Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Misery of the Forgotten Stent : Complications Due to Stentolith Volume 6 - Issue 4
Khalilur Rahman, Sana Aboosalih* and K Vignaradj
- Department of general Surgery, Saveetha medical college, India
Received:September 14, 2021; Published:September 28, 2021
Corresponding author: Sana Aboosalih, Department of general Surgery, Saveetha medical college, India
DOI: 10.32474/SCSOAJ.2021.06.000243
Introduction
Forgotten or stents retained in the biliary ducts for a prolonged period without follow-up can lead to serious complications.
Case Report
51 years old man, non smoker, non alcoholic, presented to the General Surgery OPD at Saveetha Medical College with complaints of pain in the epigastric and right hypochondriac region, associated with yellowish discoloration of sclera for 4 days. He also complained of fever during this period which was not associated with chills or rigor. He gave past history of pain in the same region on and off for the past 2 years which aggravated on eating food. Patient gave history of passing high colored urine and pale stools. with ortherwise normal bowel and bladder habits. He had no complaints of nausea, vomiting or pruritus. Patient underwent ERCP with stent placement and cholecystectomy in 2013 for cholelithiasis with CBD stone. Patient did not have any other comorbidities or significant family history.
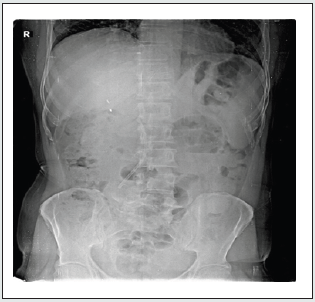
On examination patient was found to have icterus. Per abdomen examination showed and no obvious mass seen, on palpation tenderness present in epigastric and right hypochondriac region. Previous laparoscopic cholecystectomy wound is normal. Investigations showed Liver function test to be grossly deranged with total bilirubin 11.2 mg/dl, direct bilirubin9.0 mg/dl, SOGT 54 IU/L, SGPT 32 IU/L and alkaline Phosphatase 230 IU/L, indicating a picture of obstructive jaundice with on going active cholangitis. Patient was started on IV Antibiotics. Xray erect abdomen showed the stent present insitu (Figure 1).
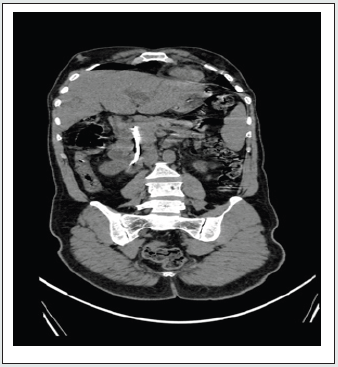
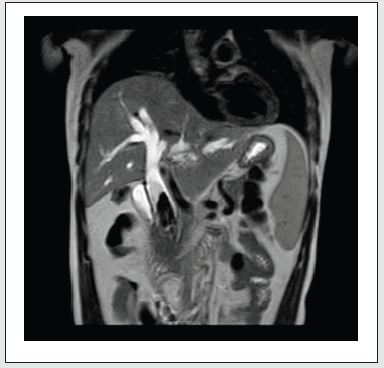
USG abdomen was done which showed dilated CBD with dilation of hepatobiliary radicles, hence an MRCP study was done showing Choledocholithiasis in the extra hepatic portion of mid distal CBD with dilatation of the proximal biliary tree and forgotten stent in situ (Figure 2 and 3). Patient was taken up for open choledochoduodenostomy with stent removal. Post operatively patient improved symptomatically, however patient had fever spikes which was managed conservatively, antibiotics were changed according to bile culture report which showed E. coli sensitive to Imipenem. Total Bilirubin and direct bilirubin reduced progressively each day. On POD 6 drain tubes were removed. Patient was tolerating diet and discharged. On routine follow up patient had no complaints.
Discussion
It is seen that approximately 10-15% of patients diagnosed with cholelithiasis have concomitant stones present in the common bile duct [1]. Choledocholithiasis can be primary-formed primarily in the biliary ducts, as intrahepatic or extrahepatic stones, not originating from the gallbladder, however this is rare. Those CBD stones originating from the gallbladder are called secondary bile duct stones. Secondary Choledocholithiasis is more common [1-3]. Risk factors for gallstone formation are nutrition, obesity, weight loss, female sex, race and raised serum lipid levels. Primary intrahepatic stones are common in Asia and studies suggest that parasitic infestation may play a role [1,2]. A combination of bile infection, dietary factors, biliary stasis, and possibly parasitic infestation are implicated in the formation of intrahepatic biliary stones [2]. Currently the management of choledocholithiasis is ERCP, where the CBD is explored using a side viewing endoscope and visualised stones are retrieved and stent is kept in place. While these stents may remain without any complications, sometimes they may migrate or even rarely they form a nidus for stone formation. Like our patient, those from the lower socioeconomic class of society, whose understanding of disease process and treatment is poor are usual candidates for forgotten stent complication. Such patients are either unaware of having a stent in situ which needs removal or assume that their treatment is completed once they are relieved of the acute symptoms the stent was placed for. Such patients with forgotten stents commonly present with abdominal pains, obstructive jaundice and cholangitis. Forgotten stents lead to bacterial proliferation, biofilm formation and precipitation of calcium bilirubinate resulting in stone-stent complex. They usually have deranged liver function tests and dilated biliary radicles on abdominal ultrasound [1,4,5]. Biliary stents are foreign bodies and, therefore, form a nidus of infection particularly if not removed within 4–6 weeks from insertion [3,4]. The de novo formation of biliary stones around the stent was reported in a few case reports [1,4]. These may lead to a stone-stent complex assuming a lollipop, dumb-bell, or the stent shape [1,4]. The term “stentolith” is credited to Bansal, et al. who were the first to refer to stent-stone complex in 2009 [4]. The real cause of the burden of stones in the biliary tract is unknown. It is noted, however, that our case was the only one reported with a forgotten metal stent while the other case reports had plastic stents [1,4,5]. Whether this is contributory to the burden and extent of stones involvement is unknown.
Endoscopic sphincterotomy and stone extraction as a treatment modality for CBD stones clearance is successful in 80-90% of cases [5,6]. There is very little information in the literature regarding forgotten biliary stents except for a few case reports [1,4,5]. Some of these cases fail endoscopic management necessitating open surgery [1,4]. This was the case with our patient. The largest case series of five patients was reported by Odabasi et al, [5]. While endoscopic management has revolutionized biliary stones management in a big way, this management modality often fails in forgotten stents necessitating open surgery. Forgotten stents can cause serious complications of severe cholangitis, biliary sepsis and obstructive jaundice. Importance of education of patients and their relatives about the implications of noncompliance to follow-up must be emphasized.
References
- Barai V, Hedawoo J, Changole S (2017) Forgotten CBD stent (102 months) with stone-stent complex: a case report. Int J Surg Case Rep 30: 162-164.
- Ko CW, Lee SP (2002) Epidemiology and natural history of common bile duct stones and prediction of disease. Gastrointest Endosc 56: 165-169.
- Yoo KS, Lehman GA (2010) Endoscopic management of biliary ductal stones. Gastroenterol Clin North Am 39: 209-227.
- Bansal VK, Misra MC, Bhowate P, Kumar S (2009) Laparoscopic management of common bile duct “Stentolith”. Trop Gastroenterol 30: 95-96.
- Odabasi M, Arslan C, Akbulut S, Abuoglu HH, Ozkan E, et al. (2014) Long-term effects of forgotten biliary stents: a case series and literature review. Int J Clin Exp Med 7: 2045-2052.
- Manes G, Paspatis G, Aabakken L, Anderloni A, Arvani-takis M, et al. (2019) Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 51: 472-491.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...