Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Realignment of a Malaligned Hallux Nail in an Adult. An Illustrated Case Report Volume 7 - Issue 2
Hau Pham*, Wei Tseng and Elizabeth Sanders
- Department of Surgery, Boston University, USA
Received:November 12, 2022; Published:November 23, 2022
Corresponding author: Hau Pham, Department of Surgery, Boston University, USA
DOI: 10.32474/SCSOAJ.2022.07.000256
Abstract
Malalignment of the hallux nail is an uncommon condition. There are three main types of nail malalignment: congenital, traumatic, and iatrogenic. They are often not reported so the incident is not well known. Most hallux nail malalignment is also associated with onychodystrophy and onychomycosis. Congenital malalignment is the most common form; it usually manifests at birth or early childhood. Toenail malalignment in adults is usually seen as a result of trauma. We present a case of malalignment of the hallux nail caused by trauma and surgery to repair the malalignment.
Introduction
Common toenail problems are onychomycosis, onychodystrophy, onychocryptosis, paronychia, subungual hematoma, onychomycosis, and subungual exostosis [1]. All these conditions lead to dystrophy of the toenail. The dystrophy can cause the toenail to become malaligned. Toenail malalignment is very rare and it is underreported. Toenail malalignment etiology includes congenital, traumatic, and iatrogenic. When malaligned, the longitudinal axis of the nail shifts in the transverse plane [2]. It is due to a deviation of the nail matrix. Pathogenesis has been related to the lateral rotation of the nail matrix. This fact results in deviation of the longitudinal axis of the nail plate that is not parallel to the corresponding axis of the distal phalanx of the hallux [2,3]. The lateral deviation is more common than the medial deviation [4]. Most of the reports in the literature involved the hallux nail [5- 8].
Traumatic nail malalignment and iatrogenic malalignment of the nail plate may be seen more often than reported in the literature. These malalignments may not be severe and a minor office procedure can usually resolve the problem. We report a severe malalignment of the hallux nail caused by trauma that affects the patient’s ability to ambulate without discomfort.
Case Report
History and Physical exam
A 19-year-old female presents to the office complaining of pain in her left 2nd toe for several months. She localizes the pain to the medial 2nd toe and describes the sensation as a pressure-type pain. The patient states the nail of her left big toe pushes against her 2nd toe. She has tried cutting the nail shorter but continues to have pain while wearing closed-toe shoes. She relates a history of ingrown in the left great toe which was treated successfully with partial nail avulsion 2 years ago. Several months ago, her left great toe was stepped on with the heel of a high-heel shoe. She denies any ecchymosis or bleeding. She had pain with mild swelling of the hallux but the nail did not fall off. The patient states she did not seek medical treatment immediately nor had any self-treatment. She recalls the ecchymosis, swelling, and pain all subsided within a few days. Shortly after the incident, she notices the nail of the injured toenail starting to grow towards her 2nd toe. The deviation has worsened with time, and so is the pain on the 2nd toe.
The patient’s past medical history includes Mood Disorder, Mixed-Expressive Language Disorder, Mild Mental Retardation, and Attention-Deficit/Hyperactivity Disorder. She is currently on medications for her social disorders. The patient is an occasional smoker and lives with her mother. She denies a family history of deviation from toenails in her family. On physical exam, she is 170 cm in height and weighs 57 kg. She is afebrile and her vital signs are stable. She is alert and oriented, and her affect and mood are noted to be appropriate. Her interaction is normal, and her judgment and insight are intact. Her HEENT, cardiac, respiratory, and abdominal exams are unremarkable. In terms of her lower extremity physical exam, her neurovascular status is intact. Her dermatological exam notes no open lesions. The patient’s left hallux nail is noted to be mildly thickened, but with no discoloration or subungual debris. Her left hallux is in anatomical position, but the nail laterally deviates. It is measured at 55 degrees from the vertical axis. The toenail is thickened, and the distal nail appears to have a fungal infection. The lateral border of the nail is incurvated into the nailbed and the lateral tip of the nail abuts the 2nd toe (Figure 1). She does not have any bunion or hammertoe deformities. Her left 1st MPJ range of motion is within normal limits. She has no other gross pedal deformity. A radiographic exam shows no fracture or dislocation of the hallux distal phalange. The distal phalange is in alignment with the proximal phalange (Figure 2). There is pain to palpation of the 2nd toe. There is no open wound nor sign of infection. The patient requested to have the hallux toenail straightened because the pain persisted despite frequent trimming of the toenail.
Figure 1: The hallux is in rectus position. The toenail has laterally deviated and the lateral tip of the hallux toenail impinged to the second toe before the nail is trimmed.

Surgical Procedure
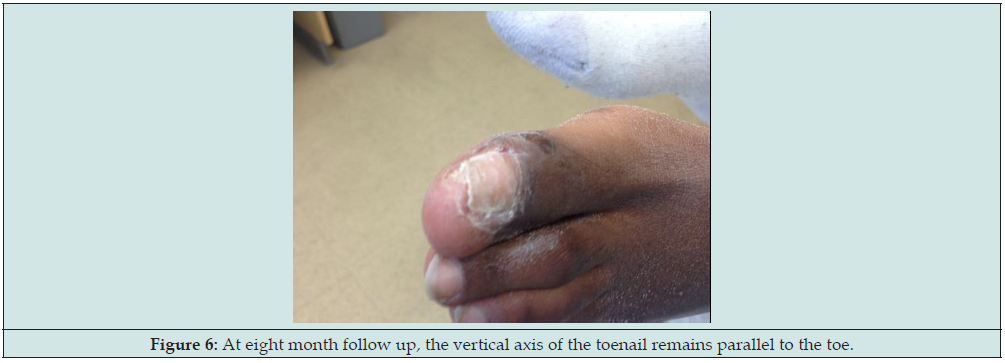
The impinged edge on the lateral aspect of the toenail is resected and removed. The surgical plan was mapped. The artist sketch in Figure 3 shows the lateral deviation of the hallux toenail with the toenail impinged into the 2nd toe. A U-shaped incision is made around the hallux, deep to the distal phalanx. Triangular shape skin incisions are made at the proximal lateral and medial end of the cut. These triangular-shaped skin are excised in full thickness and removed from the field. The skin and soft tissue are carefully dissected and lifted up from the dorsal surface of the distal phalanx (Figure 4). The double skin flaps were made to allow the nail to rotate back to a more anatomical position as described in Figure 3. After the flap was completely free from the dorsal surface of the distal phalanx, the wound is irrigated. The wound is closed with a nylon suture in a simple fashion (Figure 5). The patient has tolerated the procedure well. She has had an uneventful postoperative course. Sutures are removed after 3 weeks. At 8 months postoperative, the nail remains in a rectus position (Figure 6).
Figure 3: Artist sketch description of the procedure, courtesy of Nanette Habershaw. 2 triangular-shaped skins were excised. This allowed the nail to be derotated back to its normal position.
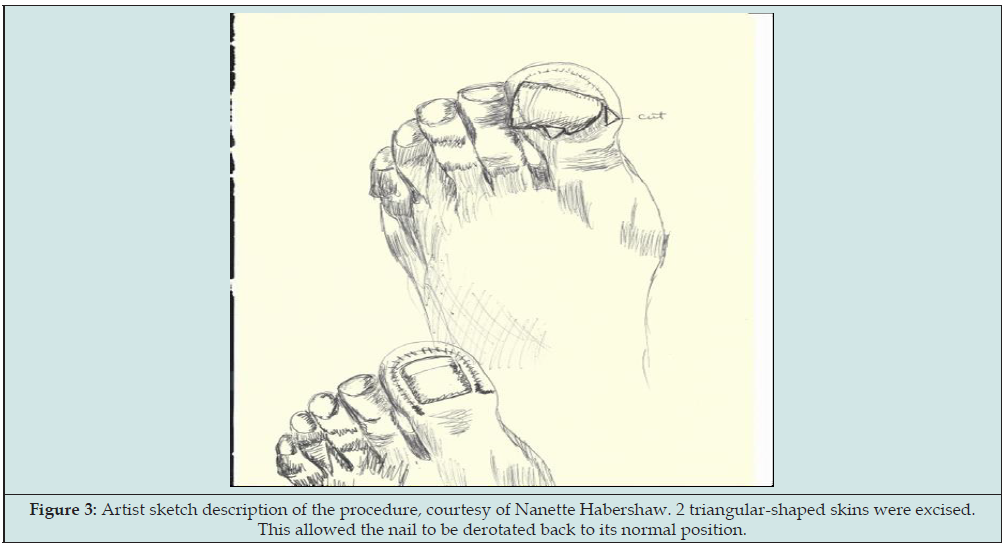
Figure 4: Nail lifted off the distal phalanx. U shape incision made around the nail. The nailbed is dissected and lift off the distal phalange.

Figure 5: Completion of Surgery. The triangular flaps allowed the whole toenail to be derotated back to rectus alignment.

Discussion
Toenail malalignment in adults may be more common than reported. The deformity is usually seen as minor and can be managed by trimming the toenail shorter. Many articles did not correctly report nail malalignment. A systemic review of 53 photographs found in 35 articles found only 30 pictures met the criteria, and 22 of 30 photographs had pure nail malalignment [8]. Some congenital nail malalignment may resolve spontaneously [9]. Cosmetic surgery improves the condition of many toenail deformities [10]. Flap for nail surgery had been described for lesions proximal and under the nail bed [11]. The procedure to correct the malalignment of the toenail consists of a realignment of the whole nail apparatus [12,13]. It was suggested that “it is impossible to perform a realignment of more than 45 degrees and that if the procedure is performed later in age, improvement is more functional than cosmetic allowing patients to wear almost any shoes”. The malalignment in our patient is 55 degrees when measuring the angle formed by the axis of the toe and the axis of the nail. We utilized a double skin flap technique to be able to rotate the nail plate and nailbed back to its anatomical position. This case presents a severe malalignment where the toenail is laterally rotated, abutting the adjacent second toe without any involvement of the underlying hallux distal phalange. We demonstrated a method to bring the toenail back to a more anatomical position. This surgical technique brought satisfactory results functionally and cosmetically to the patient. This re-alignment of a traumatic nail can be applied for severe congenital, traumatic and iatrogenic toenail malalignment. The skin flap is a useful technique to correct malalignment of the toenail.
References
- Bodman MA (2004) Nail dystrophies. Clin Podiatr Med Surg 21(4): 663-687.
- Perlis CS, Telang GH (2005) Congenital malalignment of the great toenails mimicking onychomycosis. J Pediatr 146(4): 575.
- Samman PD (1978) Great toe nail dystrophy. Clin Exp Dermatol 3: 81-82.
- Baran R, Bureau H, Sayag J (1979) Congenital malalignment of the big toenail. Clin Exp Dermatol 4(3): 359-360.
- Baran R, Bureau H (1983) Congenital malalignment of the big toe-nail as a cause of ingrowing toe-nail in infancy. Pathology and treatment (a study of thirty cases). Clin Exp Dermatol 8(6): 619-623.
- Decker A, Scher RK, Avarbock A (2015) Acquired Congenital Malalignment of the Great Toenails. Skin Appendage Disord 1(3): 147-149.
- Wagner G, Sasche MM (2012) Congenital Malalignment of the Big Toenail. J Dtsch Dermatol Ges 10(5): 326-330.
- Buttars B, Scott SG, Glinka D, Daniel CR, Brodell RT, Braswell MA (2022) Congenital Malalignment of the Great Toenail, the Disappearing Nail Bed, and Distal Phalanx Deviation: A Review. Skin Appendage Disord 8(1): 8-12.
- Handfield-Jones SE, Harman RR (1988) Spontaneous improvement of congenital malalignment of the great toenails. Br J Dermatol 118(2): 305-306.
- Richert B, Choffray A, De la Brassinne M (2008) Cosmetic surgery for congenital nail deformities. J of Cosm Dermatol 7: 304-308.
- Jellinek NJ (2012) Flaps in nail surgery. Dermatol Ther 25(6): 535-544.
- Baran R, Haneke E (1998) Etiology and treatment of nail malalignment. Dermatol Surg 24(7): 719-721.
- Baran R (1996) Significance and management of congenital malalignment of the big toenail. Cutis 58(2): 181-184.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...