Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case report(ISSN: 2643-6760) 
Pigmented Villonodular Synovitis in Children – A Case Series Volume 1 - Issue 5
K Warrier, S Deepak and S Rangaraj*
- Paediatric Rheumatology, UK
Received: December 18, 2018; Published: January 02, 2019
Corresponding author: S Rangaraj, Paediatric Rheumatology, UK
DOI: 10.32474/SCSOAJ.2019.01.000123
Abbreviations: PHPV: Persistent Hyperplastic Primary Vitreous; PVNS: Pigmented Villonodular Synovitis; JIA: Juvenile Idiopathic Arthritis
Case Report
Patient 1
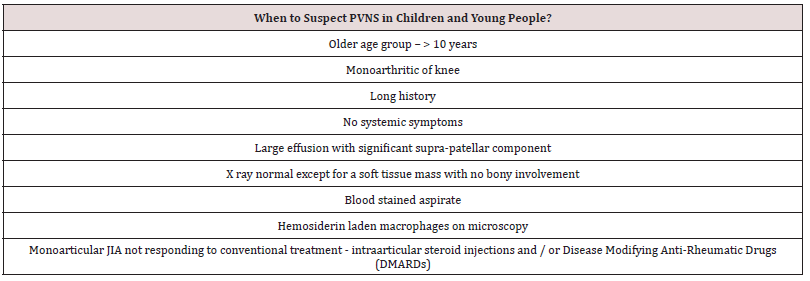
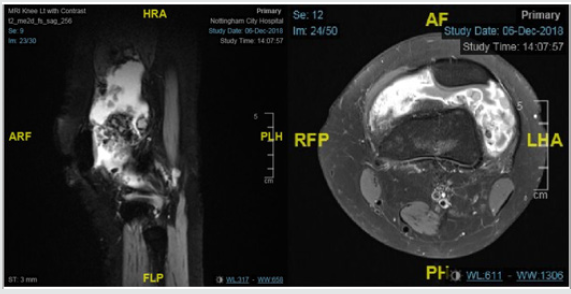
A 11-year-old girl was referred by the Orthopaedic team with swelling of her right knee which started five months back. She had no systemic symptoms or preceding trauma or infection. She was seen by the Orthopaedic team, who aspirated the joint and injected it with steroids, once the cultures came back as negative. She had a good response, although the swelling returned after 8-10 weeks, associated with some stiffness. She was previously fit and well except for visual impairment in her left eye due to Persistent Hyperplastic Primary Vitreous (PHPV). Her examination revealed moderate effusion in her right knee. Her blood tests including inflammatory markers were normal. With a diagnosis of oligoarticular JIA, she had a further intra-articular steroid injection with good response lasting 4 months. Subsequently she required two more steroid injections in the same joint within six months, at which stage she was commenced on weekly Methotrexate injections at 15mg/m2. Despite that, the swelling recurred, which did not respond to intra-articular steroid injection, following which MRI scan was requested. This showed diffuse synovial proliferation with relatively low signal components in some areas, suggestive of diffuse PVNS (Figure 1). Her immunosuppression was stopped, and she was referred for synovectomy.
Figure 1: Diffuse synovial proliferation with relatively low signal components in some areas, suggestive of diffuse PVNS.
Patient 2
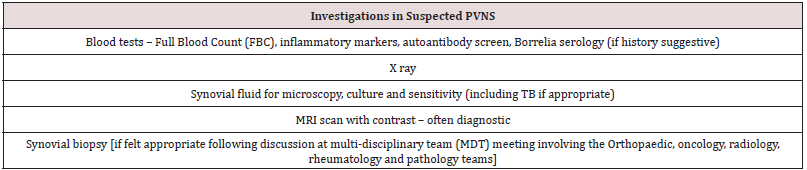
A 14-year-old boy was referred by the Oncology team with 7-month history of swelling in R knee. The onset was preceded by varicella infection. The aspiration of the knee joint carried out by the local Orthopaedic team revealed blood stained fluid, which was negative on bacterial cultures. But the swelling and the pain recurred and progressed despite regular Ibuprofen. He had no systemic symptoms including fever. His blood tests, including inflammatory markers, were normal. MRI scan of his right knee showed multi-loculated fluid collection with septas and post contrast enhancement of the collection walls with no involvement of underlying bone. He underwent synovial biopsy which ruled out sarcoma but showed synovial thickening and fibrinoid degeneration. He was then referred to pediatric rheumatology team as possible Juvenile Idiopathic Arthritis (JIA). On examination he had a large swelling of the right knee joint, more prominent in his supra patellar region with warmth and minimal restriction of movement. The rest of the joints were normal. In view of the relatively long history, the age, involvement of a single knee joint and blood-stained synovial fluid aspirate, a diagnosis of Pigmented Villonodular Synovitis (PVNS) was considered. His repeat MRI scan showed prominent and, in some places, nodular synovial proliferation around the knee and a large effusion, consistent with PVNS (Figure 2). He had poor response to intra-articular steroid injection which he had while waiting for surgery. He remains asymptomatic following open synovectomy.
Figure 2: Prominent and in someplaces nodular synovial proliferation around the knee and a large effusion, consistent with PVNS.
Patient 3
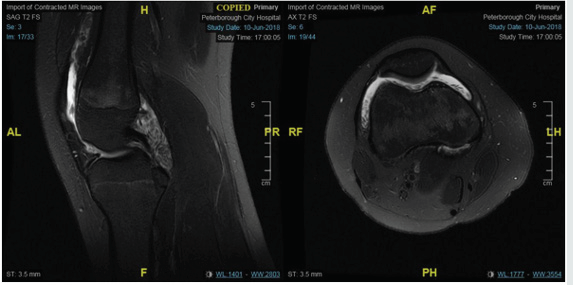
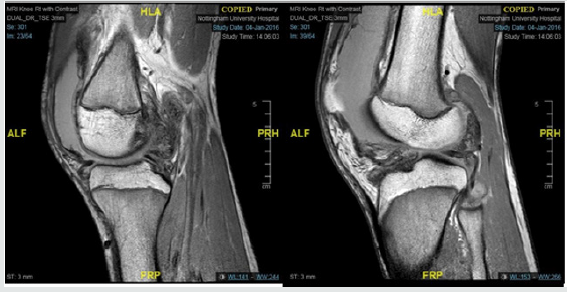
A 17-year-old girl was referred by her GP for swelling in her left knee for 3 years. The onset was insidious with no preceding trauma. The swelling slowly increased in size, associated with stiffness and significant and painful limitation of knee flexion. Following a failed aspiration in primary care, she had an ultrasound scan which revealed a large joint effusion. There were no concerns about any other joints or systemic symptoms. There was no significant past or family history. Her examination revealed large effusion of the left knee with restriction, with a significant suprapatellar component. Rest of the musculoskeletal examination and the systemic examination were normal. Her blood tests showed mild increase in inflammatory markers (CRP of 13 mg/L and ESR of 29 mm/hr) with negative autoantibody screen. MRI scan of her left knee revealed large joint effusion with multiple synovial protrusions which are low signal on T2-weighted images and intermediate signal on T1- weighted images, with peripheral enhancement suggestive of PVNS (Figure 3). She has been referred for consideration of synovectomy (Tables 1,2).
Figure 3: MRI scan of her left knee revealed large joint effusion with multiple synovial protrusions which are low signal on T2- weighted images and intermediate signal on T1-weighted images, with peripheral enhancement suggestive of PVNS.
Discussion
Pigmented Villonodular Synovitis (PVNS) is a rare condition characterized by diffuse synovial cell proliferation that affects the synovial joint, tendon sheaths, and bursa membranes [1,2]. Although a disease of young adults, it can occurs in older children, where it is usually monoarticular [3] with knee being the commonest joint involved. Pain and swelling are the usual presentation although mechanical symptoms like meniscal injury and patellar dislocation can rarely occur in adult PVNS [4]. The diagnosis is often delayed (mean of 18 months2) or mistaken for Juvenile Idiopathic Arthritis (JIA), infections like tuberculosis, hematological problems like hemophilia (due to hemarthrosis) or neoplastic processes affecting the synovium. All the above cases were referred to the Pediatric Rheumatology team as JIA by a variety of clinicians - primary care, Orthopaedic and oncology teams. The delay is often the longest in the patients who were commenced on treatment for JIA, which is demonstrated by the 2-year delay in diagnosis in patient 1.
The X ray findings are usually nonspecific - soft tissue swelling [4]. Erosive changes of bone secondary to the synovial proliferation, which can be seen in about 50% of adults with PVNS, are rare in children [5]. The synovial aspirate is often blood stained and the presence of blood-stained fluid with fragments of synovial villi in sediment and macrophages containing hemosiderin have been suggested as diagnostic criteria [6]. However, MRI findings of PVNS are characteristic (soft tissue mass with a hypo-intense signal in T1- and T2 weighted images representing hemosiderin deposits), although it is supplemented by biopsy and histopathological diagnosis in most case series. The treatment of choice is surgery, which could be open or arthroscopic synovectomy, although recurrence has been reported.
Arthroscopic and open synovectomy did not differ significantly in terms of rates of recurrence and complications [7]. Adjuvant treatment with external beam radiation therapy or intra-articular injection of radioactive material as yttrium-90 (Radio Synovectomy) [8], which has been used as an adjunct treatment modality in adults with PVNS, is hardly used in children due to risk of damage to epiphyseal growth plate and post-radiation sarcomas [2].
Conclusion
Pigmented Villonodular Synovitis is benign proliferative disorder, which can be associated with significant morbidity if left untreated. Because it is rare in children, the diagnosis is often delayed, resulting in delay in treatment. It should be suspected in chronic monoarthritic in older children without any systemic symptoms or patients with monoarticular JIA who are not responding to standard treatment. MRI scan, often in combination with synovial biopsy, confirms the diagnosis. Synovectomy seems to be the consensus treatment of choice.
References
- Ottaviani S, Aryal X, Dougados M, Gossec L (2011) Pigmented villonodular synovitis: A retrospective single center study of 122 cases and review of literature. Semin Arthritis Rheum 40(6): 539-546.
- Baroni E, Russo BD, Masquijo JJ, Bassini O, Miscione H (2010) Pigmented villonodular synovitis of the knee in skeletally immature patients. J Child Orthop 4(2): 123-127.
- Botez P, Sirbu PD, Grierosu C, Mihailescu D, Savin L, et al. ((2013) Adult multifocal pigmented villonodular synovitis-clinical review. International Orthopaedics (SICOT) 37(4): 729-733.
- Edwards MR, Tibrewal S (2004) Patello-femoral joint pain due to unusual location of localized pigmented villonodular synovitis: A case report. Knee 11(4): 327-329.
- Philip Neubauer, A Kristy Weber, Nancy Hadley Miller, Edward F, Mc Carthy (2007) Pigmented Villonodular Synovitis in Children: A Report of Six Cases and Review of the Literature. Iowa Orthop J 27: 90-94.
- I Zimmermann Górska, M Puszczewicz, G Bialkowska Puszczewicz (2001) Diagnostic value of synovial fluid analysis in pigmented villonodular synovitis (PVS) - a proposal of diagnostic criteria. Arthritis Res 3(Suppl A): pp.117.
- E Carlos Rodriguez Merchan (2014) Open versus arthroscopic synovectomy for pigmented villonodular synovitis of the knee. Journal of Orthopaedic Surgery 22(3): 406-408.
- Wael AM Nassar, MRCS & Ayman Abdelaziz Bassiony, Hesham A, Elghazaly (2009) Treatment of Diffuse Pigmented Villonodular Synovitis of the Knee with Combined Surgical and Radio synovectomy. HSSJ 5(1): 19-23.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...