Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Rare case of Bilateral Accessory Axillary Breasts – A Case Series Volume 7 - Issue 1
Thanzil Ahmed I1*, Leena S1, Surya Rao Rao Venkata Mahipathy2, Alagar Raja Durairaj3, Narayanamurthy Sundaramurthy4, Anand Prasath Jayachandiran4 and Suresh Rajendran5
- 1Post graduate Department of General Surgery, Saveetha Medical College & Hospital, India
- 2Professor & Head, Department of Plastic & Reconstructive Surgery, Saveetha Medical College & Hospital, India
- 3Professor, Department of Plastic & Reconstructive Surgery, Saveetha Medical College & Hospital, India
- 4Associate Professor, Department of Plastic & Reconstructive Surgery, Saveetha Medical College & Hospital, India
- 5Senior Resident, Department of Plastic & Reconstructive Surgery, Saveetha Medical College & Hospital, India
Received:August 24, 2022; Published:September 09, 2022
Corresponding author: Thanzil Ahmed I, Post graduate Department of General Surgery, Saveetha Medical College & Hospital, Tamilnadu, India
DOI: 10.32474/SCSOAJ.2022.07.000254
Abstract
Accessory breast tissue is a rare condition which occurs in 0.4-6% of women. These are commonly located in the axilla, chest wall, and vulva. The most common site of aberrant tissue is in the axilla, bilateral and presents as an asymptomatic mass, especially during pregnancy or lactation. The diagnosis of ectopic breast tissue is important as it can undergo the same pathological changes that occur in a normal breast, such as mastitis, fibrocystic disease and carcinoma. Here, we present a case of a bilateral axillary accessory breast in three women managed with surgical excision and confirmed as breast tissue by histopathology.
Keywords: Accessory; Axillary Breast; Pathological Changes; Surgical Excision
Introduction
The diagnosis of the accessory breast in the general population is variable and depends on gender, race, genetic disposition, and geographic location with prevalence rates of 0.4% to 6%, being more common in females (5.19%) than in males (1.68%) [1]. Supernumerary breast is the development of accessory nipple and/or areola complex with or without glandular breast tissues, whereas aberrant breast refers to ectopic breast tissue without a nipple or areola complex. Supernumerary mammary glands develop along the ectodermal ridges (the milk line) which extend from the axilla to the pubes and may occur as either unilateral or bilateral lesions in affected individuals. Supernumerary breasts are located in 90% of cases in the thorax, 5% in the abdomen and 5% in the axillary region [2]. These glands either mature into mammary glands or remain as accessory nipples in 2-6% of women [3]. The accessory breast tissue responds to the hormonal influences of the menstrual cycle, pregnancy, and lactation just as the anatomically normal breast. The rare sites of occurrence outside the milk line are the knee, lateral thigh, buttock, face, ear, and neck [4-6].
Case 1
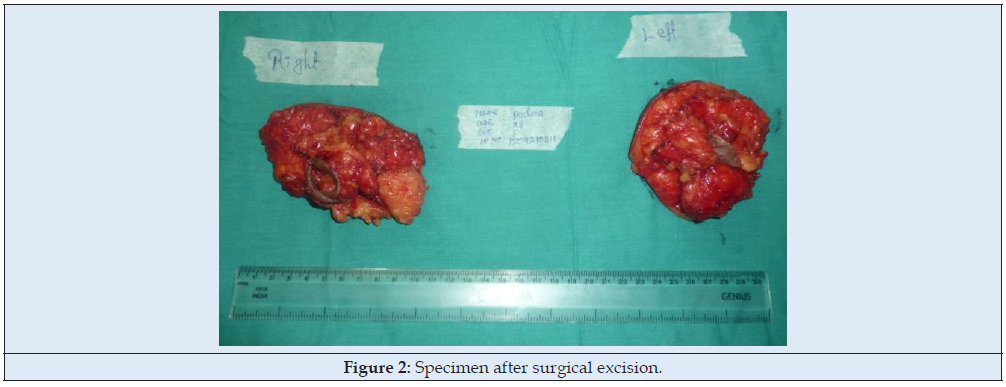
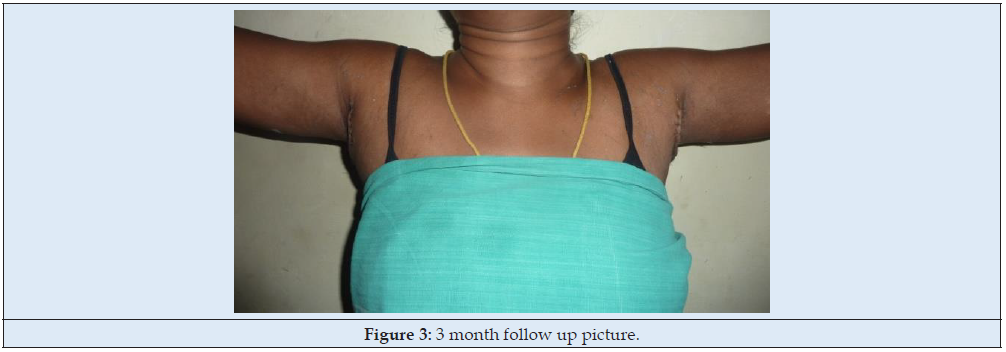
28-year-old female presented with a gradually increasing swelling in both axillae past 6 years. Initially, the swellings were painless but became tender during her pregnancy. On examination, there was a soft non-tender mass of size 5x4x3cm with no axillary lymphadenopathy (Figure 1). A diagnosis of accessory breast tissue was made and was planned for surgical excision. Under general anaesthesia, an elliptical axillary incision was made on the summit of the swelling and deepened in layers. Fibrofatty and glandular tissue were excised and sent for histopathology which was confirmed as breast tissue (Figure 2). Care was taken to preserve the neurovascular structures and not to thin the skin flaps too much. Haemostasis secured and the skin closed with 3-0 nylon over a 12 Fr closed suction drain. A Similar procedure was executed on the opposite side. Compression dressings were applied. The patient was comfortable at 3-month follow-up visit (Figure 3).
Case 2
18-year-old female presented with a gradually increasing swelling in both axillae past 4 years. The swellings were initially painless but became tender during puberty. On examination, there was a soft non-tender mass of size 6 x 5 x 5cm with no axillary lymphadenopathy (Figure 4). A probable diagnosis of axillary lipoma was made and was planned for surgical excision. Under general anaesthesia, an elliptical axillary incision was made on the summit of the swelling and deepened in layers. Fibrofatty was excised and sent for histopathology which was confirmed as breast tissue (Figure 5).
Case 3
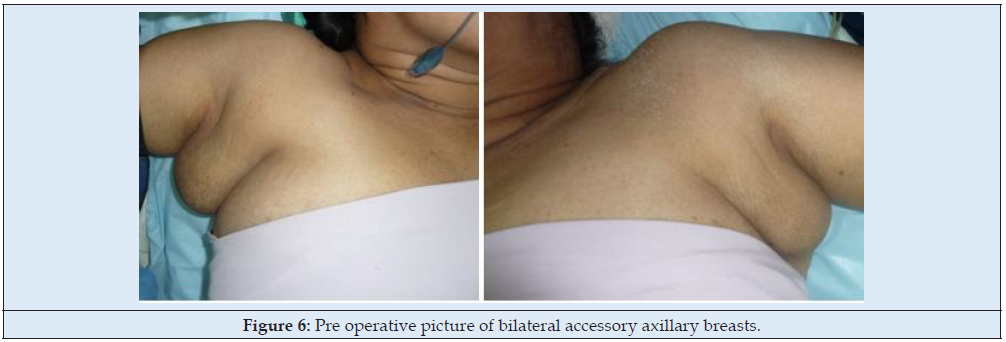
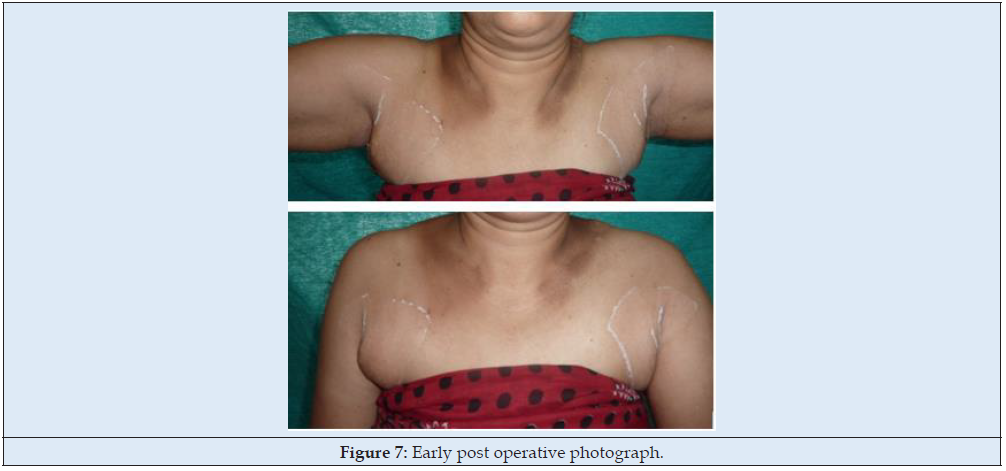
55-year-old female presented with a gradually increasing swelling in both axillae past 22 years. The swellings were initially painless but became tender during pregnancy and lactation. On examination, there was a soft non-tender mass of size 8 x 6 x 5cm with no axillary lymphadenopathy (Figure 6). A probable diagnosis of accessory axillary breasts was made and was planned for surgical excision. Under general anaesthesia, open surgical excision was done and the specimen sent for histopathological examination confirmed as breast tissue (Figure 7).
Discussion
Ectopic breast tissue occurs due to failure of resorption of the embryonic mammary ridge (milk line), which is an ectodermal thickening from axilla to groin bilaterally. It is the term used for both supernumerary and aberrant breast tissue, which are two different entities [7]. Supernumerary breasts have nipples, areolae or both with the varied compositions of glandular tissue [8]. They are mostly present along the mammary ridge but may also occur on the cheek, neck, shoulder, thigh or buttock [9]. It is usually sporadic; however, a hereditary and familial predisposition has also been reported [10]. Occurrence rates vary widely based on ethnicity and gender, ranging from as low as 0.6% in Caucasians to as high as 5% in Japanese females [10,11]. Supernumerary breast was categorized in 1915 by Kajava, whose classification system still remains in use today [12]. Class I consists of a complete breast including glandular tissue, nipple, and areola. Class II consists of only glandular tissue and nipple, without areola. Class III consists of only glandular tissue and areola, without a nipple. Class IV consists of only glandular tissue. Class V (pseudomamma) consists of only nipple and areola, without glandular tissue. Class VI (polythelia) consists of only the nipple. Class VII (polythelia areolaris) consists of only the areola. Class VIII (polythelia pilosa) consists of only hair. Medha Bhave has subclassified Kajava type IV axillary breast as para-mammary, central axillary and medial arm. This is important as the incision needs to be placed in the axilla and not on the mass directly which is aesthetically beneficial [13]. The accessory breast tissues are usually present at birth and stay dormant until puberty, pregnancy, or lactation. It then presents as a soft tissue swelling with or without a surrounding areola or nipple [12]. The management of accessory breast is mainly surgical. The various treatment modalities include open excision, liposuction, the combination of excision and liposuction (axillaplasty) and non-surgical methods like injection lipolysis and High Intensity Focused Ultrasound (HIFU) [14-16]. Excision is recommended in large size tissue for cosmetic reasons and to avoid any future complications [16]. An alternative tumescent liposuction technique was described, it allows to prevent the occurrence of the central depression appearance that is often left as a result of the adjacent fat tissue remnant following the traditional methods of resecting the accessory breast tissue [16]. This alternative approach may result in minimal scarring and better contour than can be obtained by conventional methods. The term axillaplasty was described by Kirwan in 2009 where he defines it as a procedure to correct the overhang of fat and skin above the bra at the armpit, which limits tops that women can wear. The fat is suctioned and excess skin is removed creating a neat thin line scar hidden in the apex of the axilla [17]. The complications are mild scar hypertrophy, medial arm pain, allergy to plaster, infection, seroma, haematoma, dog ear deformity, residual mass and axillary contracture [13].
Conclusion
Accessory axillary breasts are uncommon lesions which are often misdiagnosed as soft-tissue tumors. The most common disease seen in these accessory breasts was cancer and fibrocystic change. Diagnosis of accessory breast tissue is essential as it can undergo the same pathological changes that occur in the normal breast. A high index of suspicion is required to detect these lesions early to offer the best treatment options. Surgical management is recommended for cosmetic reasons as well as to avoid any future complications.
References
- Geddes DT (2007) Inside the lactating breast: The latest anatomy research. J Midwifery Womens Health 52: 556-563.
- Velanovich V (1995) Ectopic breast tissue, supernumerary breasts, and supernumerary nipples. South Med J 88(9): 903-906.
- Dabota YB (2012) Bilateral accessory breast: A case report. Jos J Med 6: 32-33.
- Nirmala JL, Gayathri M, Suguna S, Thirupurasundari R (2010) Accessory breast tissue in the axilla in a puerperal woman – Case study. Acta Medica Medianae 49: 45-48.
- Godoy-Gijón E, Yuste-Chaves M, Santos-Briz A, Esteban-Velasco C, de Unamuno-Pérez P (2012) Accessory breast on the vulva. Actas Dermosifiliogr 103: 229-232.
- Pfeifer JD, Barr RJ, Wick MR (1999) Ectopic breast tissue and breast-like sweat gland metaplasias: An overlapping spectrum of lesions. J Cutan Pathol 26: 190-196.
- Teke Z, Kabay B, Akbulut M, Erdem E (2008) Primary infiltrating ductal carcinoma arising in aberrant breast tissue of the axilla: a rare entity. Report of a case. Tumori 94(4): 577-583.
- Evans DM, Guyton DP (1995) Carcinoma of the axillary breast. J Surg Oncol 59(3): 190–195.
- Cheong GH, Lee BC, Lee KS (1999) Carcinoma of the axillary breast. Yonsei Med J 40(3): 290-293.
- Loukas M, Clarke P, Tubbs RS (2007) Accessory breasts: a historical and current perspective. Am Surg 73(5): 525–528.
- Patel PP, Ibrahim AM, Zhang J, Nguyen JT, Lin SJ, et al. (2012) Accessory breast tissue. Eplasty 12: ic5.
- Shreshtha S (2016) Supernumerary Breast on the Back: a Case Report. Indian J Surg 78(2): 155-157.
- Medha Bhave (2015) Axillary breast: Navigating uncharted terrain. Indian J Plast Surg 48(3): 283-287.
- Bartsich SA, Ofodile FA (2011) Accessory breast tissue in the axilla: classification and treatment. Plastic and Reconstructive Surgery 128(1): 35e-36e.
- Husain M, Khan S, Bhat A, Hajini F (2014) Accessory breast tissue mimicking pedunculated lipoma. BMJ Case Rep 2014: bcr2014204990.
- Fan J (2009) Removal of accessory breasts: a novel tumescent liposuction approach. Aesthetic Plast Surg 33(6): 809-813.
- Kirwan L. drkirwan.com.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...