Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Mesenteric Fibromatosis Simulating a Gastrointestinal Stromal Tumor: A Rare Cause of Intestinal Obstruction Volume 5 - Issue 1
Rasoaherinomenjanahary Fanjandrainy1, Rakotondrainibe Aurélia2, Razafindrainibe Tanjonirina3, Nomenjanahary Lalaina4, Tolotra Emmanuella Christina1, Solo Corinne5, Andriantsoa Mirana Jocya1 and Samison Luc Hervé1
- 1Digestive surgery Unit, University Hospital - Joseph Ravoahangy Andrianavalona, Madagascar
- 2Surgical Intensive Care Unit, University Hospital - Joseph Ravoahangy Andrianavalona, Madagascar
- 3Adult Intensive CareUnit, University Hospital of Gynecology Obstetrics of Befelatanana, Madagascar
- 4Anatomy Pathology Unit, University Hospital - Joseph Ravoahangy Andrianavalona, Madagascar
- 5Surgery Unit, University Hospital - Tanambao I –Antsiranana, Madagascar
Received:May 12, 2020; Published: May 22, 2020
Corresponding author: Rasoaherinomenjanahary Fanjandrainy, Digestive Surgery Unit, University Hospital - Joseph Ravoahangy Andrianavalona – Antananarivo, CHU Antananarivo 101, Madagascar
DOI: 10.32474/SCSOAJ.2020.05.000204
Abstract
Mesenteric fibromatosis also known as mesenteric desmoids is a rare benign mesenchymal lesion that can occur throughout the gastrointestinal tract, especially small bowel. Because of its biological behavior, mesenteric fibromatosis is often confused with submucosal tumor or malignant neoplasm of gastrointestinal tract, mainly gastrointestinal stromal tumors (GIST). Often asymptomatic or by incidental finding, these tumors can be revealed by signs and symptoms related to the small bowel such as abdominal pain or a palpable abdominal mass ; or by clinical complications like gastrointestinal bleeding, small bowel obstruction, fistula formation, or bowel perforation. The authors report a rare case of small bowel obstruction secondary to sporadic synchronous intra-abdominal fibromatosis in a 61-years old man who complained for a palpable mass at left lower quadrant of his abdomen and which was initially misinterpreted as a GIST on the CT. A laparotomy was planed, but the patient complained for abdominal pain with a stop of flatus and stools which required emergency hospitalization. En-bloc resection of the tumor with the adjacent jejunum was performed followed by end-to-end anastomosis. Postoperative course was unremarkable. The diagnosis was revised as mesenteric fibromatosis according to pathologic examination. Bowel obstruction is a rarely revealing complication of mesenteric fibromatosis. Clinical manifestations at a complicated stage require emergency surgery in suitable candidates. In this case, emergency tumor excision made it possible to avoid complications from intestinal obstruction and to correct the first diagnosis, which was initially a GIST.
Keywords: Anastomosis, Surgical; Benign Neoplasm; Fibromatosis, Abdominal; Intestinal Obstruction; Margins of Excision; Mesentery
Introduction
Mesenteric fibromatosis is a rare sporadic mesenchymal neoplasm of the small bowel that arises from myofibroblasts. It is a histologically benign disease and lacks the capacity to metastasis [1,2]. It can involve any site of gastrointestinal tract, but the most common site is the mesentery of the small bowel. Its biological behavior is intermediate between benign fibrous tissue proliferation and fibrosarcoma [3].They are often found incidentally but can be symptomatic or even revealed by digestive, vascular, and urological complications [4]. We report the case of a 61-year-old man, scheduled for the surgical removal of a palpable mass of the left lower quadrant of his abdomen, behaving like a GIST on CT, but who in the meantime has presented an acute bowel obstruction. Emergency laparotomy was performed. Postoperative course was uneventful. Pathologic diagnosis was mesenteric fibromatosis. Although GIST and mesenteric fibromatosis are completely different entities, their clinical, radiological and histological characteristics have many similarities which can confuse clinicians [5,6]. Through the description of this case, the important role of surgery in confirming the diagnosis and preventing complications will be emphasized.
Case presentation
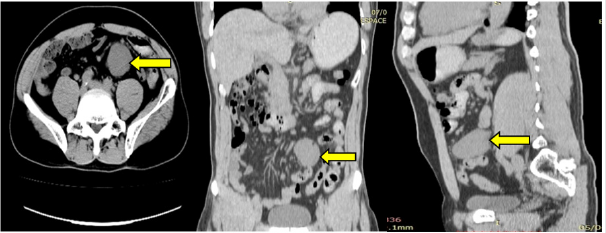
61-year-old man was admitted for constipation associated with abdominal pain in the lower quadrant evolving for a week. He had no specific family history and no previous surgical intervention. Physical examination revealed hyperactive bowel sound and palpable mass at left lower quadrant of abdomen. Initial complete blood cell counts and blood chemistry results were unremarkable. Abdominal CT scan had found a mass developing at the expense of the small intestine measuring approximately 15cm x 10cm whose morphological characteristics evoked a stromal tumor (Figure 1).
A surgical approach was planned in order to confirm the pathological diagnostic but before the scheduled date, the patient complained of diffuse abdominal pain with a stop of his bowel function. An emergency laparotomy was performed. The lesion was close to superior mesenteric vessels. Resection of the small intestine involved by the tumor was performed followed by manual end to end anastomosis (Figure 2).
Figure 2: Operative view: The small intestine adjacent to the tumor was invaded on its antimesenteric side explaining the acute intestinal obstruction.

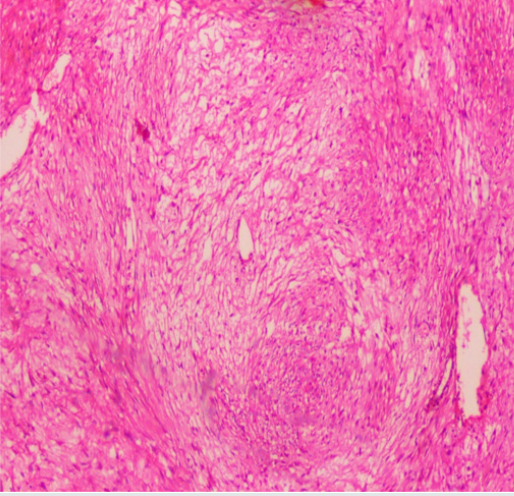
The surgical specimen consisted of an angulated segment of the small intestine, which was 35 cm long, and had a hard ovoid nodule, measuring 10 x 15cm, in the mesentery (Figure 3). Microscopic examination revealed a homogeneous proliferation of mesenchymal spindle cells arranged in bundles, with low mitotic index, no evidence of necrosis, and few hypercellular areas. There was no invasion of surgical margins. The microscopic study shows orderly arrangement of uniform fibroblasts associated with moderate amounts of collagen (Figure 4) compatible with a mesenteric fibromatosis. The postoperative course was uneventful, and the patient was allowed to go home on the seventh postoperative day. No adjuvant therapy has been performed. After 12 months of follow-up, the patient was in very good general condition with no sign of recurrence on clinical examination and on imaging.
Discussion
Mesenteric fibromatosis is a rare, benign fibrous lesion found
in the bowel mesentery or the retroperitoneum. The mesentery
of the small bowel is the most common site [3] like in this case.
But despite its benign character, mesenteric fibromatosis tend to
be invasive and to recur locally, but do not metastasize [3,7]. Their
discovery circumstances are variable. Some cases were incidental
finding [4], others have been revealed by symptoms of abdominal
discomfort or by complications requiring emergency management
[3, 5]. Mesenteric fibromatosis can occur spontaneously or after
surgical trauma and also is associated with hormonal therapy,
familiar polyposis, or Gardner’s syndrome [8,9]. In this case,
there was no particular illness or medication in the past history.
When the mesenteric fibromatosis is symptomatic, the common
signs are: abdominal pain like in this case,constipation, palpable
mass on physical examination. These tumors can also be revealed
by complications like gastrointestinal bleeding, small bowel
obstruction, fistula formation, or gastrointestinal perforation in
rare cases [7-9]. The first case of peritonitis secondary to mesenteric
fibromatosis reported in the literature was by Gorlin RJ in 1960 and
it was initially misinterpreted as a ruptured GIST [6].
Similarly, Ng Eugene PL reported a case of a man who presented
signs of peritonitis in clinical examination. Radiological features
were consistent with a GIST but in laparotomy there was a tumor
diagnosed as mesenteric fibromatosis after the microscopic
examination [5]. Mesenteric fibromatosis can also be revealed by
occlusive syndrome such as in the case reported by Ricardo PC
[10] in which the patient complained for abdominal pain, and CT
scan evidenced a heterogeneous nodular lesion in the mesentery,
involving the fourth duodenal portion and the initial jejunal segment.
Sung HJ & Coskun P [3,11] also reported a case revealed by intestinal
obstruction following chronic abdominal pain and constipation.
In the case described here, the tumor was discovered following a
CT-scan done for chronic constipation with palpable but painless
mass. The occurrence of intestinal obstruction while waiting for
scheduled surgery has precipitated emergency management.
Abdominal fibromatosis being part of desmoid tumors, Sala A. has
reported an atypical presentation of small bowel obstruction and
perforation secondary to sporadic synchronous intra-abdominal
desmoids tumor [12]. Other complications including gynecological
and renal complications were reported as possible circumstances
of findings [3,10].
Diagnosis of mesenteric fibromatosis is based on clinical
suspicion, which depends on the location or local effect of the
tumor. The role of imaging is to define the degree of its extension
to local and neurovascular structures [13,14]. But, in most cases of
mesenteric site, the diagnosis of fibromatosis can be made difficult
by the similarity of the symptomatology with the other mainly
malignant tumors of the mesentery. Their location and their imaging
behavior are often confused with GIST in CT scan [11-14]. In the
case reported here, like in more others, the mesenteric fibromatosis
was initially misinterpreted as a GIST. Physical examination
revealed palpable mass at the left lower quadrant of abdomen
and abdominal injected CT scan had found a mass developing in
the small intestine whose morphological characteristics evoked a
stromal tumor. To distinguish mesenteric fibromatosis from GIST
on CT, Zhu H [1] suggested a number of differentiating features in
favour of mesenteric fibromatosis including extra-gastrointestinal
location, ovoid or irregular contour, homogeneous enhancement,
absence of intralesional necrosis and lower degree of enhancement.
Magnetic resonance imaging of mesenteric fibromatosis
typically demonstrates low-signal intensity relative to muscle
on the T1-weighted image and variable signal intensity on the
T2-weighted image. Otherwise, GIST typically has high-signal
intensity on T2-weighted images [2]. Surgical excision is essential
and is the most effective method for resectable masses [15]. For
this patient, excision of the tumor with the small intestine and the
corresponding mesentery was performed followed by hand sown
end to end anastomosis. There by, in our case, surgery not only
allowed resection of the mesenteric mass, but also to treat intestinal
obstruction. The patient recovered well postoperatively. For several
authors, the preferred treatment of mesenteric fibromatosis is
wide local surgical excision with tumor-free margins [8,9,11]. The
discrimination between a GIST and mesenteric fibromatosis is
difficult since a biopsy cannot be performed, which make surgery
an essential step of the management. After surgery, further
treatment will depend on the histological nature of the tumor,
which will be different for GIST and mesenteric fibromatosis. If
in case of GIST, adjuvant treatment with Imatinib is mandatory
[16-18], for mesenteric fibromatosis, the need or not for adjuvant
therapy is controversial. Surgery with negative surgical margins
is sufficient for some authors [8,9] as in our case where as for
other authors, surgery only is not advised because of the risk of
recurrence. Indeed like GIST, mesenteric fibromatosis is locally
aggressive with a high recurrence rate after surgical resection [5].
Studies have shown that the local recurrence rate is 25%–50% at
five years after complete resection [10]. For cases with incomplete
resection and recurrent cases, radiotherapy may be effective,
although this is rarely used for mesenteric fibromatosis because
of the severe side effects. Khorsand J reported that radiotherapy
reduced the recurrence of mesenteric fibromatosis to 20%-40%
compared to 40%-70% reduction achieved with surgery only
[16]. In addition, chemotherapy (vincristine, cyclophosphamide,
and dactinomycineither alone or in combination), non-steroidal
anti-inflammatory drugs, hormonal manipulation (tamoxifen,
aromatase inhibitors,gonadotropin), and molecular target therapy
(imatinib, sorafenib, and sunitinib) may be alternative choices
[17]. Pathologic confirmation should be made by microscopic
examination and immunohistochemistry [2]. The absence of CD34
and S100 expression supports the fibromatous nature of the lesion
and may be helpful in discriminating mesenteric fibromatosis from GIST [19]. In our case, due to the patient’s financial problems,
immunohistochemical examination could not be performed, the
cost of this additional examination being the responsibility of the
patient in our rstudy site. Despite this absence of complementary
immunohistochemistry, the pathology examination was sufficient
to confirm the diagnosis of fibromatosis by showing an arrangement
of uniform fibroblasts associated with collagen. No adjuvant
treatment was initiated. No recurrence was observed after one year
of follow-up and the patient is still alive.
Conclusion
Distinction of mesenteric fibromatosis from GIST is clinically important, as they are different entities with a different clinical course, treatment options, and prognosis. Although, watchful waiting may be offered for asymptomatic mesenteric fibromatosis, surgical resection with microscopic examination and immunohistochemistry remains the best way to confirm the diagnosis, and to avoid complications.
References
- Zhu H, Chen H, Zhang S, Peng W (2013) Intra-abdominal fibromatosis: Differentiation from gastrointestinal stromal tumour based on biphasic contrast-enhanced CT findings. Clin Radiol 68(11):1133-1139.
- Marek W, Bogna ZW, Maciej S, Wlodzimierz C, Barbara G, et al. (2011) Mesenteric fibromatosis with intestinal involvement mimicking a gastrointestinal stromal tumour. Radiol Oncol 45(1): 59-63.
- Sung HJ, Chang NP, Ji HJ, Kang Moon L, Woo CC, et al. (2009) Simultaneous Colonic Obstruction and Hydroureteronephrosis due to Mesenteric Fibromatosis. Gut and Liver 3(3):215-217.
- Majdouline B, Mariam A, Abdesslam B (2014) Desmoid tumor of the mesentery: a rare cause of abdominal mass in women. Pan Afr Med J 17: 257.
- Ng Eugene PL, Kwok SY, Lok KF, Chow MP, Lau PY (2018) Mesenteric fibromatosis: a rare cause of peritonitis. Hong Kong Med J 24(1): 84-86.
- Gorlin RJ, Chaudhry AP (1960) Multiple osteomatosis, fibromas, lipomas and fibrosarcomas of the skin and mesentery, epidermoid inclusion cysts of the skin, leiomyomas and multiple intestinal polyposis: a heritable disorder of connective tissue. N Engl J Med 263: 1151-1158.
- Rampone B, Pedrazzani C, Marrelli D, Pinto E, Roviello F (2007) Update on abdominal desmoids tumors. World J Gastroenterol 13: 5985-5988.
- Burke AP, Sobin LH, Shekitka KM, Federspiel BH, Helwig EB (1990) Intra-abdominal fibromatosis: a pathologic analysis of 130 tumors with comparison of clinical subgroups. Am J Surg Pathol 14(4): 335-341.
- Rodriguez JA, Guarda LA, Rosai J (2004) Mesenteric fibromatosis with involvement of the gastrointestinal tract. A GIST simulator: a study of 25 cases. Am J Clin Pathol1 21: 93-98.
- Ricardo PC, Enilde EG, Eduardo C, Karla L (2016) Mesenteric fibromatosis affecting duodenum and jejunum. Int J Colorectal Dis. mars 31(3): 715.
- Coskun P, Fatma A, Serkan T, Burc Y, Taner O, et al. (2010) A giant mesenteric fibromatosis case presenting with mechanical intestinal obstruction and successfully resected with partial duodeno-jejunectomy and right hemicolectomy. Clinics 65(1):110-113.
- SalaA, MichelleW, Mark, Aleksandras U (2016) An atypical presentation of small bowel obstruction and perforation secondary to sporadic synchronous intra-abdominal desmoid tumours. Int J Surg Case Rep 20: 147-150.
- Einstein DM, Tagliabue JR, Desai RK (1991) Abdominal desmoids: CT findings in 25 patients. AJR Am J Roentgenol 157(2): 275-279.
- Quinn SF, Erickson SJ, Dee PM, Walling A, Hackbarth DA, et al. (1991) MR imaging in fibromatosis: results in 26 patients with pathologic correlation. AJR Am J Roentgenol 156(3): 539-542.
- Peng W, Haitao Z, Zhixiang Z, Jianwei L(2018) Mesenteric fibromatosis misdiagnosed with lymph node metastasis after successful laparoscopic right hemicolectomy: a report of two cases with review of literature. OncoTargets and Therapy 11: 4811-4816.
- Khorsand J, Karakousis CP (1985) Desmoid tumors and their management. Ann J Surg 149(2): 215–218.
- Chaudhary P (2014) Mesenteric fibromatosis. Int j Colorectal Dis 29(12): 1445-145118.
- Colombo P, Rahal D, Grizzi F, Quagliuolo V, Roncalli M (2005) Localized intra-abdominal fibromatosis of the small bowel mimicking a gastrointestinal stromal tumor: a case report. World J Gastroenterol. september 11(33): 5226-5228.
- Monihan JM, Carr NJ, Sobin LH (1994) CD34 Immunoexpression in stromal tumours of the gastrointestinal tract and in mesenteric fibromatoses. Histopathology 25(5): 469-473.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...