Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Necrotizing Pancreatitis with Mediastinal Abscess Formation Volume 3 - Issue 5
JStephen N Fung1*, Sascha Vaghiri1, Johannes G Bode2, Lino M Sawicki3, Andreas Krieg1, Alexander Rehders1 and Wolfram T Knoefel1
- 1Department of Surgery (A), Heinrich-Heine-University and University Hospital Duesseldorf, Moorenstrasse 5, 40225 Duesseldorf, Germany
- 2Department of Gastroenterology, Infectiology and Hepatology, Heinrich-Heine-University and University Hospital Duesseldorf, Moorenstrasse 5, 40225 Duesseldorf, Germany
- 3Institute of Diagnostic and Interventional Radiology, Heinrich Heine-University and University Hospital Duesseldorf, Moorenstrasse 5, 40225 Duesseldorf, Germany
Received: November 29, 2019; Published: December 09, 2019
Corresponding author: Stephen N Fung, Department of Surgery (A), Heinrich-Heine-University and University Hospital Duesseldorf, Moorenstrasse 5, 40225 Duesseldorf, Germany
DOI: 10.32474/SCSOAJ.2019.03.000175
Abstract
Mediastinal abscess formation is a rare thoracic complication of acute pancreatitis with a high mortality. Pleural effusion and pneumonia represent the most frequent complications. Here we report the case of a 52 years old patient with a history of alcoholinduced acute pancreatitis, who was admitted at our hospital with acute abdominal pain. Contrast-enhanced Computed Tomography showed a necrotizing pancreatitis with mediastinal abscess formation. Endosonographic puncture and subsequent placement of a transesophageal pigtail drainage in the necrotic cavity led to complete evacuation of the infected mediastinal necrosis. To our knowledge this therapeutic approach has not been described for such a case before and seems to be an effective therapy of mediastinal abscess formation.
Keywords: Mediastinal abscess formation; necrotizing pancreatitis
Introduction
Necrotizing pancreatitis (NP) is a severe complication of acute pancreatitis (AP) with high mortality and morbidity rates up to 27% [1]. The main cause of death is the infection of the necrotic tissue, which is associated with poor prognosis [2]. Mortality is approximately 15% in patients with necrotizing pancreatitis and in cases with infected necrosis up to 30-39% [3-5]. Mediastinal necrosis is a rare complication of AP and only few cases have been reported until now [6-8]. The common thoracic complications of AP are pleural effusions and pneumonia [9,10]. Some reported rare complications include cardiac tamponade [11,12], pancreaticopleural fistula with recurrent pleural effusion, hemothorax or mediastinitis [13- 15] and mediastinal pseudocyst with pneumonia [16-18]. In this case, we report a patient with mediastinal abscess formation, a rare complication of AP which was treated successfully with endoscopic placement of a transesophageal pigtail drainage in the necrotic cavity. Using per oral endosonographic the abscess formation was clearly located and measured. Afterwards puncture was performed with a special puncture needle (Giovannini Needle Wire Oasis, FA Cook) and the tract was subsequently dilated (Hurricane balloon catheter) up to 6 mm. Thereafter a 10 Fr double-pigtail drainage was placed under fluoroscopic control. The pigtail catheter drained the abscess from the abscess cavity into the esophagus, leading to a complete evacuation of the mediastinal abscess formation [19-21].
Case Report
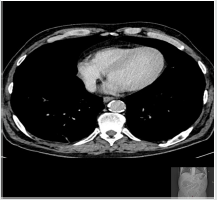
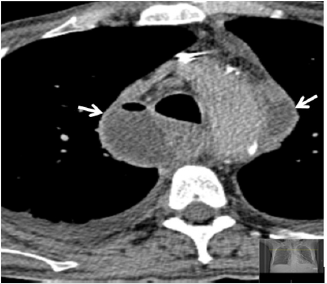
A 52 years old patient with a history of alcohol-induced necrotizing pancreatitis previously diagnosed with Contrastenhanced Computed Tomography (CECT) scan and treated conservatively at the Department of Internal Medicine of our university hospital was admitted in January 2016 at our emergency department with acute abdominal pain. Two weeks before the patient was discharged from hospital after being conservatively treated by the above clinical diagnosis. Clinical examination suggested no thoracic complication, but a recurrence of acute necrotizing pancreatitis confirmed with laboratory values and CECT scan (Figures 1a & 1b) [22-25].
Figure 1a: CECT revealed a walled-off-pancreatic necrosis, a rare complication of acute pancreatitis which often results to formation of pancreaspseudocyst or peripancreatic fluid collection.

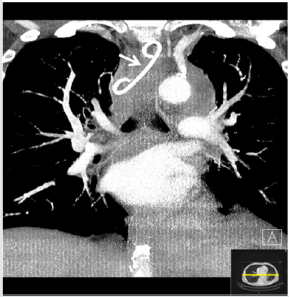
Figure 2: CECT showed progress of necrotizing pancreatitis with increased volume of the peripancreatic fluid collections.

The pre-existing medical history of the patient was: gastritis, steatosis hepatis, status post myocardial infarcted 2005 and 2010, arterial hypertonia and hyperlipoproteinemia. Blood chemistry on admission showed increased levels of leucocytes (22.6 x 1000/μl), C-reactive protein (CRP; 31.6mg/dl) and serum amylase (679U/L). Other laboratory values such as serum calcium, potassium, sodium, urea, amylase in urine and liver values were normal. The patient was admitted at our intermediate care unit (ICU), where the patient´s condition significantly improved after about one month of conservative therapy with antibiotics, analgesia and intravenous fluid substitution. One month later during clinical course the patient suddenly developed fever, acute abdominal pain, dyspnea and high levels of leucocytes. CECT-scan showed a progression of the necrotizing pancreatitis with increased volume of the peripancreatic fluid collection as well as ascites (Figure 2) [26-29]. In addition, bilateral pleural effusions became evident (Figure 3).
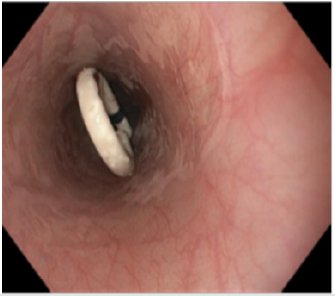
Because of the high risk of bowel perforation, image-guided percutaneous catheter drainage of the necrotic peripancreatic fluid collection was not performed. Instead a trans gastral drainage was established via endosonographic puncture, subsequent dilatation and placement of three pigtail catheters into the necrotic cavity (Figure 4) resulting in a enough draining of the fluid. The pleural effusions were drained by chest tube insertion. Laboratory analysis of the pleural effusion showed normal levels of serum amylase. After this intervention, the condition of the patient improved fast and after a few days of intensive care treatment the patient was transferred to the normal hospital ward. To further evaluate the structure of the pancreatic duct, a magnetic resonance cholangiopancreatography (MRCP) was performed, showing a large pseudocyst along the pancreatic tail but no pancreatic pleural fistula or stone in the pancreatic duct (Figure 5) [30-34].
Figure 4: After puncture of the necrotic peripancreatic fluid collection with placement of 3 double-pigtail catheters.
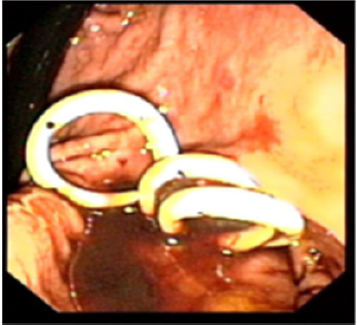
Figure 5: MRCP revealed no pancreaticopleural fistula. A pancrespseudocyst was detected along the pancreatic tail.
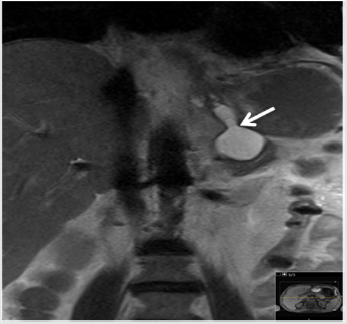
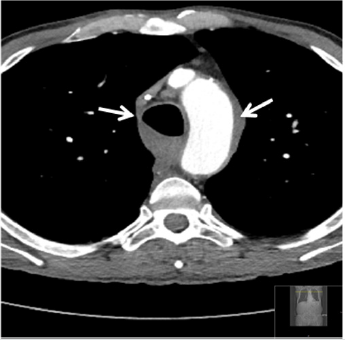
Figure 6: Chest CT scan shows mediastinal abscess with trapped air adjacent to the esophagus (arrow on the right side) and aortic arch (arrow on the left side).
Five weeks later, the patient suddenly developed acute thoracic pain, dyspnea, fever and hypertensive crisis. Blood level of leucocytes and CRP were also elevated. The immediately performed CECT displayed a posterior mediastinal abscess formation with supra-carinal location as cause of the patients deteriorating condition. Because of persisting thoracic pain, dyspnea and hemodynamic instability, the patient was again transferred to the intermediate care unit, where antibiotics, analgesia und controlled fluid substitution was applied (Figure 6). Based on the unsuitable abscess localization in the posterior mediastinum, CTguided percutaneous drainage placement could not be performed safely. In addition, by using this route there was a risk of bacterial contamination of the pleural space. Thus, we decided to perform a per-oral endoscopy with transesophageal puncture accompanied by simultaneous placement of a double-pigtail drainage in the necrotic cavity (Figures 7 & 8).
Figure 8: Maximum intensity projection CT imaging shows the position of pigtail drainage in the thoracic cavity.
One day after the intervention, the patient´s clinical condition significantly improved. During the following days, the clinical symptoms were relieved and blood leucocytes normalized. The follow-up CT scan during the clinical course after intervention, suggested a significant regression of the mediastinal (Figure 9) as well as of the peripancreatic and abdominal necrosis. After the intervention, the patient’s situation stabilized with no relapse since then. The trans gastral und transesophageal pigtail drainages were removed after CT scan control one month later without any additional complication. The Barium swallow examination showed no pathologic results. The patient was then enterally fed and remained under observation in our clinic.
Figure 9: Follow-up Chest CT after removing the transesophageal pigtail showed almost complete necrosectomy of the mediastinal abscess. Pleural effusion also completely decreased on both sides.
Discussion
Mediastinal abscess formation is a rare thoracic complication
of acute pancreatitis and only a few cases have been reported till
now [6-8]. The common thoracic complications of AP are pleural
effusions and pneumonia [9,10]. In the most cases patients died
before or at time of diagnosis. To date less is known about the
therapeutic options at time of diagnosis. Related to other illnesses
with mediastinal abscess formation such as Berhane’s syndrome or
anastomosis leak after esophagectomy, minimal invasive techniques
such as video-assisted thoracoscopy, CT-guided percutaneous
drainage, cervical drainage and transesophageal endoscopic
ultrasound (EUS) have been described as effective management
strategies in these cases [30,31,32,33]. The mechanism of pleural
effusion and abscess formation is unknown, but some theories have
been reported. Fistolous communication between a pancreatic
pseudocyst and the pleural space due to pancreatic pleural fistula,
lymphatic transportation of amylase [27] and circulating enzymes
[28,29] belong to the most common theories for pleural effusion
formation. In our case, no pancreatic pleural fistula was detected
in the MRCP. Normal levels of amylase in the pleural effusion also
foreclosed the existence of a fistula.
The most used approach to infected pancreatic necrosis has
been open surgical necrosectomy, but it is associated with high
morbidity (34-95%) and mortality (11-39%), due to physical stress
of the laparatomic debridment [19-22]. In the last two decades,
treatment of necrotizing pancreatitis has evolved and emerged
from invasive to less invasive techniques such as laparoscopy
[23], interventional radiology [24-25] and endoscopy [26]. These
methods are nowadays alternatives or complimentary approaches
to surgical necrosectomy and may substitute or delay surgical
intervention. Here we report the case of a patient with necrotizing
pancreatitis who developed mediastinal abscess formation.
However, image-guided percutaneous catheter drainage (PCD),
which is the first step approach (in the step-up approach) to drain
necrotic collections before endoscopic debridement or surgery are
considered [22] was not implemented because of unfavorable supracarinal
abscess localization at the posterior mediastinum. Thus,
the patient was successfully treated with per-oral transesophageal
endoscopic necrosectomy.
Follow-up CT scan showed a regression of the mediastinal
abscess and served as therapy control till the double-pigtail
drainage was removed. After removal of the drainage, a barium
swallow examination of the upper gastrointestinal tract did not
show any leakage or fistula of the esophagus, which are possible
complications after removal of a pigtail drainage. Likewise, other
potential complications, which could emerge from endosonographic
puncture and placement of a pigtail drainage such as injury of
neighboring organs (e.g. the aortic arch or trachea) or dislocation of
the pigtail drainage did not occur. Therefore analogous to the wellknown
endoscopic trans gastral necrosectomy, which is also used to
relieve infected peripancreatic or pancreatic necrosis, endoscopic
transesophageal necrosectomy may also represent an effective
therapy for patients with infected supra-carinal mediastinal fluid
collection or abscess at time of diagnosis. In summary these data
suggest that endosonographic guided placement of transesophageal
drainage is enough to adequately manage mediastinal abscess
formation due to necrotizing pancreatitis. This approach requires
a multidisciplinary approach in specialized centers with a high
expertise in interventional endoscopy and a good intensive care
unit.
Author contributions
Fung SN. designed and wrote the report, analyzed and interpreted the data; S. Vaghiri and Rehders A were attending doctors of the patient; Bode J. performed the transesophageal puncture; Sawicki L.M analyzed the CT scans; Krieg A, Rehders A. and Knoefel WT critically revised the report and gave important intellectual input.
Institutional review board statement: The study was reviewed and approved by the Independent Research Ethics Committe at the Medical Faculty of the Heinrich-Heine-University of Duesseldorf (Study No. 6128)
Informed consent statement: The study participant provided informed written consent prior to study enrollment
Core tip Mediastinal abscess formation is a rare thoracic complication of acute pancreatitis. This case reports a patient with mediastinal abscess formation due to necrotizing pancreatitis who was successfully treated with endosonographic puncture and subsequent placement of a transesophageal pigtail drainage in the necrotic cavity. Fung SN, Vaghiri S, Bode JG, Sawicki LM, Krieg A, , Rehder A, Knoefel WT. Necrotizing pancreatitis with mediastinal abscess formation
Conflict of Interest
There is no conflict-of-interest between authors.
References
- de Beaux AC, Palmer KR, Carter DC (1995) Factors influencing morbidity and mortality in acute pancreatitis. an analysis of 279 cases Gut 37(1): 121-126.
- Walter Bugiantella, Fabio Rondelli, Marcello Boni, Paolo Stella, Andrea Polistena, et al. (2016) Necrotizing pancreatitis: A review of the interventions. International Journal of Surgery 28: S163-S171.
- Banks PA, Freeman ML (2006) Practice parameters committee of the American college of gastroenterology. Practice guidelines in acute pancreatitis Am J Gastroenterol 101(10): 2379e2400.
- Frossard JL, Steer ML, Pastor CM (2008) Acute pancreatitis. Lancet 371: 143e152.
- Petrov MS, Shanbhag S, Chakraborty M, Phillips AR, Windsor JA (2010) Organ failure and infection of pancreatic necrosis as determinants of mortality in patients with acute pancreatitis. Gastroenterology 139(3): 813-820.
- Sˇtimac D, Niksˇic´M, Sincic´, Mijandrusic´, Depolo M, et al. (2007) Mediastinal Necrosis in Acute Pancreatitis - Case Report. Zentralbl Chir 132: 155-157.
- Valverde A, Hammel P (1999) Mediastinal and cervical diffusion of necrosis infiltration in acute pancreatitis. Gastroenterol Clin Biol 23: 137-144.
- Kratz HW, Hamper P (1982) Acute necrotising alcoholic pancreatitis with abscess formation in the mediastinum. ROFO Fortsch Geb Rontgenstr Nuklearmed 136: 262-265.
- Kim YT (2005) Medical management of acute pancreatitis and complications. Korean J Gastroenterol 46: 339-344.
- Kim HY, Seo DW, Lee TY, Kang HH, Lee SK, et al. (2002) A Clinical review on chronic pancreatitis. Korean J Gastroenterol 40: 191-196.
- Jung HC, Nah DY, Park KU, Lee CH, Jung SY, et al. (2001) A Case of cardiac tamponade caused by acute pancreatitis. J Korean Soc Echocardiogr 9: 66-69.
- In Soo Choe, Yong Seok Kim, Tae Hee Lee, Sun Moon Kim, Kyung Ho Song, et al. (2014) Acute mediastinitis arising from pancreatic mediastinal fistula in recurrent pancreatitis.
- Park SY, Jang JY, Lee SE, Yang SH, Kim SW (2006) Pancreaticopleural fistula: complication of chronic pancreatitis. Korean J Hepato-Biliary-Pancreat Surg 10: 29-33.
- Sul YH, Shin HS, Lee KH, Chun KS, Song IS (2009) Pancreaticopleural fistula with hemothorax. J Korean Surg Soc 76: 187.
- Nam KW, Chae HS, Kim HR, Kwok SK, Lee BI, et al. (2002) A case of mediastinal pancreatic pseudocyst presenting with pneumonia. Korean J Gastroenterol 40: 414-421.
- Lee JS, Kim YS, Chang WC, Lee JW, Moon JS, et al. (2003) Cardiac tamponade complicated by chronic recurrent pancreatitis. Korean J Med 65: S693-S697.
- Maeng HY, Jung JH, Lee SW, Park MS, Chung JH, et al. (2002) A Case of mediastinal pancreatic pseudocyst. Tuberc Respir Dis 52: 271-277.
- Park SH, Kim SJ, Kim EJ, Lee MH, Kim HS, et al. (1999) A Case of mediastinal pancreatic pseudocyst treated with octreotide. Korean J Gastroenterol 34: 417-421.
- Traverso LW, Kozarek RA (2005) Pancreatic necrosectomy: definitions and technique. Gastrointest Surg 9(3): 436-439.
- Raraty MG, Halloran CM, Dodd S, Ghaneh P, Connor S, et al. (2010) Neoptolemos, Minimal access retroperitoneal pancreatic necrosectomy: improvement in morbidity and mortality with a less invasive approach. Ann Surg 251(5): 787-793.
- Tan V, Charachon A, Lescot T, Chafaï N, Le Baleur Y, et al. (2008) Endoscopic transgastric versus.
- Freeman ML, Werner J, Van Santvoort HC, Baron TH, Besselink MG, et al. (2012) International multidisciplinary panel of speakers and moderators. Interventions for necrotizing pancreatitis: summary of a multidisciplinary consensus conference, Pancreas 41(8): 1176-1194.
- Fink D (2011) History, goals, and technique of laparoscopic pan-creatic necrosectomy. J Gastrointest Surg 15(7): 1092-1097.
- Freeny PC (1998) Percutaneous CT-guided catheter drainageof infected acute necrotizing pancreatitis: techniques and results. AJR Am J Roentgenol 170(4): 969-975.
- Baril NB (2000) Does an infected peripancreatic fluid collectionor abscess mandate operation? Ann Surg 231(3): 361-367.
- Papachristou GI (2007) Peroral endoscopic drainage/debridement of walled-off pancreatic necrosis. Ann Surg 245(6): 943-951.
- Rockey DC, Cello JP (1990) Pancreaticopleural fistula: reports of 7 patients and review of the literature. Medicine 69: 332-344.
- Mitchell CE (1964) Relapsing pancreatitis with recurrent pericardial and pleural effusion. Ann Intern Med 60: 1047-1053.
- Demuth WE, Rottenstein HS (1964) Case 28-1964, Case records of the Massachusetts General Hospital: Weekly clinopathologic exercises. N Engl J Med 1270: 1248-1251.
- Kahaleh M, Yoshida C, Kane L, Yeaton P (2004) EUS drainage of a mediastinal abscess. Gastrointest Endosc. 60(1): 158-160.
- Son HS, Cho JH, Park SM, Sun K, Kim KT, et al. (2006) Management of descending necrotizing mediastinitis using minimally invasive video-assisted thoracoscopic surgery. Surgical laparoscopy, endoscopy & percutaneous techniques 16(6): 379-382.
- Isowa N, Yamada T, Kijima T, Hasegawa K, Chihara K (2004) Successful thoracoscopic debridement of descending necrotizing mediastinitis. Ann Thorac Surg 77(5): 1834-1837.
- Till Wehrmann MD, Nikos Stergiou MD, Bernd Vogel MD, Andrea Riphaus MD, Ferdinand Kockerling MD, et al. (2005) Endoscopic debridment of paraesophageal, mediastinal abscesses: a prospective case series. Gastronintestinal Endoscopy 62(3): 344-349.
- Nakamura Y, Matsumura A, Katsura H (2009) Successful video-thoracoscopic drainage for descending necrotizing mediastinitis. Gen Thorac Cardiovasc Surg 57(2): 111-115.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...