Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Research Article(ISSN: 2643-6760) 
Obstructed Defecation Syndrome does the Starr Procedure Take Place? Technical and Functional Facts Volume 4 - Issue 1
Gerardo Martín Rodríguez1* and Pablo Piccinini2
- 1Staff Surgeon and Endoscopist, Clínica Del Angelo, Argentina
- 2Consultant Surgeon, CEMIC, Ciudad Autónoma de Buenos Aires, Argentina
Received: December 02, 2019; Published: December 16, 2019
Corresponding author: Gerardo Martín Rodríguez, Staff Surgeon and Endoscopist, Clínica Del Angelo Formosa, Argentina
DOI: 10.32474/SCSOAJ.2019.04.000180
Summary
Background: constipation due to bowel obstruction in the outflow tract aims to correct the anatomy and functionality of the pelvic floor in the posterior side. Among several approaches, the STARR technique (Stapled Trans Anal Rectocele Resection) has valid foundations in order to solve them.
Objectives: to communicate the experience with the technique in a center of Argentina and analize its feasibility, results and review the current evidence.
Design: prospective and consecutive
Materials and Methods: between January 2009 and January 2019 Starr was used in 30 patients diagnosed with constipation due to bowel obstruction in the outflow tract –Obstructed defecation syndrome - (ODS) caused by rectocele with or without rectoanal intussusception. We analyse the demographic variables, indications, technique, morbidity rate and functional results.
Results: 100% of the people who had surgery were women. The average age in all the procedures was about 58,5 years old. The tecnique was performed as ambulatory surgery in the 6% percent of the cases. The global index of complications was of 30% percent, which was grouped according to the Dindo-Clavien classification. Severe complications or morbidity weren’t registered. 30% percent of the patients presented recurrence of the symptoms after more than six months follow up, eventhough all of them solved through fingering or manoeuvre in order to empty the bowels and improved the quality of life.
Conclusion: Starr tecnique is and effective and safe procedure for the treatment of constipation due to ODS. It could be carried out as outpatient basis. The correct indication and experience in the handling of mechanical sutures are essential. The recurrence of symptoms is probably associated with functional and neuromuscular disorders devoloped by the patients.
Keywords: Constipation; oubstructed defecation syndrome; surgery; starr
Background
Among the types of constipation, patients with Obstructed Defecation Syndrome (ODS) represent a subgroup with serius deterioration of quality of life, to whom we can offer surgical correction of the anatomical alterations which determine their symptoms. The challenge is complex, since it is important to achieve the improvement of the functionality in the bowel mechanism which is affected under these circumstances. For the ODS determined by a previous rectocele, associated (or not) to a rectoanal intussusception, there are various approaches which are described, with variable acceptance and uncertain long- term results. Among the resection techniques, the procedure called Stapled Transanal Rectal Resection (STARR) was proposed in the early 2000’s by the doctor Antonio Longo with interesting arguments on its favor [1]. The purpose of this communication is to present our experience with the approach, analyze its feasibility and results in our place, revising the national and international evidence.
Material and Methods
we carried out a consecutive longitudinal analysis of data
uploaded on a prospective database of the procedures done with STARR. We recorded the demographic variables, indications and
short – and long terms morbidity.
The data was uploaded prospectively on a computerized
database (Excel). The results are expressed in averages and
percentages. For this approach we selected patients with
constipation for obstruction of the outflow tract caused by previous
rectocele with or without rectoanal intussusception evidenced
with physical exam, colonic transit, video defecography (VDFG) or
dynamic resonance of the pelvic floor ( RMNDPP) with significant
effect on the life quality and did not improve with hygiene and
dietetic measures and / or Biofeedback. One diameter of rectocele
greater than or equal to 4 cm in VDFG or 2,5 cm in RMNDPP and
that it didn’t empty completely during the bidding process was
considered pathological. In order to evaluate the symptoms and
the alteration of the life quality, the patients completed a modified
questionnaire of the ODSSS index of the Italian Society of Colon
and Rectal Surgery, which was answered by the patients before the
surgery and after one month of postoperative period [2]. All the
procedures were carried out by the same colorectal surgeon with
experience in hemorrhoidopexy with mechanical suture. During
the preoperative period, a cleansing of the rectum with phosphates
and antibiotic prophylaxis enemas in the anesthetic induction
(ciprofloxacin 200 mg + metronidazole 500 mg) was done.
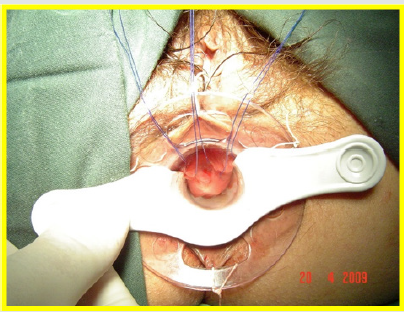
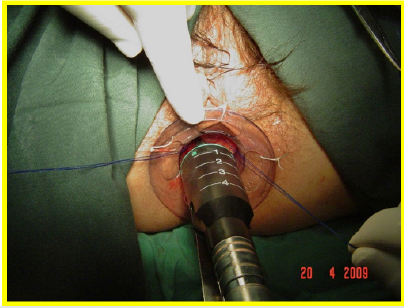
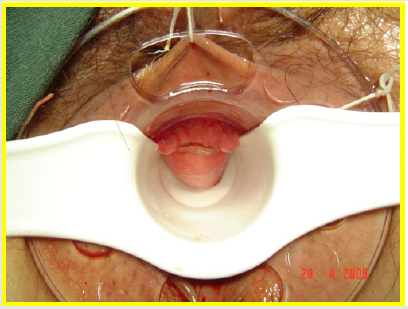
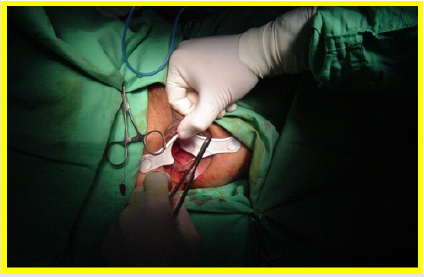
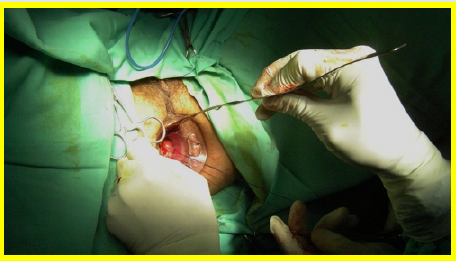
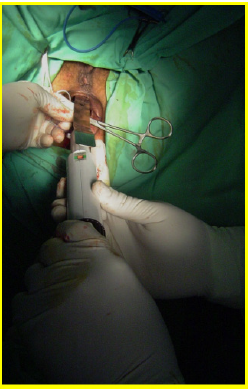
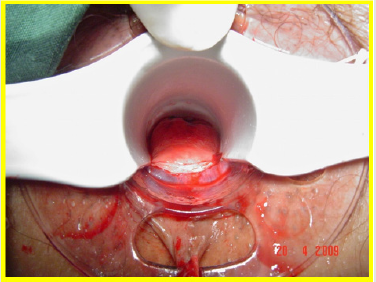
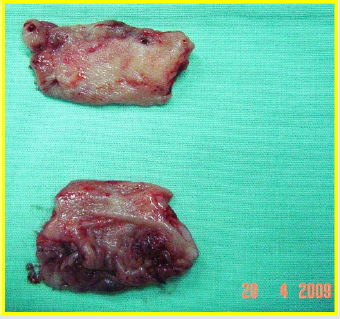
All the patients underwent surgery in gynecologic position with spinal anesthesia. The anoscope of the hemorrhoidopexy set was inserted. First, we proceeded in anterior side, doing points of suture separated in X with Prolene suture 2/0 with SH Needle ® (Ethicon inc.) in the rectocele vertex (12 hour) and at the ends (9 hour and 3 hour) including mucosa, submucosa and muscular of the rectum. Afterwards, a shot of stapler designed for hemorrhoidopexy was done, with previous protection of the posterior side with ductil valve. Once the device was removed, hemostasis at the end of the suture line was found, performing hemostasis systematically, with resorbable material (Figures 1,2,3 & 4). Once the forward face was finished, it was proceeded in the same way with the posterior side, placing the stitches in hours 6,9 y 3 at the same level than the previous side (Figures 5,6,7,8 & 9). During the immediate postoperative period, continuous intravenous analgesia with Diclofenac + Hydrocortisone was supplied. Once the anesthesia wore off, active movement was indicated. At the moment of the medical discharge, analgesia with AINES and opioid booster as demanded, were prescribed. The postoperative complications were recorded according to the Dindo and Clavien Classification (2004) [3]. The medical checks were made after 10 days, 1 month and every six months postoperative with medical interrogation and proctological examinations.
Results
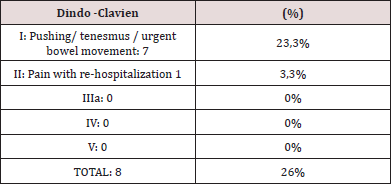
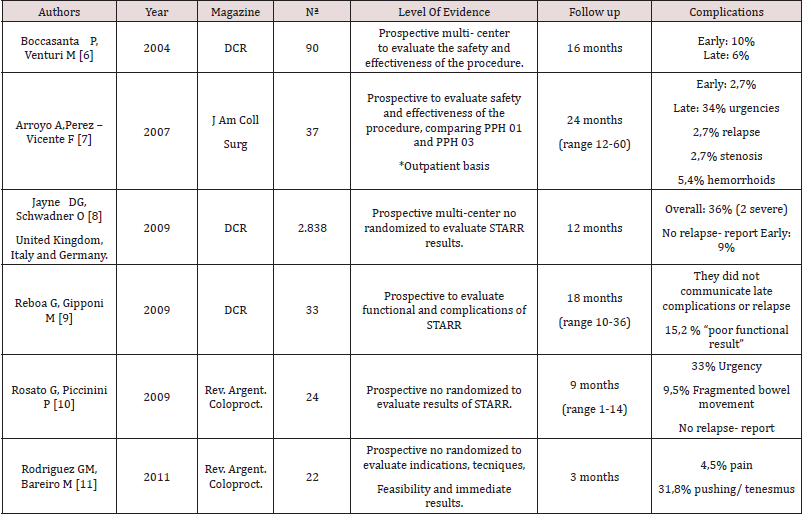
Between January 2009 to January 2019 ,30 women underwent surgery with STARR procedure for constipation for ODS caused by Rectocele with or without rectoanal intussusception. All the patients that were operated were women. The average age was 58, 5 years old (age range 26-76). Functionally, the patients presented a ODS Score greater or equal to 12 during the preoperative period in addition to the various symptoms of ODS ( excessive bowel effort, emptying of the bowel in stages, feeling of incomplete bowel emptying, rectal bleeding, dyspareunia, recurrent urinary tract infections) all of them refered vaginal, anal or perineal fingering to complete the faeces evacuation. 29 surgeries were done with PPH 03 ® (Ethicon inc.) device, which represents 96,6% of our serie; 1 with PPH 03® (Ethicon inc) devices 3,4 %. The average operative time was of 40 minutes in 28 patients (93,4%) to whom only STARR was done, in 2 patients (6,6%) two simultaneous procedures were done in the pelvis, alongside with the Gynecology team prolonging the surgery. 28 patients (93,4 %) stayed hospitalized 24 hours. The last 2 cases of the series were operated under outpatient surgery regimen (6,6%). The global index of complications was of 26,6%, that have been grouped according to Dindo-Clavien (Table 1).
In respect of early results, the improvement in the index of ODSS was significant: from an average of 26/37 (range 33 to 19) to 5/ 37 range 12 to 1) one month after the surgery. The distant monitoring was on an average of 96 months (range 6-120). 8 patients (30%) had recurrence of some symptom of ODS after 12 months of monitoring, primarily excessive bowel effort, even though all of them solved it with fingering or manual maneuvers in order to empty the bowel and improved their life quality. 3 patients (10%) passed away (for causes not related to the surgery) and in 2 patients (6,6%) a PPH procedure was done, both due to a mucosal hemorrhoidal prolapse grade IV with bleeding. We didn’t carry out another anal, perianal or abdominal surgery to treat ODS in the rest of the patients Table 2. The satisfaction rate of the patients with the procedure was higher than 80% and 90% (27 patients) would recommend the approach or would undergo surgery again.
Discussion
With the increase in life expectancy over the last decades,
anatomical and functional colorectal conditions take an important
place during medical consultations, most probably sub recorded
due to cultural issues (embarrassment, disinformation or habitforming).
Since they affect the patients’ life quality considerably,
it is crucial to be able to offer them the appropriate treatment
that relieves them and provides an acceptable relational life.
Constipation for Obstructed Defation Syndrome usually represents
a multifactorial entity and is estimated that affects between 15% to
20% of adult women [4,7-9]. The comprehension of the anatomical
and functional defects that brings this kind of constipation has
led us to propose STARR as a valid alternative to improve it
when it is caused by large rectocele, associated or not to recto
anal intussusception. Noting that stapled hemorrhoidopexy also
corrects small rectoceles and improves significantly the symptoms
of OTS, Antonio Longo carried out cadaverous and dynamic studies
(VDFG and Endoanal ultrasound- test), in conclusion, the distal
prolapse of the rectum is the cause of OTS. Initially compensated
by physiological mechanisms, various modifications became
permanent and determine severe effect on life quality. Based on this
finding, proposes that circumferential resection of rectal prolapse
could be considered as an effective and rational treatment for the
OTS. However, notes that possible neuromuscular injuries, that
were found are irreversible and cannot be corrected with surgery
[1].
From this description, controlled studies were undertaken
in order to evaluate its feasibility and efficacy. Regadas and Col.
[5] performed three-dimensional Endoanal ultrasound and
manometry on women with or without rectocele in order to
compare the anatomy of the anal canal and the anorrectal ring
in both of them. Their findings showed that the rectocele begins
in the superior anal canal and then involves the rectum; and that
the herniation of the rectum caused by excessive and prolonged
strain could explain the origin of the rectocele; and that the vaginal
delivery doesn’t seem to have a rol in its pathogenesis ( except in the case of big obstetric traumas) and that rectal herniation
could be promoted by excessive intra-anal pressures resulting in
intussusception and rectocele and could be aggravated by elevated
intrabdominal pressures. These anatomophysiological foundations
set out the bases of the respective technique. In terms of its
feasibility and results, Boccasanta et al. [6] published the results of
a prospective multicenter study, designed to evaluate the safety and
the results of the technique, the average follow-up of 16 months.
They operated 90 patients (87 women) 10%of early complications
were reported approximately and 6% of late complications (urgent
bowel movement, gases incontinence and stenosis) there were no
mortalities, or pelvic sepsis. They concluded that the method is safe
and effective, with acceptable complication rate and the solving of
the symptomatology; make us aware of the need of skilled surgeons
and the correct patient selection.
Arroyo et al. [7] studied the safety and efficacy of the
procedure and comparing the use of the two devices for stapled
hemorrhoidopexy (PPH 01® and PPH 03®). It is worth noting that
all the surgeries were performed on an outpatient basis. Low early
complications rate and distanced were reported with an average
follow-up of 24 months, reporting 1 patient with rectocele relapse
(2,7 %). They said that STARR is safe and effective as an alternative
for constipation caused by OTS treatment and recommend the use
of the PPH 03® device in order to reduce the risk of post-operative
bleeding.
At 2009 Jayne et al. [8] present the results of the European
Register of STARR, designed with the aim of evaluating its safety and
results throughout 12 months of follow- up. Great Britain, Italy and
Germany are included. Although with different evaluative methods
in respect of life quality and functionality, they collected 2838
surgery patients, 83% women. Having an overall complications rate
of 36%, mainly emergency, persisten pain, bleeding and urinary
retention, with 2 cases of severe complications, with no mortality.
They show a clear improvement of the symptoms of OTS that
remain during the year of the follow-up. There are no pathology
or symptoms relapse reported. They present the procedure as safe
and effective, highlighting the points concerning the experience
of the surgeon and the correct patient selection. Likewise, other
studies proved acceptable short- term results [9]. In Argentina,
Rosato-Piccini [10] and our working group [11] evaluated its
feasibility and immediate results with similar patients’ samples. It
was proved that technically is possible to perform it with acceptable
morbidity, emphasizing on the careful selection of the candidates
and the need of training in the handling of the pelvic floor and
mechanical sutures. Coincidentally, we reported some cases treated
in cooperation with urologists and gynecologists, without consider
them as a contraindication to the method.
The technique is safe, feasible and reproducible, and could
be offered as an option to selected patients. The questioning
continued in terms of long- term functional results, and the cost
of the procedure. Providing a retrospective analysis of 450 cases
submitted to surgery in 10 years, with a follow up in period of at
least 5 years Guttadauro A et al. [12]refers to the urgent emptying
of the bowels as the mainly early complication (27,8%) and 6
patients (1,3%) with rectal perforation subjected to treatment,
with no mortality due to the method. Functionally, a significant
reduction of symptoms is evidenced, which remains on average 6
after 5 years, and doesn’t register relapse of prolapse or rectocele.
Once again, this working group insists in the correct selection of
patients and the surgical team’s experience, considering the severe
complications only relative to the first phase of diffusion of the
technique. The first study with 10 years of follow-up was published
in in 2017 by Di Visconti et al. [4]. It is about a retrospective
analysis of a retrospective data base about 74 consecutive patients
subjected to surgery with STARR between 2005-2006; severe
complications weren’t registered, 60 of these patients completed
the follow- up to 10 years, where the recurrence of OTS was defined
as the onset of symptoms that affects the patient with rectocele
+/- Intussusception confirmed with VDGF. No patients presented
recurrence of symptoms during the first year of follow up. After 10
years 24 patients (40%) had recurrence of symptoms, 12 patients
agreed to be subjected to clinical examination, VDGF and manometry.
11 of them were subjected to a new procedure (Laparoscopic
rectopexy with ventral mesh, conventional abdominal approach
with promontopexy, posterior colporrhaphy and ventral rectopexy
with mesh + STARR in one patient). In 10 years, 35% of the patients
were satisfied with the surgery and 28% would recommend the
operation, while 21% wouldn’t choose the technique basically
because of the urgent emptying of the bowels and the pain they
suffered from. The authors point out as predictive factors of
recurrence: female sex, previous urogynecology surgery, previous
anorectal surgery and high rates of the ODSS questionnaire. They
concluded that STARR determines a significant improvement of
symptoms at short-term, being less effective in the long- term, that
the possibility of relapse should be raised to the patient, especially
to those who have the predictive factors.
In another analysis of the functional results, Giarratano et al.
[13] report a short operative time, with no mortality and 23% of
morbidity over 262 surgery patients. In an average of 79 months of
follow-up, 85% of the patients remain without OTS symptoms, with
86% of satisfaction, with no Dyspareunia. 10 patients experienced
recurrence, with 3 re-operative surgery (ventral rectopexy). Our
study has some limitations. It is a single center experience an
observational study. At limited number of the sample, we could add
the fact that we didn’t count with anorectal manometry during the
evaluation and the follow up; we exclude animus or paradoxical
contraction through physical exam and images, although subjected
to the experience deficiencies. Neither we documented with
studies the post- operatives’ results. We believe however that the
solving of the symptoms, the satisfaction index achieved, and the
fact of improving the relational and life quality and of the patients
represent a relevant fact of the contribution.
Conclusion
We considered the STARR technique as safe and effective, presented as an alternative that the specialist could offer to the difficulty in the emptying of bowel cause by rectocele with or without intussusception that does not respond to a medical treatment. It requires experience in the handlig of mechanical sutures in orifice pathology and presents good functional results at short term. It has clear anatomical and functional foundations. The accurate indication and selection of patients seems to increase its efficiency. In the long- term an average of patients could have relapse of symptoms and that situation should be raised to the patients before the surgical intervention.
References
- Longo A (2004) Obstructed defecation because of rectal pathologies. Novel surgical treatment: Stapled Transanal Rectal Resection (STARR). Proceedingos of the 15th Annual Colorectal Disease Symposium. Ft. Lauderdale, Florida, USA.
- Rosato G, Piccinini P (2009) Tratamiento del Síndrome de Defecación Obstruida mediante la técnica STARR (Stapled Trans Anal Rectal Resection). Rev Argent Coloproct 20: 216-226.
- Dindo D, Demartinez N (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2): 205-213.
- Schiano di Visconte M, Nicoli F (2018) Clinical outcomes of stapled transanal rectal resection (STARR) for obstructed defaecation syndrome at 10-year follow-up.
- Regadas FSP, Muras Regadas SM (2006) Anorectal three-dimensional endosonographic and anal manometry in assesing anterior Rectocele in women: a new pathogenesis concept and the basic surgical principle. Colorectal Dis 9: 80-85.
- Boccasanta P, Venturi M (2004) Stapled Transanal Rectal Resection for Outlet Obstruction: A prospective, Multicenter Trial. Dis Colon Rectum 47(8): 1285-1297.
- Arroyo A, Perez-Vicente F (2007) Evaluation of the Stapled Transanal Rectal Resection Technique with two staplers in the treatmento of Obstructive Defecation Syndrome. J Am Coll Surg 204(1): 56-63.
- Jayne DG, Schwadner O (2009) Stapled Transanal Rectal Resection for Obstructed Defecation Syndrome: One-Year Results of the European STARR Registry. Dis Colon Rectum 52(7): 1205-1214.
- Reboa G, Gipponi M (2009) The Impact of Stapled Transanal Rectal Resection on Anorectal Function in Patients with Obstructed Defecation Syndrome. Dis Colon Rectum 52(9): 1598-1604.
- Rosato G, Piccinini P (2009) Tratamiento del Síndrome de defecación obstruída mediante la técnica de STARR (Stapled Trans Anal Rectal Resection). Rev Argent Coloproct 20: 216-226.
- Rodríguez GM, Bareiro MJ (2012) Utilidad de los dispositivos de sutura mecánica circular para técnicas endoanales. Rev. Argent. Coloproct 23(4): 207-211.
- Guttadauro A, Chiarelli M (2017) Value and limits of Stapled Transanal Repair for Obstructed Defecation Syndrome: 10 years-experience with 450 cases. Asian Journal of Surgery.
- Giarratano G, Toscana C (2017) Stapled transanal rectal resection for the treatment of rectocele associated with obstructed defecation syndrome: a large series of 262 consecutive patients. Tech Coloproct.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...