Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Preoperative Parenteral Iron Supplementation in Critical Mesenteric Ischaemia Volume 2 - Issue 3
Misha Sidapra*, Sarah Jane Messeder, Chenhan Ma, Jill Austin, Euan Munro and Bryce Renwick
- Department of Vascular Surgery, Aberdeen Royal Infirmary, Aberdeen, United kingdom
Received: February 19, 2019; Published: February 26, 2019
Corresponding author: Misha Sidapra, Department of Vascular Surgery, Aberdeen Royal Infirmary, Aberdeen, United kingdom
DOI: 10.32474/SCSOAJ.2019.02.000137
Abstract
Background
Symptomatic mesenteric ischaemia is an uncommon disease entity which can prove complicated to diagnose and manage. Both endovascular and open operative approaches have been described but the nutritional complications caused by poor gut absorption can mean that these patients may be at higher risk of operative complications, and appropriate care should be given to preoperative nutritional optimisation prior to surgical management.
Objective
We present a case of critical mesenteric arterial stenosis treated with preoperative intravenous iron supplementation to illustrate preoperative optimisation and therapeutic approaches, together with a selected review of the literature
Conclusion
Preoperative parenteral iron supplementation is likely to be effective in reducing preoperative anaemia but the impact of this intervention on postoperative blood transfusion and other complications in the context of complex aortic surgery is unknown.
Keywords: Critical Mesenteric Ischaemia; Iron Supplementation; Preoperative Optimisation
Introduction
Chronic mesenteric ischaemia (CMI) caused by atherosclerotic stenosis of the arteries supplying the small bowel is a fairly common finding at autopsy (reported to be between 12-60% of elderly patients at autopsy [1]), however symptomatic critical mesenteric ischaemia is rarely reported and can elude diagnosis for extended periods of time due to the non-specific symptoms of presentation. Patients may complain of post-prandial abdominal pain, appetite and weight loss, and “food fear” [2]. In these patients, as the disease process can be protracted and well-established by time of diagnosis and management, patients may show signs of long-term undernourishment, including weight loss, electrolyte and micronutrient deficiencies and declining overall health [3]. As such, substantial preoperative optimisation may be required prior to consideration of operative management and revascularisation. Consideration should also be given postoperatively to a possibility of re-feeding syndrome. We present here the case of a 70-yearold woman seen in our unit with a complex critical mesenteric ischaemia compounded with general frailty and undernourishment.
Case Report
A 70-year-old woman was initially referred by her primary care doctor for assessment of unintentional weight loss for investigation of possible malignancy. At time of referral, the patient had lost 9 kilograms (from 51kg to 42kg) within 4 months (body mass index 18) and complained of persistent nausea and upper abdominal pain. She was noted to have a background of rheumatoid arthritis and chronic obstructive pulmonary disease. A CT scan of the thorax, abdomen and pelvis did not show any sign of malignant lesions, and upper gastrointestinal endoscopy revealed only mild gastritis. The patient was treated with helicobacter pylori eradication therapy and discharged (Figure 1). She was re-referred to the service following further concerning weight loss to a body weight of 35kg with a BMI of 12.86. A repeat upper GI endoscopy was completely normal. Blood tests showed a mild red cell macrocytosis (MCV 100) and low ferritin levels; renal function, electrolytes and liver function tests were unremarkable. Further review of CT imaging revealed an occluded coeliac trunk with stenosis at the origin of the superior mesenteric artery and suspicion of post-stenotic aneurysm.
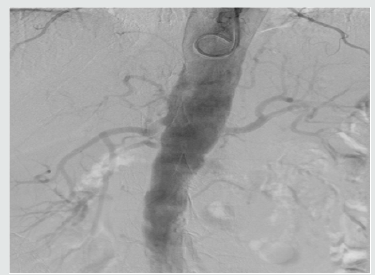
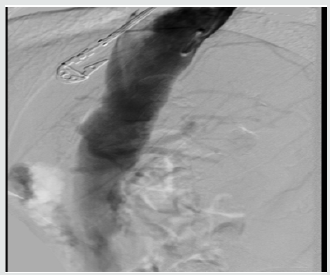
The patient underwent CT angiography which showed critical stenosis with short occlusion of the coeliac trunk origin, and a 3cm occlusion at the origin of the superior mesenteric artery. Bowel was entirely supplied by collateral vessels originating from the inferior mesenteric artery, which was itself also stenosed at its origin. Abdominal aorta, renal arteries and iliac vessels did not show any significant disease. Attempts were made to treat the stenoses with an endovascular approach but were ultimately unsuccessful as it was not possible to identify mesenteric vessel origins due to severity of stenosis. Following this the patient was planned to undergo supracoeliac aortic-SMA bypass, with preoperative optimisation with IV iron supplementation. The patient’s low ferritin levels at diagnosis were supplemented by this approach and came up to normal levels by the time of procedure; this was reflected in the improved full blood count of the patient.” The patient underwent laparotomy and adhesiolysis, following which the root of the SMA was identified (Figures 2 & 3).
Figure 5: Postoperative CT with 3D reconstruction showing right renal artery takeoff and vein graft.
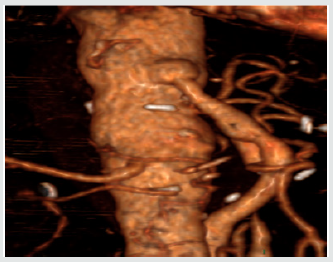
A long saphenous vein graft was harvested and anastamosed to the supracoeliac aorta proximally and the terminal SMA distally. On completion of anastamosis and upon opening of the graft, the small bowel became flushed pink and began enthusiastically peristalsing almost immediately (Figures 4 & 5). Postoperatively the patient progressed well, and upon follow up, had gained 7kg in the space of 3 months. Symptoms of post-prandial pain and nausea, as well as appetite generally, had improved significantly from her previous morbid state.
Discussion
ACritical mesenteric ischaemia poses a particular challenge for preoperative optimization; reduced arterial supply of the small bowel is likely to affect its function and the degree to which this occurs is likely to depend on the severity of the stenotic areas. Equally, preoperative anaemia is known to increase the risk of blood transfusion, and in turn, increase the morbidity and mortality risk of undergoing a procedure [4]. A recent study involving patients with colorectal cancer treated with preoperative intravenous iron supplementation showed that the haemoglobin level was significantly increased in the active treatment group, however the further impact of this increase on risk levels of morbidity and mortality is not known [5]. In particular, the effectiveness of this intervention is unknown in patients undergoing high risk aortic surgery. A 2015 Cochrane report identified 3 prospective randomised controlled trials investigating its use – two in colorectal surgery and one gynaecological study. This review suggested that there was a reduction in use of blood transfusions associated with preoperative intravenous iron supplementation but it was not statistically significant. Each of these studies had small patient numbers, however, and overall the authors note that the studies are unlikely to have had sufficient power to reliably analyse the significance of the effect [6].
Conclusion
We present a case of critical mesenteric ischaemia with use of preoperative intravenous iron supplementation. Intravenous iron replacement therapy has been noted in the literature to have reduced the prevalence of preoperative anaemia, though more studies are needed to see if this truly translates to lower levels of operative morbidity and mortality, and if this effect is seen across differing surgical procedures.
References
- Hansen KJ, Wilson DB, Craven TE, Pearce JD, English WP, Edwards MS, et al. (2004) Mesenteric artery disease in the elderly. J Vasc Surg 40(1): 45-52.
- Kolkman JJ, Geelkerken RH (2017) Diagnosis and treatment of chronic mesenteric ischemia: An update. Best Pract Res Clin Gastroenterol 31(1): 49-57.
- van Noord D, Kolkman JJ (2017) Functional testing in the diagnosis of chronic mesenteric ischemia. Best Pract Res Clin Gastroenterol 31(1): 59-68.
- Ellermann I, Bueckmann A, Eveslage M, Buddendick H, Latal T, et al. (2018) Treating Anemia in the Preanesthesia Assessment Clinic. Anesth Analg 127(5): 1202-1210.
- Wilson MJ, Dekker JW, Bruns E, Borstlap W, Jeekel J, et al. (2018) Shortterm effect of preoperative intravenous iron therapy in colorectal cancer patients with anemia: results of a cohort study. Transfusion 58(3): 795- 803.
- Ng O, Keeler BD, Mishra A, Simpson A, Neal K, et al. (2015) Iron therapy for pre-operative anaemia. Cochrane Database Syst Rev 22(12).

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...