Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Mucinous Cystadenoma of Ovary-How Large Can They Grow? Volume 6 - Issue 3
T Abinaya Preethi1, Rufus Ranjitsingh1*, SN Saravana Sundaram1, P Jayaganesh2 and Rekha Arcot1
- 1Department of general surgery, Saveetha institute of Medical and technical sciences (SIMATS), India
- 2Department of pathology, Institute of Medical and Technical Sciences (SIMATS), India
Received:May 21, 2021 Published:June 02, 2021
Corresponding author: Rufus Ranjit Singh Edwin, Department of general surgery, Saveetha Medical College and Hospital, Saveetha institute of Medical and technical sciences (SIMATS), India
DOI: 10.32474/SCSOAJ.2021.06.000240
Abstract
Mucinous cystadenomas make up to 15-20% of all epithelial tumors. They are multiloculated cysts lined by epithelium resembling the endocervix. We here present a case of 48-year-old female with mass on the abdomen. Differential diagnosis for mass in the abdomen includes Ovarian tumors, ovarian cysts, abdominal masses.
Keywords: Mucinous Cystadenoma; Abdominal Masses; Ovarian Cyst, ovarian Tumors
Introduction
Epithelial tumors of the ovary represent over 65-75% of all ovarian tumors. Mucinous cystadenomas (epithelial in origin) may originate from tubes, endocervix, endometrium or bladder epithelium. They are more common in middle aged women and rare among adolescents and teenagers. We report a case of large mucinous cystadenoma of left ovary and discuss its etiology, investigations and treatment modalities.
Case Presentation
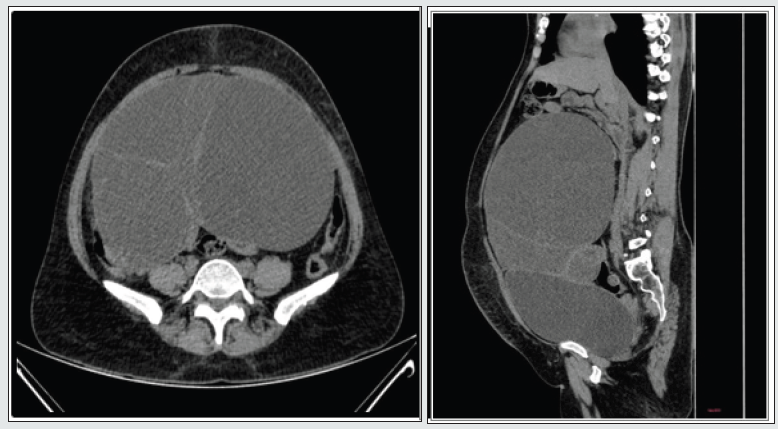
A 48-year-old nulliparous woman presented with complaints of mass in the abdomen over the last 8 years and intermittent dull aching abdominal pain to the general surgery outpatient department. She had no bowel and bladder symptoms. Her menstrual cycles were regular and unremarkable. Examination showed a large swelling occupying the entire abdomen, with a fluid thrill. Investigation with ultrasound abdomen showed a large cystic lesion which on computed tomography showed a well-defined pelvic abdominal cystic lesion of size15.8×22× 22 cms (Figure 1) arising from the left adnexa, extending to the epigastrium superiorly, posteriorly abutting the infra renal aorta, with no solid components, debris or peritoneal nodules (likely representing a benign etiology). The tumour markers were found to be within normal limits as follows. CA-125 was 14U/m (Normal range:<46U/ ml), CEA was 0.40ng/ml (Normal range:0-2.5ng/ml), Beta HCG was <2.39mIU/ml (Normal range:<10mIU/ml) and AFP was 1.42ng/ml (Normal range:<10ng/ml)
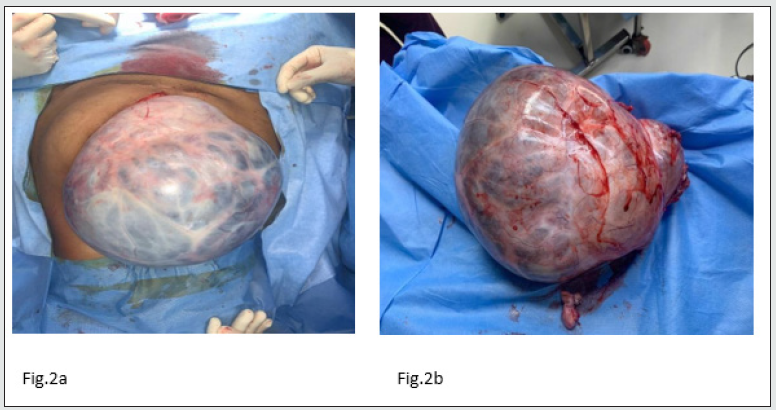
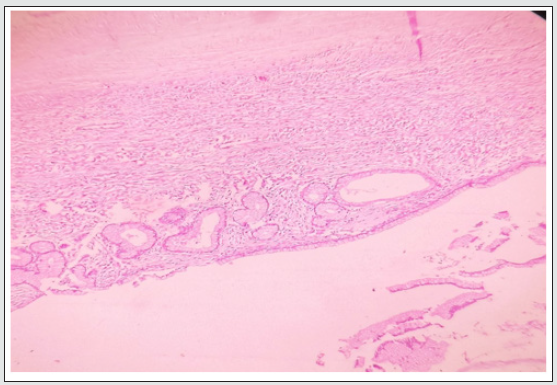
She underwent laparotomy with resection of the ovarian cyst in toto (Figure 2a and 2b) It weighed 5.4kgs and the frozen section was negative for malignancy. She was desirous of conceiving and hence the ovaries and uterus were preserved. The histopathology revealed ovarian stroma with multiloculated cystic neoplasm lined by mucinous columnar epithelium, no stratification or atypia noted. Section also showed tubal mucosa with minimal congestion (Figure 3). Postoperative period was uneventful, and the patient was comfortable at the fourth week follow-up.
Discussion
Epithelial tumors of the ovary include serous, mucinous, endometrioid, clear cell, Brenner and seromucous tumors. Benign mucinous tumors include mucinous cystadenoma and mucinous adenofibroma [1]. Mucinous cystadenomas were formerly referred to as pseudo mucinous cysts, but their contents are not chemically true mucin. Risk factors for ovarian cyst formation include infertility treatment, tamoxifen use, pregnancy, hypothyroidism, maternal gonadotropins, cigarette smoking, and tubal ligation. The risk factors for ovarian adenocarcinoma include family history, advancing age, white race, infertility, nulliparity, endometriosis, history of breast cancer, BRCA gene mutations, and Lynch II syndrome [2]. Mucinous cystadenomas can be classified as benign, borderline and malignant. Benign mucinous tumours represent 40% of all benign ovarian neoplasms. Whole borderline tumours have a low malignant potential and can have an extra ovarian spread in about 10%. On gross appearance, mucinous tumours are large size before being discovered but this does not necessarily indicate malignancy, even when they reach a diameter of 50cms or more and weigh 50 to 150kgs.On average, the mucinous tumours measure 15-30 cms in diameter. Only 10% of primary mucinous cystadenomas are bilateral.
Patients with benign ovarian tumours are usually asymptomatic and discovered incidentally on ultrasound. The symptoms of malignancy might include abdominal pain, pelvic pain, abdominal distension, altered bowel and bladder habits, low back ache, dyspareunia, loss of appetite, loss of weight and early satiety.
Investigations include routine blood investigations and tumour markers such as CEA, CA-125, beta HCG,AFP levels [3] . The USG sensitivity and specificity for detecting ovarian malignancies is 84% and 82% respectively. While CT had shown sensitivity and specificity of 81% and 87% respectively. MRI has a sensitivity and specificity of 76% and 97% respectively, while in a contrast enhanced MRI the sensitivity and specificity increases to 81% and 98% respectively [4,5]. The primary advantage of using MRI in the evaluation of ovarian masses is the ability to employ this modality in the characterization of tissue. The presence of fat, haemorrhage, mucin, fluid, and solid tissue within an ovarian mass can be determined with the aid of MRI. Features suggestive of malignancy include a thick irregular wall, thick septa, papillary projections, and a large soft-tissue component with necrosis. Ancillary findings of pelvic organ invasion; spread to the peritoneum, omentum, or mesentery, ascites and adenopathy are also suggestive of malignancy [6, 7].
Treatment of ovarian cysts depends on the patient’s age, size of the cyst and its histopathological nature. Conservative surgery naming ovarian cystectomy, salpingo-oophorectomy are adequate in case of benign lesions [8,9]. Meanwhile for larger ovarian masses with a risk of malignancy, laparotomy and intraoperative intraperitoneal exploration and a biopsy of the diaphragm, omentum, the Pouch of Douglas and right and left side colon needs to be done.
Conclusion
Mucinous cystadenomas lie at the benign end of the spectrum of ovarian tumours, rarely recur and are pretty innocuous in spite of the large size with which they present. After excluding malignancy, the challenge lies in complete excision without spillage.
References
- Kurman RJ, Carcangiu ML, Herrington S, Young RH (2014) World Health Organization classification of tumours of the female reproductive organs. (4th Edn). Lyon, France: IARC.
- Yemelyanova AV, Vang R, Judson K, Wu LS, Ronnett BM et.all (2008) Distinction of primary and metastatic mucinous tumors involving the ovary: Analysis of size and laterality data by primary site with reevaluation of an algorithm for tumor classification. Am J SurgPathol 32(1): 128-138.
- Engelen MJ, de Bruijn HW, Hollema H, et al (2000) Serum CA 125, carcinoembryonic antigen, and CA 19-9 as tumor markers in borderline ovarian tumors. GynecolOncol 78(1): 16-20
- Micco M, Sala E, Lakhman Y, Hricak H, Vargas HA, et al(2014) Role of imaging in the pretreatment evaluation of common gynecological cancers. Women’sHealth (Lond).
- Togashi K (2003) Ovarian cancer: The clinical role of US, CT, and MRI. EurRadiol 13(suppl 4): 87-s104
- Mutch DG, Prat J (2014) FIGO staging for ovarian, fallopian tube and peritoneal cancer. GynecolOncol 133(3):401-404
- Brun JL, Fritel X, Aubard Y, et al (2014) Management of presumed benign ovarian tumors: Updated French guidelines. Eur J ObstetGynecolReprod Biol 183:52-58.
- Fatema N, Mubarak Al, Badi M (2018) A Postmenopausal Woman with Giant Ovarian Serous Cyst Adenoma: A Case Report with Brief Literature Review. Case Rep Obstet Gynecol 5478328.
- Gonzalez DO, Minneci PC, Deans KJ (2017) Management of benign ovarian lesions in girls: A trend toward fewer oophorectomies. Curr Opin Obstet Gynecol 29(5):289-294.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...