
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Research Article(ISSN: 2643-6760) 
Post-Operative Outcomes in Obese Vs. Non-Obese Children with Adolescent Idiopatic Scoliosis Undergoing Posterior Spinal Deformity Surgery: An ACS-NSQIP Analysis Volume 4 - Issue 2
Hassan MM*, Naqvi A, McKenzie SA, Thompson TL and Wilson RH
- Department of Orthopaedic Surgery, Howard University Hospital, USA
Received: January 13, 2020; Published: January 22, 2020
Corresponding author: Mahad M Hassan, Department of Orthopaedic Surgery, Howard University Hospital, Washington DC, USA
DOI: 10.32474/SCSOAJ.2020.04.000183
Abstract
Background: While obesity is on the rise in the pediatric population, there is a paucity of literature concerning the effect obesity may have on post-operative outcomes. Posterior spinal fusion for the treatment of Adolescent Idiopathic Scoliosis is one of the most common spinal procedures in the pediatric population. However, the role obesity may play on outcomes following this extensive surgery is poorly understood.
Methods: The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database for children was queried to identify pediatric patients who underwent spinal deformity correction surgery. Patients who had undergone an anterior surgical approach were excluded from the analysis. Children were categorized as Obese if their BMI exceeded 95th percentile for their age group in months. They were then stratified into cohorts based on their obesity status (Obese vs. Non-Obese) and compared in regard to demographics, pre-operative comorbidities, intra-operative, and post-operative outcomes. Propensity score matching was then performed to limit confounders between the two cohorts. Statistical analysis was performed utilizing independent t-tests for continuous variables and chi-square analysis for categorical data. Statistical significance was set at <0.05.
Results: A total of 1702 patients met the inclusion criteria for the study, 851 obese and 851 non-obese. Pre-operatively, the mean age of both the non-obese and obese patients was 14 years (p=0.481). The mean weight was 48.62 kg for non-obese patients, and 83.06 for obese patients (p<0.001), while BMI was 20.46 in the non-obese group and 36.99 in the obese group (p<0.001). Both cohorts had a majority of female patients (non-obese: 75.3% vs. obese: 74.6%, p=0.780). The most common ASA score in both groups was 2 (non-obese: 71.0% vs. obese: 70.2%, p=0.899). White patients underwent fusion more often in the non-obese and obese groups (71.7% vs. 70.9%, p=0.820). Intra-operative findings demonstrated obese patients spent a significantly longer time in the operating room (272.75 minutes vs. 293.10 minutes, p<0.001). Non-obese patients had a significantly longer LOS than obese patients (5.75 days vs. 4.59 days, p<0.001). There was a significantly higher incidence of superficial SSI in obese patients (0.2% vs. 1.2%, p=0.038). Non-obese patients had significantly more bleeding needing transfusions than obese patients (67.0% vs. 61.6%, p=0.023), and had more total blood transfused (335.94 mL vs. 222.02 mL, p<0.001). Obese patients had a higher 30-day readmission rate (2.6% vs. 5.2%, p=0.008). No other differences were observed in demographics, medical conditions, or postoperative complications.
Conclusion: Obesity significantly increases the risk for early complications in pediatric patients undergoing spinal deformity surgery. Obese patients are at increased risk for longer operative time, postoperative superficial infection and 30-day readmission. As such, spine surgeons should be cognizant of these potential adverse outcomes and should consider the benefits of prophylactic protocols.
Abbreviations: AIS: Adolescent idiopathic scoliosis; BMI: Body Mass Index; SSI: Surgical Site Infection; ASA: American Society of Anesthesiology; SSI: Surgical Site Infection; LOS: Length of Stay; UTI: Urinary Tract Infection; DVT: Deep Vein Thrombosis;
Introduction
Adolescent idiopathic scoliosis (AIS) is the most common variant of scoliosis, with an incidence of 2% - 5% and a strong preponderance for women [1-3]. In this population, the increasingly common treatment for AIS is multilevel posterior spinal fusion. There have been numerous improvements to the procedure allowing for better long-term outcomes [4,5]. Some studies suggest a peri-operative complication rate of about 0.2% - 5% depending on the patient population and severity of AIS, among other things [1,6,7]. Numerous studies have demonstrated the increased risk associated with obese patients undergoing spinal surgery. Basques et al showed that obese patients developed more adverse events following PSF [1]. Patel et al identified a correlation between increasing BMI and perioperative complications in patients undergoing spinal fusion [8]. The role obesity may play on outcomes, and the underlying pathophysiology, following this extensive surgery is poorly understood. Furthermore, the vast majority of the literature focuses on the adult population. While obesity is on the rise in the pediatric population, there is a paucity of literature on the effect obesity may have on post-operative outcomes. This study aims to compare the peri-operative outcomes between obese and non-obese patients with AIS undergoing posterior spinal deformity surgery using relevant variables including, surgical site infection (SSI), unplanned reoperation and 30-day readmission.
Methods
Data source
The American College of Surgeons National Surgical Quality Improvement Program Pediatric (ACS NSQIP Peds) database was utilized for this study. The ACS NSQIP Peds provides information on patients under the age of 18 that undergo major surgical procedures at participating hospitals (https://www.facs.org/quality- programs/childrens-surgery/pediatric/overview). Approximately 94 data points are collected on patients and compiled from most pediatric surgical specialties at acute care children’s hospitals, specialty children’s hospitals, children’s hospitals within a larger hospital, and pediatric wings of acute care hospitals. Outcomes for 30-days post-procedure are also included.
Patient selection
The ACS NSQIP Peds was retrospectively reviewed for all patients between January 1, 2012 and December 31, 2016. Patients were included if they had a diagnosis of idiopathic scoliosis (ICD codes: 737.32, 737.30, M41.114, M41.115, M41.116, M41.119) and a spinal fusion (CPT codes: 22800, 22802, 22804). Patients were excluded if they had a diagnosis of neuromuscular scoliosis or were under the age of 5 years. A total of 7,517 patients were identified.
Data Collection
Demographic factors such as age, weight by kilogram, body mass index (BMI), gender, American Society of Anesthesiology (ASA) physical status score, and race were collected for each patient. Patient BMI was calculated utilizing weight and height data made available in the NSQIP database. Obesity was calculated based upon patient weight in kilograms and age at the time of surgery, with patients having a weight in the 95th percentile for their age classified as obese. Operative time, total length of stay (LOS) and surgical complications in the 30-day period after spinal fusion were compared between non-obese and obese patients. The complications assessed included superficial surgical site infection (SSI), deep SSI, organ space SSI, wound dehiscence, sepsis, urinary tract infection (UTI), postoperative pneumonia, bleeding needing transfusion, total blood transfused, deep vein thrombosis (DVT), pulmonary embolism, acute renal failure, nerve injury, unplanned reoperation and 30-day readmission.
Statistical Analysis
Propensity score matching was performed to limit confounders between non-obese and obese patients. Patients were matched on age, gender, ASA score and race. Continuous variables were compared using t-tests, while categorical variables were compared using chi-square or Fisher’s exact tests. Statistical significance was set at 0.05. All statistical analyses were performed using SPSS version 25 (IBM Corporation, Armonk, New York, USA).
Results
There were a total of 1,702 patients included for analysis after
propensity score matching, 851 non-obese patients and 851 obese
patients (Table 1). The mean age of both the non-obese and obese
patients was 14 years (p=0.481). The mean weight was 48.62 kg
for non-obese patients, and 83.06 for obese patients (p<0.001),
while BMI was 20.46 in the non-obese group and 36.99 in the obese
group (p<0.001). Both cohorts had a majority of female patients
(non-obese: 75.3% vs. obese: 74.6%, p=0.780). The most common
ASA score in both groups was 2 (non-obese: 71.0% vs. obese:
70.2%, p=0.899). White patients underwent fusion more often in
the non-obese and obese groups (71.7% vs. 70.9%, p=0.820).
Compared to non-obese patients, obese patients spent a
significantly longer time in the operating room (272.75 minutes vs.
293.10 minutes, p<0.001) (Table 2). Conversely, non-obese patients
had a significantly longer LOS than obese patients (5.75 days vs.
4.59 days, p<0.001). There was a significantly higher incidence
of superficial SSI in obese patients (0.2% vs. 1.2%, p=0.038). No
significant difference was seen between non-obese and obese
patients in deep SSI (0.6% vs. 1.2%, p=0.300), organ space SSI (0.2%
vs. 0.1%, p=0.999), wound dehiscence, (0.9% vs. 0.9%, p=0.999),
sepsis (0.6% vs. 0.4%, p=0.726), UTI (0.8% vs. 0.5%, p=0.547),
postoperative pneumonia (0.6% vs. 0.2%, p=0.452), DVT (0.0%
vs. 0.0%), PE (0.0% vs. 0.0%), acute renal failure (0.1% vs. 0.0%,
p=0.999), nerve injury (0.5% vs. 0.4%, p=0.999) or unplanned
reoperations (2.5% vs. 3.8%, p=0.162). Non-obese patients had
significantly more bleeding needing transfusions than obese
patients (67.0% vs. 61.6%, p=0.023), and had more total blood
transfused (335.94 mL vs. 222.02 mL, p<0.001). Obese patients
had a higher 30-day readmission rate (2.6% vs. 5.2%, p=0.008).
Table 1: Demographics for non-obese and obese scoliosis patients.
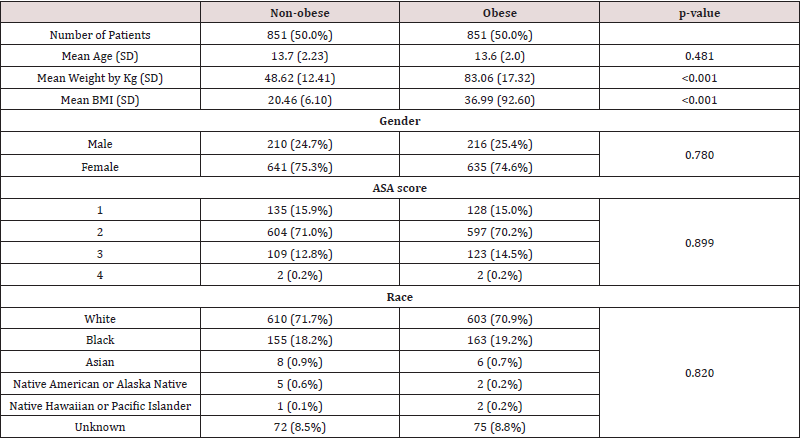
SD: Standard Deviation
Kg: Kilograms
BMI: Body Mass Index (kg/m2)
ASA: American Society of Anesthesiology physical status score
Table 2: Surgical complication rates between non-obese and obese scoliosis patients.
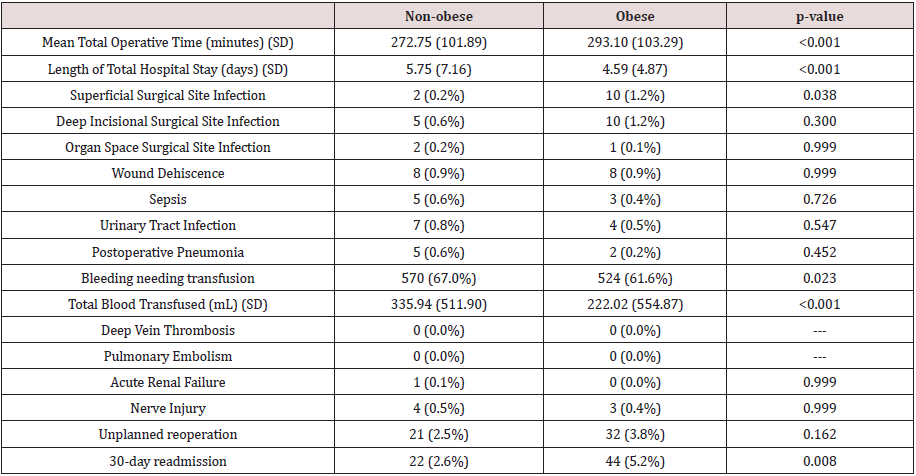
BMI: Body Mass Index (kg/m2)
Discussion
The obesity epidemic has tremendous fiscal implications for
the US healthcare system. Obesity accounts for over 300,000 deaths
and over $100 billion in healthcare costs annually [9]. Additionally,
the incidence of obesity is also increasing in Europe demonstrating
the global nature of this issue [10,11]. The pathophysiological
changes associated with obesity have been well documented in the
literature. Obese patients demonstrate significant impairment in
both cardiac and pulmonary function [10,12,13]. Furthermore, obesity
predisposes patients to numerous comorbidities including hypertension,
diabetes, and coronary artery disease.13 As such, these
patients have demonstrated an increased risk for the development
of postoperative complications such as infection [14]. However, the
vast majority of the literature has analyzed the risk of complications
in the adult population following general surgery. The prevalence
of obesity in children 2-19 years of age is 16.9% [15]. The
goal of our study was to assess the additional risk, if any, pediatric
patients with AIS may incur while undergoing spine surgery.
The obese cohort demonstrated a significantly longer total
operative time (272.75 minutes vs. 293.10 minutes, p<0.001)
compared to non-obese patients. As such, these patients are placed
at greater risk of postoperative complications. Peersmen performed
a retrospective analysis of 6489 who underwent total knee
arthroplasty in order to assess the role of operative time on rates of
infection.16 Their study demonstrated an increased risk of infection
in association with increased operative time.16 Additionally, they
identified weight, body mass index, comorbidity burden as risk
factors for increased operative time [16]. Furthermore, our costconscious
healthcare environment seeks to reduce healthcare
spending. However, longer operative times most certainly result in
the utilization of more hospital resources. As such, surgeons may
benefit from counseling patients on weight loss prior to surgery if
possible.
Obese patients also demonstrated a significantly higher risk of
superficial ((0.2% vs. 1.2%, p=0.038) surgical site infection (SSI).
Numerous studies have demonstrated an increased risk of infection
in obese patients undergoing spine surgery. Wound infection rates
of 4% for clean surgical sites have been reported for non-obese
patients while the literature reports rates as high as 40% for clean
contaminated sites in obese patients [17-21]. Olsen et al performed
a retrospective case control study on 219 patients in order to
assess the risk of SSI following spine surgery [21]. They identified
postoperative incontinence, posterior approach, tumor resection,
and morbid obesity as independent risk factors for SSI [21,22].
Obese patients in this study had a higher 30-day readmission rate
(2.6% vs. 5.2%, p=0.008). While there was no statistical difference
in early reoperation, the higher incidence of readmission in the
obese cohort may be explained by the higher incidence of superficial
surgical site infection requiring IV antibiotics.
Non-obese patients in this study had a significantly longer
length of stay (LOS) (5.75 days vs. 4.59 days, p<0.001). They
also had significantly more bleeding needing transfusions than
obese patients (67.0% vs. 61.6%, p=0.023), and had more total
blood transfused (335.94 mL vs. 222.02 mL, p<0.001). This is
counter to what previous studies have found [23]. Further longterm
prospective studies will be needed to see if these results are
repeatable. There are limitations to this analysis. This analysis was
performed using a national database consisting of self-reported
data. Hospitals with higher incidences of complications may be
more reserved about sharing their outcomes. Therefore, this data
may be skewed towards better outcomes. Also, these procedures
were conducted at multiple hospitals by different surgeons who
may all utilize different perioperative protocols. Therefore, these
findings may not be generalizable to all patients in all regions of
the US. As such, prospective standardized studies are warranted to
clearly identify the additional risk, if any, obese patients may incur.
Conclusion
Obesity significantly increases the risk for adverse outcomes in pediatric patients undergoing spinal deformity surgery. Obese patients are at increased risk for longer operative time, postoperative superficial infection and 30-day readmission. These potential complications contribute significantly to morbidity and may even be life threatening. As such, spine surgeons should be cognizant of these potential adverse outcomes and should consider the benefits of increased patient counseling. In addition, prospective standardized studies should be conducted to elucidate the risk obesity may play in the development of adverse outcomes following spinal deformity surgery in the pediatric population.
References
- Basques BA, Bohl DD, Golinvaux NS (2015) Patient factors are associated with poor short-term outcomes after posterior fusion for adolescent idiopathic scoliosis. Clinical orthopaedics and related research 473: 286-294.
- El-Hawary R, Chukwunyerenwa C (2014) Update on evaluation and treatment of scoliosis. Pediatric clinics of North America 61: 1223-1241.
- Konieczny MR, Senyurt H, Krauspe R (2013) Epidemiology of adolescent idiopathic scoliosis. Journal of children's orthopaedics 7: 3-9.
- de Kleuver M, Lewis SJ, Germscheid NM (2014) Optimal surgical care for adolescent idiopathic scoliosis: an international consensus. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 23: 2603-2618.
- Roach JW, Mehlman CT, Sanders JO (2011) "Does the outcome of adolescent idiopathic scoliosis surgery justify the rising cost of the procedures?". J Pediatr Orthop 31: S77-80.
- Coe JD, Arlet V, Donaldson W (2006) Complications in spinal fusion for adolescent idiopathic scoliosis in the new millennium. A report of the Scoliosis Research Society Morbidity and Mortality Committee. Spine 31: 345-349.
- Lykissas MG, Jain VV, Nathan ST (2013) Mid- to long-term outcomes in adolescent idiopathic scoliosis after instrumented posterior spinal fusion: a meta-analysis. Spine 38: E113-E119.
- Patel N, Bagan B, Vadera S (2007) Obesity and spine surgery: relation to perioperative complications. Journal of Neurosurgery: Spine 6: 291-297.
- Mokdad AH, Bowman BA, Ford ES (2001) The continuing epidemics of obesity and diabetes in the United States. JAMA : the journal of the American Medical Association 286: 1195-2000.
- Dindo D, Muller MK, Weber M (2003) Obesity in general elective surgery. The Lancet 361: 2032-2035.
- Organization WH (2000) Obesity: preventing and managing the global epidemiced: World Health Organization.
- Berkalp B, Cesur V, Corapcioglu D (1995) Obesity and left ventricular diastolic dysfunction. International journal of cardiology 52: 23-26.
- Pi-Sunyer FX (1993) Medical hazards of obesity. Annals of internal medicine 119: 655-660.
- Shapiro M, Muñoz A, Tager IB (1982) Risk factors for infection at the operative site after abdominal or vaginal hysterectomy. New England Journal of Medicine 307: 1661-1666.
- Ogden CL, Carroll MD, Kit BK (2014) Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA : the Journal of the American Medical Association 311: 806-814.
- Peersman G, Laskin R, Davis J (2006) Prolonged operative time correlates with increased infection rate after total knee arthroplasty. HSS Journal 2: 70-72.
- Buckwalter JA, Herbst CA (1983) Perioperative complications of gastric restrictive operations. Am J Surg 146: 613-618.
- Maini BS, Blackburn GL, McDermott WV (1977) Technical considerations in a gastric bypass operation for morbid obesity. Surg Gynecol Obstet 145: 907-908.
- Telfeian AE, Reiter GT, Durham SR (2002) Spine surgery in morbidly obese patients. Journal of neurosurgery 97: 20-24.
- Gepstein R, Shabat S, Arinzon ZH (2004) Does obesity affect the results of lumbar decompressive spinal surgery in the elderly? Clinical orthopaedics and related research pp. 138-144.
- Olsen MA, Mayfield J, Lauryssen C (2003) Risk factors for surgical site infection in spinal surgery. Journal of neurosurgery 98: 149-155.
- Malone DL, Genuit T, Tracy JK (2002) Surgical site infections: reanalysis of risk factors. Journal of Surgical Research 103: 89-95.
- Epstein NE (2017) More risks and complications for elective spine surgery in morbidly obese patients. Surg Neurol Int 8: 66.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




