Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Retroperitoneal Liposarcoma Presenting as Femoral Hernia Volume 7 - Issue 3
Dr Sudarshana, Dr Dattaprasad Samant, Dr Jude Rodrigues and Dr Frazer CS Rodrigues*
- General Surgeon, Department of General Surgery, Goa Medical College, Goa, India
Received: March 27, 2023; Published: April 13, 2023
Corresponding author: Dr Frazer CS Rodrigues, General Surgeon, Department of General Surgery, Goa Medical College, Goa, India
DOI: 10.32474/SCSOAJ.2023.07.000264
Introduction
Liposarcoma is a common type of soft tissue sarcoma [1], which occurs most commonly in the extremities (52%), followed by the retroperitoneum (19%) [2]. Retroperitoneal Liposarcoma is usually asymptomatic until the liposarcoma is large enough to compress the surrounding organs [3]. It is often misdiagnosed due to its rarity and absence of symptoms. Its localization in the fossa femoralis is uncommon and may lead to erroneous interpretation being sometimes clinically indistinguishable from a groin hernia.
Case Report
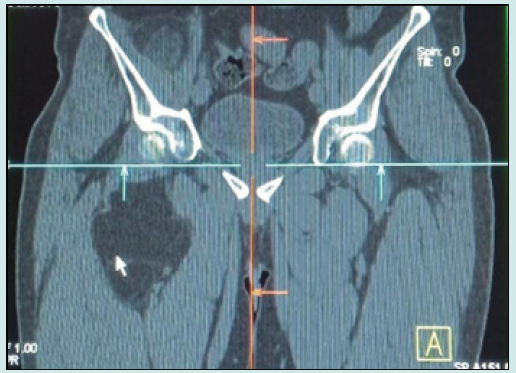
A 49 year old male had come with a right groin swelling, which gradually progressed in size over six months. There was no history of trauma, paresthesia, abdominal pain or altered bowel habits. There was neither significant past nor family history. The patient was normotensive and the general examination was unremarkable. Per abdominal examination revealed a firm, non tender swelling of 5x6 centimeters below the medial aspect of the right inguinal ligament, lateral to pubic tubercle, associated with expansile cough impulse. Genital and per-rectal examination were normal. Examination of other systems revealed no abnormality. Soft tissue ultrasound of the right thigh revealed a well-defined hypoechoic lesion measuring 7.8x4.0x16.8 (APxTRxSI). CT scan revealed an encapsulated mass of fat density in retroperitoneum extending to the thigh and groin surrounding the femoral vessels with foci of calcification with ill-defined, soft tissue component over anterosuperior aspect of the mass (Figure 1).
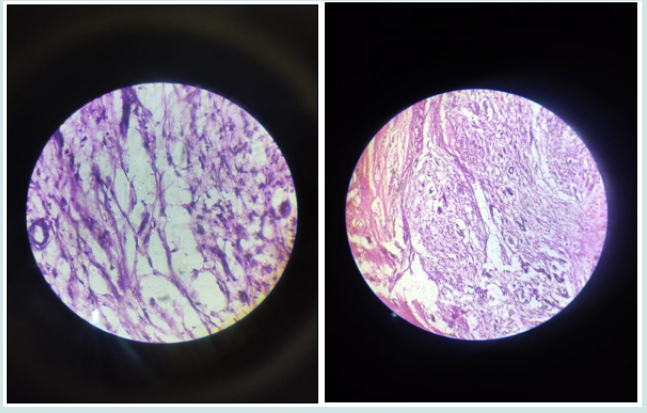
The patient was taken for excision of the mass under general anesthesia. Intraoperatively 8x10cm lipomatous tumor, extending from psoas to mid-thigh with multiple extensions in the groin noted with surface bossellations. The tumor was excised with an intact capsule. No local infiltration noted (Figures 2 and 3). Postoperative period was uneventful and the patient was discharged on postoperative day 5. On follow up histopathology was suggestive of well, differentiated liposarcoma (Figures 4 and 5). Immunohistochemistry for SMA, desmin, S100, CD34, B16, MDM, CDK4 and Ki67 were performed and were non-contributory. Patient was administered adjuvant radiotherapy
Figure 2: Intraoperative picture and specimen showing well encapsulated lipomatous tumor with surface bosselations.
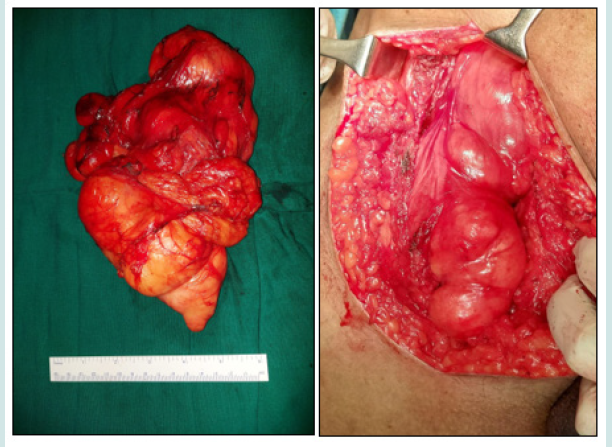
Figure 3: showing lobules of adipocytes separated by fibrous septae with variation in size of the cells with calcifications suggestive of liposarcoma.
Discussion
Retroperitoneal liposarcoma is the most frequently observed subtype of retroperitoneal tumor with an incidence of approximately 2.5 million individuals [4]. It usually occurs at 40 to 60 years of age and the ratio between the genders is approximately 1:1. The large volume of the intra-abdominal space allows liposarcoma to grow without compressing the vital organs resulting only rarely in early diagnosis. To differentiate from other soft tissue tumors auxiliary examinations are required, including ultrasonography, CT scan, and MRI. These investigations provide information on the tumor position and size in addition to appropriate staging of the tumor extent and involved structures, which aids greatly in designing a surgical scheme. Preoperative biopsy may indirectly improve outcomes in selected patients by virtue of receipt of neoadjuvant therapy and attainment of complete tumor resection [5]. The final diagnosis of the retroperitoneal sarcoma is dependent on the pathological and immunohistochemical analysis.
Liposarcoma can be histologically subdivided into five subtypes: Well-differentiated, myxoid, round-cell, pleomorphic and dedifferentiated [6]. Round-cell, pleomorphic, and de-differentiated subtypes are regarded as high grade whilst well differentiated and myxoid liposarcoma are low grade [7]. High histological grade is one of the most important negative prognostic factors. Welldifferentiated liposarcoma may recover locally but the metastatic potential is low while pleomorphic liposarcomas have high grade metastatic potential, which may reduce the survival rate [7]. With regards to the high recurrence rate of liposarcoma, complete resection is the predominant treatment. Successful complete resection of retroperitoneal liposarcoma may increase the five year survival rate from 16.7 to 58.9% [8]. However, complete resection is a challenge particularly in the well-differentiated subtype, for the reason that the margins are not easily distinguishable [9]. Even with complete removal of the liposarcoma prognosis remains poor.
The five-year survival rate of well-differentiated retroperitoneal liposarcoma is 83%, while it is 20% for the dedifferentiated tumor subtype [7]. Local recurrence remains the predominant cause of mortality in retroperitoneal liposarcoma [10]. In order to detect recurrence, patients who undergo complete resection should undergo active surveillance. Adjuvant radiation therapy may improve the outcomes by decreasing the local recurrence.
Conclusion
a. Retroperitoneal liposarcoma presenting as a femoral hernia is a rare presentation with only 2 cases reported in literature.
b. Pre-op diagnosis is crucial for complete work-up and surgical extirpation.
c. Since it has a high rate of recurrence, complete resection with tumor free margin is the benchmark for treatment.
d. Patient prognosis and recovery will depend upon age of presentation, tumor free margin excision, histology, radiotherapy, physiotherapy and rehabilitation.
e. Patient to be followed up actively as incidence of recurrence and metastasis is high.
f. It is mandatory to think of common possibilities first followed by thinking out of the box for Rare Case Possibilities if Clinically and Symptomatology do not correlate.
References
- Mendenhall WM, Zlotecki RA, Hochwald SN, Hemming AW, Grobmyer SR, et al. (2005) Retroperitoneal soft tissue sarcoma. Cancer 104(1): 669-675.
- Russell WO, Cohen J, Enzinger F, S I Hajdu, H Heise, et al. (1977) A clinical and pathological staging system for soft tissue sarcomas. Cancer 40(4): 1562-1570.
- Bradley JC, Caplan R (2002) Giant retroperitoneal sarcoma: A case report and review of the management of retroperitoneal sarcomas. Am Surg 68(1): 52-56.
- Neuhaus SJ, Barry P, Clark MA, Hayes AJ, Fisher C, et al. (2005) Surgical management of primary and recurrent retroperitoneal liposarcoma. Br J Surg 92(2): 246-252.
- Straker RJ 3rd, Song Y, Shannon AB, Marcinak CT, Miura JT, et al. (2021) Preoperative Biopsy in Patients with Retroperitoneal Sarcoma: Usage and Outcomes in a National Cohort. Ann Surg Oncol 28(11): 6868-6879.
- Singer S, Antonescu CR, Riedel E, Brennan MF (2003) Histological subtype and margin of resection predict pattern of recurrence and survival for retroperitoneal liposarcoma. Ann Surg 238(3): 358-371.
- Nijhuis PH, Sars PR, Plaat BE, Molenaar WM, Sluiter WJ, et al. (2000) Clinico-pathological data and prognostic factors in completely respected AJCC stage I-III liposarcomas. Ann Surg Oncol 7(7): 535-543.
- Lee SY, Goh BK, Teo MC, Min Hoe Chew, Pierce Kah Hoe Chow, et al. (2011) Retroperitoneal liposarcomas: the experience of a tertiary Asian center. World J Surg Oncol 9(1): 12-15.
- Chen ZH, Song XM (2009) The therapeutic progress in retroperitoneal liposarcoma. Chin J Gen Surg 24(1): 81-83.
- Milone M, Pezzullo LS, Salvatore G, Pezzullo MG, Leongito M, et al. (2011) Management of high-grade retroperitoneal liposarcomas: personal experience. Updates Surg 63(2): 119-124.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...