Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Review Article(ISSN: 2643-6760) 
Posterior Vertebrectomy in Thoracolumbar Spine. Surgical Technique Review and Results Volume 4 - Issue 3
Vanessa Borrero Muñoz1* and Gustavo Uriza2
- 1Neurosurgeon, Clinica Universidad de la Sabana, Colombia
- 2Chief of Neurosurgery, Clinica Universidad de la Sabana, Colombia
Received: February 05, 2020; Published: February 14, 2020
Corresponding author: Vanessa Borrero Muñoz, Neurosurgeon, Clinica Universidad de la Sabana, Colombia
DOI: 10.32474/SCSOAJ.2020.04.000188
Introduction
Spine surgery has evolved through the years, and developed several techniques allows better results with shorter and less aggressive surgeries. Thoracolumbar spine has several surgical approach, according to the pathology that we need to treat, those may be anterior, such transthoracic, trans pleural - trans diaphragmatic or retroperitoneal, retroperitoneal or trans peritoneal; posterior approach, like transfacetary, transpedicular, lateral extra cavitary, costotransverse, among others, and in some cases, we need to do both, anterior and posterior, whit large and morbid surgeries. Surgeons around the globe, have developed a safe, less morbid technique, that allows perform, in just one surgery, anterior and posterior spine fixation, called posterior vertebrectomy.
Among the realignment techniques, we found Smith Petersen osteotomy, Ponte osteotomy, pedicle subtraction, partial or total corpectomies, and vertebral column resection. Schwab anatomical
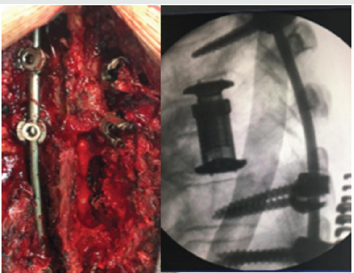
spine osteotomy classification15, has 6 grades resection [1]. partial facet join resection [2]. complete facet join resection [3]. pedicle and partial body resection [4]. pedicle, partial body and disc resection [5]. complete vertebra and disc resection [6]. multiple adjacent vertebrae and disc resection. In this paper, we are going to describe patient under 5 and 6 grade resections, by posterior approach only [7,8] (Figure 1).
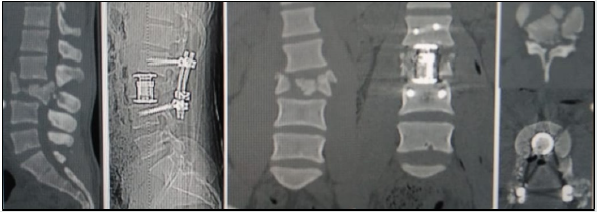
After the anesthetic techniques used by Morton, in 1848, laminectomy was the standard surgery for all spinal diseases. Ménard (costotransversectomy in 1894) and Capener (lateral racotomy, in 1933), were pioneers in Pott’s decease treatment with lateral and paraspinal approach, but they were not popular; and in 1976 lateral extracavitay approach was developed by Larson. The first-time vertebral resection was described to correct deformities, was in 1922 by MacLennan, in 1928 Royle resect a hemivertebrae, and it was until 1973 that Leatherman report again a vertebral resection. In 1987 Bradford popularized the technique, 10 years later, he and Tribus, describes combined anteroposterior technique in severe deformities. In 2002, Suk et all, publish for the first time only posterior approach, and in 2005 published 16 patient’s results; later, Lenke, in 2009, publish a 35 patient’s series, with severe spine deformity, corrected by only posterior approach [9-13] (Figure 2).
Some years ago, surgeons believe that was not possible totally remove thoracic vertebral just with transthoracic approach, and in the 70’s Roy-Camille and Stener, developed a unique posterior approach for treatment of spinal tumor, and it´s been evolved through the years [14].
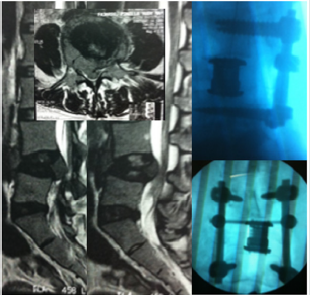
This technique it’s a valid option for all Deni’s column injury, patients who cannot tolerate anterior thoracic procedures, or long segments fixation; allows decompress neural structures and it’s safe visualization during all the procedure, rebuild anterior spine, correct deformities, pathological tissue dissection (tumor or infections), and remove several levels. This posterior spine stabilization via a 360- degree construct, also restore sagittal balance performing intraoperative kyphotic correction, restores spinal height and allows both ventral and dorsal decompression, with minimal surgical morbidity [9,15,16]. Posterior vertebrectomy is indicated in vertebral tumors, vertebral body fractures, spinal deformities, and infections, patients with no neurological injury [17-23], or complete neurological injury, with posterior ligament injury; and is not required collaboration of other surgical specialties [24] (Figure 3).
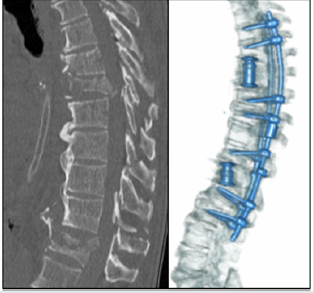
A consensus panel review by the spine trauma study group, in 2006, concluded that lesion’s morphology, neurological condition and posterior ligament’s integrity are the most important points to approach decision; though surgeon’s experience is a determinant factor [24]. Posterior approach is familiar to the spinal surgeon, and avoid vascular and visceral structures. Only posterior approach vertebrectomy has similar complication to anterior approach, like cerebrospinal fluid fistulae, material failure, wound complications, and incidental durotomy. Costotrasversectomy and lateral approach has more complications, like pneumonia, pleural lesion, hemothorax, pulmonary insufficiency, and larger hospital stay [2,9,22-25]. Biomechanically, a distractible cage that allows is correct the kyphosis by lengthening the anterior column, achieving the reconstruction of the anterior spine; and it is supplemented by dorsal pedicle screw and rod implants, getting a circumferential construct [16] (Figure 4).
Figure 4: Male, 42y, T7-T6 AO A3 and T12 AO A3. ASIA C. Brown – Sequard syndrome. Work accident (drop fall).
According to Knop et al. [17,19], expandable cages resist axial
compression, lateral flexion, and axial rotation. Also, combined
with posterior instrumentation, resist translation of the vertebrae
above and below the cage in both the sagittal and the coronal plan.
In Clinica Universidad de la Sabana, we have used this technique,
(distractible cage supplemented by dorsal pedicle screw) with
Intraoperative neurophysiological monitoring, having excellent
results. In our series, we have from 2016 to September 2019,
12 patients, 8 males, 4 females; 7 thoracic, 6 lumbar; etiology:
7 traumatic, 5 tumoral, 1 infection; one patient has 2 thoracic
fractures, that required 2 different surgeries; age: 5 patients 20 to 29 (1F, 4M), 1 female from 40 to 49, 2 from 60 to 69 (1M, 1F), and 4
from 70 to 79 (3M, 1F) [26].
According to Schwab’s classification, we perform 10 type 5
osteotomies, and 3 type 5 [27,28]. Those who had neurological
deficit, recovered after surgery with physical therapy, none of
them was ASIA A. One patient had an epidural hematoma after
the surgery, and has paraparesis, that recover after drainage, and
one patient, has a trans operatory hypovolemic shock, and died. 3
patients had work accident, and 2 a car accident. We can conclude
that 66.6% were male, 41.6% between 20 and 29, most of them
traumatic, and the older group, 33.3%, most of them tumoral,
according to the literature, this technique allows a safe surgery, in
just one intervention, and reduces the complication risks, having an
excellent outcome, using neurophysiological monitoring.
References
- Aydogan (2008) Kyphosis, scoliosis and kyphoscoliosis. Journal of Pediatric Orthopaedics B 17(1): 33-37.
- Clavel Escribano M, Clavel Laria P, (1996) El abordaje posterolateral extracavitario a la columna dorsal. Neurocirugía 7: 119–125.
- Crocker M (2008) Posterior approach vertebrectomy in the thoracolumbar spine with expandable cage reconstruction: indications and techniques based on eight cases, British Journal of Neurosurgery 22(2): 235-240.
- Jong-Il C (2017) Single-Stage Transpedicular Vertebrectomy and Expandable Cage Placement for Treatment of Unstable Mid and Lower Lumbar Burst Fractures. Clinical Spine Surgery 30(3): E257-E264.
- Hamzaoglu A (2011) Posterior Vertebral Column Resection in Severe Spinal Deformities: A Total of 102 Cases. Spine, 36(5): E340–E344.
- Mazel C (2014) Long-term quality of life after en-bloc vertebrectomy: 25 patients followed up for 9 years. Orthopedics & Traumatology: Surgery & Research 100: 119-126.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...