Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Review Article(ISSN: 2643-6760) 
Orbital Mass in A 9Year Old Girl Volume 1 - Issue 5
S Deepak, K Warrier and S Rangaraj*
- Department of Paediatric and Adolescent Rheumatology, UK
Received: December 18, 2018; Published: January 02, 2019
Corresponding author: S Rangaraj, Department of Paediatric and Adolescent Rheumatology, UK
DOI: 10.32474/SCSOAJ.2019.01.000121
Introduction
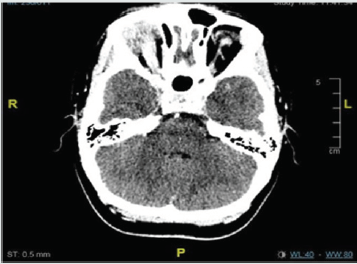
A 9-year-old girl presented with 4-month history of swelling and discoloration on the right upper eyelid and inability to open the eyes completely (Figure 1). She was previously fit and well with no past medical history of note. She was initially diagnosed with periorbital cellulitis at the local hospital and was treated with antibiotics and antihistamines for four weeks with no improvement. Initial investigations showed elevated platelet count of 508, and raised inflammatory markers - ESR of 67 mm/hr and CRP of 40 mg/L. The CT scan was suggestive of a mass lesion on the upper eyelid (Figure 2). Biopsy done by the ophthalmology team showed soft tissue fibro-inflammatory mass with reactive lymphoid aggregates and dense histiocytic and eosinophilic inflammation centred around variable calibre vessels. No atypical leukemic/ lymphoid infiltrates were seen. Histiocytic cells were positive for CD160 and negative for Langerin. Hence a diagnosis of small vessel vasculitis was suggested. The child was then referred to our tertiary pediatric rheumatology service.
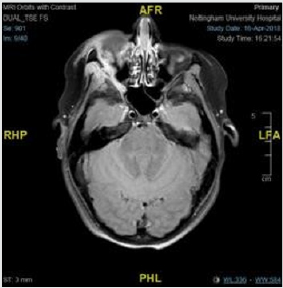
On examination the child was apyrexial with normal vital signs. She had tender, erythematous swelling of the right upper eyelid and fullness around the right cheek (Figure 3). She had normal vision with blocked right nostril, reduced sensation of smell, and taste. The systemic examination was completely normal. The antibody testing showed negative ANA, and weakly positive p-ANCA, but MPO and PR3 were negative. An MRI of the orbit with contrast showed significant enlargement of the intra -orbital mass with enhancement in the infratemporal and pterygopalatine fossa and masticator compartment, and induration and enhancement of the fat of the right cheek (Figure 4). The possibility of IGG4 disease was discussed at the multi-disciplinary team (MDT) meeting involving pathology, oncology, and ophthalmology teams. the biopsy specimens were reviewed. This confirmed evidence of vasculitis with the presence of fibrinoid necrosis with mostly lymphocytes infiltrating the blood vessel wall. There were >10 IgG4 positive cells per high power field, but the total cells did not represent 40% of plasma cells. Her serum IgG levels were normal as well as the IgG subtypes. With a provisional diagnosis of localised IgG4 related disease, she received weaning course of steroids and weekly subcutaneous methotrexate (15mg/m2) with very good response.
Discussion
Immunoglobulin G4-related disease (IgG4-RD) is a systemic fibro-inflammatory disease affecting different parts of the body [1,2]. The disease is characterized by tumour-like infiltrations of IgG4 positive plasma cells in the tissues, mostly with fibrotic abnormalities and often but not always elevated serum IgG4 levels. IgG4-RD can affect any organ or tissue and hence the clinical picture is highly heterogeneous and these patients can present to a number of different specialties. IgG4-RD is a disease of middle to upper age, with an onset at 50–70 years [3,4] and more common in men. It is rare in children with median age 13 years in a systematic review5. IgG4-related orbital disease (IgG4-ROD) was the commonest site (44% of case reports) in the paediatric age group; the other sites included pancreatitis, cholangitis, pulmonary disease, thyroiditis, lymphadenopathy and sialadenitis [5].
The inflammatory markers (ESR and CRP) are often elevated with autoantibodies negative. IgG4 level was elevated in 16/23 paediatric patients. Most of the patients undergo computed tomography (CT) or magnetic resonance imaging (MRI) scans as a part of investigations. 18F-fluorodeoxyglucose. Positron emission tomography (FDG PET)/CT, which can highlight active inflammatory lesions, is a useful tool for diagnosis, staging and monitoring4. Histopathology is considered the gold standard in the diagnosis of IgG4-RD, characterised by dense lymphoplasmacytic infiltrate, fibrosis, and obliterative phlebitis [6]. The diagnosis often requires collaboration between the clinicians involved, radiologist and pathologist, as this case demonstrated.
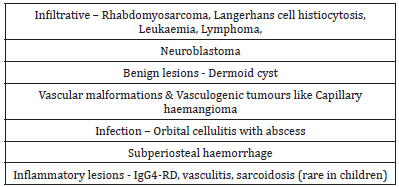
When untreated, IgG4-RD can cause irreversible organ damage hence early and aggressive treatment is indicated. Glucocorticoids (GCs) are the first-line therapy in IgG4-RD4 with prompt response, although it often relapses following tapering or stopping steroids. Azathioprine, mycophenolate Mofetil and Methotrexate have been used as GC sparing agents in the treatment of IgG4-RD. Recently B-cell depletion with RTX has been used successfully, leading to specific IgG4 reductions and very effective disease control, even in GC refractory patients [7,8]. These results have been replicated in certain paediatric case reports too (Table 1).
Conclusion
IgG4-RD is a rare but significant disease in children that can lead to considerable morbidity. This case highlights the need to consider this as a differential diagnosis, thereby facilitating early treatment.
References
- Kamisawa T, Zen Y, Pillai S, Stone JH (2015) IgG4-related disease. Lancet 385(9976): 1460-1471.
- Pieringer (2014) IgG4- related disease: an orphan disease with many faces. Orphanet Journal of Rare Diseases 9: 110.
- Brito-Zeron P, Ramos Casals M, Bosch X, Stone JH (2014) The clinical spectrum of IgG4-related disease. Autoimmun Rev 13(12): 1203-1210.
- David Lang, Jochen Zwerina, Herwig Pieringer (2016) IgG4-related disease: current challenges and future prospects. Therapeutics and Clinical Risk Management 12: 189-199.
- Faiz Karim, Jan Loeffen, Wichor Bramer, Lauren Westenberg, Rob Verdijk, et al. (2016). IgG4-related disease: a systematic review of this unrecognized disease in paediatrics. Pediatric Rheumatology 14:18.
- V Deshpande (2012) Consensus statement on the pathology of IgG4- related disease. Modern Pathology 25(9): 1181-1192.
- Khosroshahi A, Carruthers MN, Deshpande V, Unizony S, Bloch DB, et al. (2012). Rituximab for the treatment of IgG4-related disease: lessons from 10 consecutive patients. Medicine (Baltimore). 91(1): 57-66.
- Carruthers MN, Topazian MD, Khosroshahi A (2015) Rituximab for IgG4- related disease: a prospective, open-label trial. Ann Rheum Dis 74(6): 1171-1177.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...