
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Osteogenesis Imperfecta: about One Case and Literature Review Volume 5 - Issue 2
Andrianarison Lofo Heriniaina*, Ranaivomanana Volahasina Francine, Andriambelo Zinambatosoa Andrianina and Randrianjafisamindrakotroka Nantenaina Soa
- UPFR Anatomy and Cytology Pathology Unit, University Hospital – Joseph Ravoahangy Andrianavalona – Antananarivo
Received:June 05, 2020; Published: June 12, 2020
Corresponding author: Andrianarison Lofo Heriniaina, UPFR Anatomy and Cytology Pathology Unit, University Hospital – Joseph Ravoahangy Andrianavalona – Antananarivo, CHU Antananarivo 101 Madagascar
DOI: 10.32474/SCSOAJ.2020.05.000206
Abstract
Osteogenesis imperfecta is a rare congenital pathology with an incidence approximately 1/15,000 to 1/20,000 births. It is an autosomal dominant genetic disease cause by an abnormality type I of collagen with a mutation in the COL1A1 or COL1A2. It is characterized by a frailty and bone deformity with growth retardation. It can be viable or lethal, according to the type. Prenatal diagnosis is based in imaging examinations and can be confirmed by cytogenic examination. In our country, financial problem is often a blockage for prenatal imaging examinations and the technical platform is insufficient for a cytogenic examination. The aim of our study is to describe an osteogenesis imperfecta case, in order to improve its prenatal diagnosis and to demonstrate the interest of the fetal autopsy in a country where the means of diagnosis are limited. This is to properly guide genetic counseling and for a better care of a subsequent pregnancy.
Introduction
Osteogenesis imperfecta is a rare congenital pathology characterized by a frailty and bone deformity with growth retardation [1]. Its incidence is approximately 1/15,000 to 1/20,000 births [2,3]. It is more often as not transmitted in an autosomal dominant way and due to an abnormality type I of collagen with a mutation COL1A1 or COL1A2 genes [4]. According to the classification of Sillence and Glorieux, it can be viable or lethal [5]. The objective of our study is to describe an osteogenesis imperfecta case in order to improve its prenatal diagnosis and to demonstrate the interest of the fetal autopsy in a country where the means of diagnosis are limited.
Case Presentation
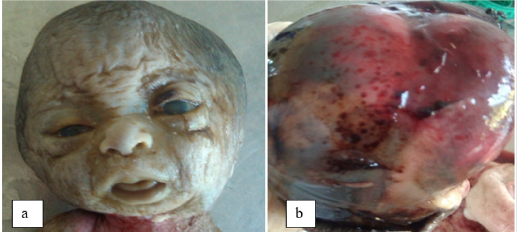
We report a case of 28 weeks amenorrhea (SA) fetus referred to the UPFR for pathological Anatomy and cytology department for brevity of the limbs. It is a spontaneous pregnancy and the parents had no particular personal or familial medical history. At the autopsy, the measurement of the biometric parameters revealed a growth retardation compatible with 22SA fetus; vertex-heel distance of 22 cm (5 °p), vertex-coccyx of 19 cm (5 °p), head circumference of 25 cm (25-50 °p) and 4 cm (5 °p) foot. On examination of the head (Figure 1), we observed a cranio-facial dysmorphism like a clover head, proeminent forehead, hypertelorism, low inserted ears, anteverted nose, long philtrum with retrognathism. At the opening of scalp [figure 1b], the dome of the skull was without bony structure and reduced in conjunctive membrane with petechia. The encephalon examination was impossible owing to the lyses. The examination of the trunk was without particularity. The dissection of the thoracic, abdominal and pelvic viscera showed no abnormality in shape or volume. On examination of the limbs (Figure 2), the fore-arms were curved and the legs were saber with hypoplasia of the big toe and internal gust. The bone radiography showed bone hypodensity of severe bone deformities and multiple fractures of the long bones. In total, this is a hypotrophic fetus with cranio-facial dysmorphia, demineralized dome of the skull, severe bone deformities and multiple fractures. The diagnoses of osteogenesis imperfecta type II was suggested face to these morphological signs.
Figure 1: a: facial cranial dysmorphism (clover head, prominent forehead, hypertelorism, flat nose root); b: demineralized dome of the skull.
Discussion
The osteogenesis imperfecta is a rare disease, often due to a
mutation in the COL1A1 or COL1A2 on chromosome 17q21, 33. Its
transmission can be autosomal recessive or dominant depending
on the type [1]. Its incidence is from 1/15,000 to 1/20,000 births
[2,3]. In our study, no particular medical history of malformation
was observed from the parents which demonstrated the De Novo
nature of the mutation, in favor of an autosomal dominant disease.
To our knowledge, it is the first case described in Madagascar.
According to the classification of Sillence and Glorieux, there are
18 types of osteogenesis imperfecta, depending to the affected
gene and clinical severity. Types I to IV are the most frequent and
the others are very rare and exceptional. Types I, III and IV are
compatible with life whereas type II is lethal. The latter is clinically
characterized by short long bones, severely deformed with in utero
fractures. The entire skeleton is weakly mineralized.
Antenatal diagnosis is based on imaging tests. Morphological
ultra sound of the fetus allows to observe some signs which can
guide the diagnoses, especially in case type II, characterized by a
weak echogenicity of the bones, a deformation of long bones and
multiple fractures [1,7]. In our case, the ultra sound showed brevity
of the limbs. A multi cut uterine content CT scan with an average
dosimetry of 3m GY is indicated in front of any suspected congenital
bone disease [7]. It allows a reconstitution in 3 dimensions and
this facilitates the precise analysis of the pelvis, spine, ribs, facial
bones and bones of the inner ears [7]. Magnetic reasoning imaging
is indicated for the detection of cerebral, thoracic, digestive and
urinary anomalies. It is complementary of diagnosis from the
second trimester. It gives a good image quality, it is independent
of the fetal position and has no harmful effect. In our study, neither
computed tomography nor magnetic reasoning imaging was
performed to refine the diagnosis.
In post-natal or post-medical termination of the pregnancy,
the ultra sound of fetus before autopsy is an essential examination
face to a congenital bone disease. It shows a hypodensity of all the
bones, curvature of long bones, multiple fractures, vomer bones of
the skull, a thorax in a chaim, and an agenesis of the bones of the
inner ear [1,3,4]. In our case, the X-ray showed bone hypodensity,
bone deformities and multiple fractures, but it could not be done
before the autopsy, which did not allow observing the skull and the
rib cage.
The fetal autopsy reveals a stunted growth, a demineralized
skull and the blue sclera [1,2,6]. Other sings such as imperfect
dentinogenesis and scoliosis can be seem in non-lethal imperfecta
osteogenesis. In our case we observed stunted growth cranio
facial dysmorphia with demineralization of the skull, sever
bone deformation and multiple fractures. These malformations,
associated with radiological signs, allowed us to evoke the diagnosis
of imperfecta osteogenesis type II which is lethal.
For the taking care, in case of type I, III, IV, the objectives of the
treatment are to reduce the fractures, optimize the motor functions
and to promote the patients independence the means used are
surgery functional or medical treatment with bisphosphonate
[1,3,5]. For type II, a medical termination of pregnancy is often the
first recommendation [3,5]. In our case, the result of the autopsy
helped to guide genetic counseling by recommending medically
assisted procreation for any subsequent pregnancy in order to
detect the disease earlier. From the prognostic point of view, the
lethal form ends in perinatal death due to respiratory distress
syndrome [1,3]. The non-lethal forms are compatible with life and
the patient can be independent if the treatment is adequate and
well followed [8].
Conclusion
Osteogenesis imperfecta is a rare disease. It can be lethal or compatible with life according to the type. An early prenatal diagnosis is necessary for the therapeutic decision and a multidisciplinary consultation is essential before any decision is taken. The fetal autopsy allows completing the information obtained during the prenatal examination, and also guiding the diagnosis.
References
- Marini JC, Cabral WA (2018) Osteogenesis Imperfecta; Genetics of Bone Biology and Skeletal Disease.
- Sillence DO, Senn A, Danks DM (1979) Genetic heterogeneity in osteogenesis imperfecta. J Med Genet 16(2): 101-116.
- Stoll C, Dott B, Roth MP, Alembik Y (1989) Birth prevalence rates of skeletal dysplasias. Clin Genet 35(2): 88-92.
- Forlino A, Marini JC (2016) Osteogenesis imperfecta. Lancet 387(10028): 1657-1671.
- Van Dijk FS, Sillence DO (2014) Osteogenesis imperfecta: Clinical diagnosis, nomenclature and severity assessment. Am J Med Genet Part A, 164A: 1470-1481.
- Van Dijk, G Pals, Van Rijn (2009) Classification osteogenesis imperfect revisited; European Journal of Medical Genetics.
- Gorincour G, Chaumoitre K (2014) CT scan of the fetal skeleton. When? How? 'Or' Why? Diagnostic and interventional radiology journal.
- Brasseur-Daudruy M, Ickowicz V, Eurin D. Fetal (2007) MRI: indications, limits and dangers. Gynecol Obstet Fertil 35: 678-83.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





