8 +/-0.8 and emergent cases were 7+/-1.5 days (Table 8). Table 9 shows a comparison between elective, urgent and emergent cases. Comparison items are LOS in hospital, LOS ICU admission, LOS post operatively, and number of packed RBC needed for blood transfusion.
Table 9: Shows a comparison between elective, urgent and emergent cases.
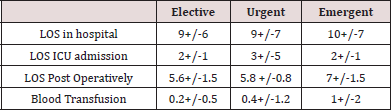
*LOS: length of stay, EVAR: Endovascular aortic repair, ICU: intensive care unit.
Discussion
The prevalence of AAA ranges between 4 and 8 % in screening studies, with predominance male gender [14]. The screened AAA size was generally smaller than 5.5cm. While the incidence of those more or equal to 5.5cm, was prevalent between 0.4 to 0.6% of the screened population [15]. Considering the ICD-10; I71.3 (Abdominal aortic aneurysm, ruptured); I71.4 (Abdominal aortic aneurysm, without mention of rupture); I71.8 (Aortic aneurysm of unspecified site, ruptured); I71.9 (Aortic aneurysm of unspecified site, without mention of rupture), the CDC website shows a crude death rate of ruptured aortic aneurysm of 3.7, 11.0 and 7.1 for the female, male and both respectively in the year 2008 of the age group in years 65 to 74 per 100,000 population. This changed 10 years later (2017) to 2.0, 6.2 and 4.0 respectively. For the period from 2008 to 2017, the crude rate was 2.7, 5.6 and 5.0 respectively [16]. The United States Preventive Services Task Force recommends that men aged 65–75 years who have ever smoked (more or equal 100 cigarettes) should get an ultrasound screening for abdominal aortic aneurysms, even if they have no symptoms [17]. Recognized risk factors whose presence increase the need for screening even more include; male sex, obesity, older age, tobacco use, atherosclerosis, hypercholesterolemia, hypertension, cerebrovascular disease, coronary artery disease, coronary artery disease, history of other vascular aneurysms, first-degree relative with abdominal aortic aneurysm [18]. Surgical intervention by open or endovascular repair is the primary option and is typically reserved for aneurysms 5.5 cm in diameter or greater [18].
The number of patents seen in the military hospitals are around
two million patients of different age and gender. Calculating the
incidence of total patient with aortic aneurysm per the military
hospital patients came out as 2 patients in 10,000 patients of the
age group 65 -75, we believe that this represent a less number than
expected. Prevalence for those more than or equal 5.5cm of the 65
to 74 years old, 8 male cases out of 42 cases whose aneurysmal size
was 7.3 +/- 1.8 cm, percentage of patients was 1.9 per 10,000 male
population. We assume if we screen for AAA in the same population
the prevalence will be higher due to many the many availability of
risk factors in these patient- age group. For example, the prevalence
of smoking is 70.2 % in the Jordanian adult population, in adult
women 10.9% in Jordan, and in adult Arab males is around 51.3%
[19]. In a prospective, population‐based study (Oxford shire, UK,
2002–2014), the incidence and outcome of acute AAA events were
determined. Over the 12‐year period, 103 incident of acute AAA
events occurred in the study population of 92 728. Incidence/100
000/year was 55 in men ages 65 to 74 years but increased to 112
at 75 to 85 and 298 at ≥85, with 66.0% of all events occurring
at age ≥75 years. Incidence at ages 65 to 74 was highest in male
smokers (274), with 96.4% of events in men <75 years occurring in
ever‐smokers. Extrapolating rates to the UK population, using trial
evidence of screening efficacy, the current UK screening program
would prevent 5.6% of aneurysm‐related deaths (315 200 scans/
year: 1426/death prevented, 121/year‐of‐life saved). Screening
only male smokers age 65 and then all men at age 75 would prevent
21.1% of deaths (247 900 scans/year; 297/death prevented, 34/
year‐of‐life saved). By 2030, 91.0% of deaths will occur at age ≥75,
61.6% at ≥85, and 28.6% in women.
Screening programs in the United States and Europe have shown
that 5% of men older than 65 have an occult AAA.(20) Interestingly,
individuals detected with AAA on screening, rarely have an aortic
diameter associated with a short-term risk of aneurysm-related
death (e.g., from rupture). On the other hand, recent data suggest
the coexistence of atheroembolic risk like coronary heart disease
and cerebrovascular ischemic events in the patients with AAA who
were detected by screening. These cardiovascular (CV) events
confer the major increased CV morbidity and mortality burden
[20,21]. Late survival of patients with AAA is significantly lower
than that of age- and sex-matched non-AAA populations, even after
successful AAA repair [22-24]. Patients with AAA, have significantly
higher rates of CV deaths, hospitalizations for atherothrombotic
events in particular revascularization procedures (coronary
angioplasty, carotid surgery, peripheral bypass surgery and new
or worsening PAD [25]. Polyvascular disease is twice as frequent
in patients with AAA as in patients without. Patients with AAA
are more likely to establish symptomatic atherothrombosis in
more than one vascular bed, in addition to AAA [26]. Therefore,
early diagnosing patients with AAA, would prevent not only major
complications of AAA, but can present a key to treat and prevent
atheroembolic vessels diseases.
In an Australian study, Hayter et al, showed that the total
hospital cost of EVAR in the US was $16,631 vs. $14,063 for the
open repair. The increase in total hospital costs was due to a
significant difference in graft costs, which was not offset by reduced
postoperative costs in EVAR compared to the open repair group.
The average follow-up cost per year after EVAR was US $999 [27].
Ruptured AAA repairs are more expensive ($38K) than elective
AAA repairs ($28K), though no difference in length of hospital
stay. A screening program that reduces the incidence of surgery
for ruptured AAA could decrease the average inpatient cost of AAA
repairs [28].
Screening patients younger than 65 and older than 75 years,
is controversial as AAA is a disease of the aging population,
and elderly group should be selected to get a reasonable rate of
recognition. Patients who are older than 75 years diagnosed with
AAA may not be suitable for surgical correction. They may refuse to
accept the risk of the surgery as in 11 patients in our study, or not
fit for general anesthesia and this major surgery. Some differences
in recommending AAA screening, the U.S. Preventive Services Task
Force (USPSTF) recommended a screening ultrasound once in life
for men ages 65 and 75 who ever smoked [29]. The Society for
Vascular Surgery (SVS) recommended screening all men ages 65
years or above, men ages 55 years or above with a family history
of AAA, and women ages 65 years or above with a family history
of AAA or past or present smoking use. (29) Given that two thirds
of acute AAA occurred at ≥75 years of age, screening older age
groups should be considered. Screening nonsmokers at age 65 is
likely to have very little impact on AAA event rates. In our study,
the significant limitation in the clinical presentation is the lack of
consistent documentation in the records of “ex-smoker” status.
Hence, we are unable to establish a localized screening guideline
regarding screening of non-smokers, even though the international
guidelines do not recommend it.
It is worth mentioning, if we start screening for abdominal
aortic aneurysm at age 65 with an abdominal ultrasound as per
other international guidelines, we would be missing a 33% patients
who have either abdominal or thorcoabdominal aortic aneurysm
(14 cases out of 42 cases were at age range from 46 and 64 years)
with size range from 3.5 cm to 9.5 cm with average 6.2cm of
abdominal aortic aneurysm. This means that we would miss 33% of these large aneurysms by that screening if we waited till the age of
65. (Data not mentioned in results section) This seems substantial
and perhaps screening at an earlier age would be warranted in
Jordan.
Conclusion
In conclusion, our results show the increased risk of aortic aneurysm in male patients above the age of 50 year, especially with a positive smoking history. One third of the patients required same day surgery to avoid immediate mortality. This outlines the late presentation of these cases due to the absence of screening. Hence, we recommend a one lifetime screening abdominal ultrasound for male smokers. Considering the high rate of smoking and other prevalent risk factors for developing aortic aneurysms, more studies are needed to evaluate the ideal age of starting this screening in Jordan. Implementing the electronic health system Hakeem has increased the accessibility and accuracy of research data and has lead to the increased awareness of this important issue.
References
- Sakalihasan N, Limet R, Defawe OD (2005) Abdominal aortic aneurysm. Lancet 365(9470): 1577-1589.
- Liddington MI, Heather BP (1992) The relationship between aortic diameter and body habitus. Eur J Vasc Surg 6(1): 89-92.
- Johnston KW, Rutherford RB, Tilson MD, Shah DM, Hollier L, et al. (1991) Suggested standards for reporting on arterial aneurysms. Subcommittee on Reporting Standards for Arterial Aneurysms, Ad Hoc Committee on Reporting Standards, Society for Vascular Surgery and North American Chapter, International Society for Cardiovascular Surgery. J Vasc Surg 13(3): 452-458.
- Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, et al. (2005) Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation 113(11): e463-654.
- Paravastu SC, Jayarajasingam R, Cottam R, Palfreyman SJ, Michaels JA, et al. (2014) Endovascular repair of abdominal aortic aneurysm. Cochrane Database Syst Rev 23(1): CD004178.
- Golledge J, Muller J, Daugherty A, Norman P (2006) Abdominal aortic aneurysm: pathogenesis and implications for management. Arterioscler Thromb Vasc Biol 26(12): 2605-2613.
- Lederle FA, Johnson GR, Wilson SE, Aneurysm D (2001) Management Veterans Affairs Cooperative S. Abdominal aortic aneurysm in women. J Vasc Surg 34(1): 122-126.
- Golledge J, Norman PE (2011) Current status of medical management for abdominal aortic aneurysm. Atherosclerosis. 217(1): 57-63.
- Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, et al. (2006) Heart disease and stroke statistics--2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 113(6): e85-151.
- Chaikof EL, Dalman RL, Eskandari MK, Jackson BM, Lee WA, et al. (2018) The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Sur 67(1): 2-77e2.
- Moll FL, Powell JT, Fraedrich G, Verzini F, Haulon S, et al. (2011) Management of abdominal aortic aneurysms clinical practice guidelines of the European society for vascular surgery. Eur J Vasc Endovasc Surg 41(1): S1-S58.
- Brewster DC, Cronenwett JL, Hallett JW, Johnston KW, Krupski WC, et al. (2003) Guidelines for the treatment of abdominal aortic aneurysms. Report of a subcommittee of the Joint Council of the American Association for Vascular Surgery and Society for Vascular Surgery. J Vasc Surg 37(5): 1106-1117.
- Michaels JA (2014) Long-term cost-effectiveness analysis of endovascular versus open repair for abdominal aortic aneurysm based on four randomized clinical trials 101(6): 623-631.
- Ashton HA, Gao L, Kim LG, Druce PS, Thompson SG, et al. (2007) Fifteen-year follow-up of a randomized clinical trial of ultrasonographic screening for abdominal aortic aneurysms. 94(6): 696-701.
- Von Allmen RS, Powell JT (2012) The management of ruptured abdominal aortic aneurysms: screening for abdominal aortic aneurysm and incidence of rupture. The Journal of cardiovascular surgery 53(1): 69-76.
- Centers for Disease Control and Prevention NCfHSUCoD-oCWOD, released December (2018) Data are from the Multiple Cause of Death Files, 1999-2017, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program.
- Fleming C, Whitlock EP, Beil TL, Lederle FA (2005) Screening for abdominal aortic aneurysm: a best-evidence systematic review for the U.S. Preventive Services Task Force. Ann Intern Med 142(3): 203-211.
- Keisler B, Carter C (2015) Abdominal aortic aneurysm. Am Fam Physician 91(8): 538-543.
- Abdulrahim S, Jawad M (2018) Socioeconomic differences in smoking in Jordan, Lebanon, Syria, and Palestine: A cross-sectional analysis of national surveys. PloS one 13(1): e0189829.
- Powell JT, Greenhalgh RM (2003) Clinical practice. Small abdominal aortic aneurysms. N Engl J Med 348(19): 1895-1901.
- Sukhija R, Aronow WS, Yalamanchili K, Sinha N, Babu S (2004) Prevalence of coronary artery disease, lower extremity peripheral arterial disease, and cerebrovascular disease in 110 men with an abdominal aortic aneurysm. Am J Cardiol 94(10): 1358-1359.
- Hallett JW, Naessens JM, Ballard DJ (1993) Early and late outcome of surgical repair for small abdominal aortic aneurysms: a population-based analysis. J Vasc Surg 18(4): 684-691.
- Johnston KW (1994) Nonruptured abdominal aortic aneurysm: six-year follow-up results from the multicenter prospective Canadian aneurysm study. Canadian Society for Vascular Surgery Aneurysm Study Group. J Vasc Surg 20(2): 163-70.
- Galland RB, Whiteley MS, Magee TR (1998) The fate of patients undergoing surveillance of small abdominal aortic aneurysms. Eur J Vasc Endovasc Surg 16(2): 104-109.
- Al-Zahrani HA, Rawas M, Maimani A, Gasab M, Aba al Khail BA (1996) Screening for abdominal aortic aneurysm in the Jeddah area, western Saudi Arabia. Cardiovasc Surg 4(1): 87-92.
- Baumgartner I, Hirsch AT, Abola MT, Cacoub PP, Poldermans D, et al. (2008) Cardiovascular risk profile and outcome of patients with abdominal aortic aneurysm in out-patients with atherothrombosis: data from the Reduction of Atherothrombosis for Continued Health (REACH) Registry. J Vasc Surg 48(4): 808-814.
- Hayter CL, Bradshaw SR, Allen RJ, Guduguntla M, Hardman DT (2005) Follow-up costs increase the cost disparity between endovascular and open abdominal aortic aneurysm repair. J Vasc Surg 42(5): 912-918.
- Peek KN, Khashram M, Wells JE, Roake JA (2016) The costs of elective and emergency abdominal aortic aneurysm repair: a comparative single centre study. NZ Med J 129(1433): 51-61.
- Zucker EJ, Prabhakar AM (2018) Abdominal aortic aneurysm screening: concepts and controversies. Cardiovasc Diagn Ther 8(1): S108-S17.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...