Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Lumbar Fracture : is it Better to Operate with Minimally Invasive Surgery or Conventional (Open) Surgery? Volume 2 - Issue 4
Inaki Arrotegui*
- Department of Neurosurgery, Spain
Received: March 29, 2019; Published: April 10, 2019
Corresponding author: Inaki Arrotegui, Department of Neurosurgery, Spain
DOI: 10.32474/SCSOAJ.2019.02.000145
Introduction
Spinal traumatisms are defined as the damage to the osteoligamentous elements of the spine with or without involvement of the spinal cord and / or roots of the spinal nerves secondary to trauma.
Anatomical memory of the spine
The spine is a bone structure composed of numerous bones, which are the vertebrae, joined by ligamentous elements and other elastic tissues (such as the intervertebral disc) and muscular. The main functions of the spine are: stability and mobility for the movements of the trunk and extremities and provide protection to different nerve structures [1]. The vertebral column is divided into three parts: cervical, formed by seven vertebrae (C1-C7), thoracic, with twelve vertebrae (T1-T12), lumbar, with five vertebrae (L1- L5), sacrum, with five vertebrae fused together to form a single bone (S1-S5) and the coccyx [2]. Likewise, the spine forms a series of characteristic curves: two ventral convex (cervical and lumbar lordosis) and two dorsal convexes (thoracic and sacral kyphosis) [3]. Finally, the ligamentous and muscular structures give it the necessary stability to support the weight of the trunk and allow different movements.
Epidemiology
Spinal cord injuries have an incidence of 30 cases / year per million inhabitants. The most frequent age range is 25 to 35 years, highlighting the male sex. The most frequent etiology is the traffic accident. One The region of the column most frequently affected is the cervical spine, followed by the cervicothoracic junction (C6-T1) and subsequently by the thoracolumbar junction (T11-L2) .
Clinical features
The most frequent and important clinical feature in spinal cord injuries is spinal pain that may or may not be focused in the segment that presents the osteoligamentous lesion. There may also be a subjective or objective involvement of the central nervous system (marrow) or peripheral (nerve roots). In general, with didactic effects, the clinic of spinal osteoligamentous lesions are divided into [4]:
a. Patients with neurological involvement
b. Patients without neurological involvement
Neurological involvement is not important for the classification, for the prognosis and for planning the treatment of spinal cord injuries. Within the neurological involvement of spinal fractures we can find almost any possible syndrome within the medullar and radicular pathology (complete spinal cord shock, medullary syndrome, lateral syndrome, anterior syndrome, posterior cord syndrome, radicular syndrome, etc.) [5].
Treatment
In the medical-surgical literature there have been hundreds of treatment modalities for this type of fracture. Basically they can be classified into two types: conservative treatment (with orthosis and rest) and surgical treatment. Within the surgical treatment in the history of orthopedic surgery there have been multiple techniques. At the present time, we can classify the different techniques into two groups: open surgery and minimally invasive surgery [6]. In recent years, open or minimally invasive techniques have been diversified thanks to the evolution of instrumented fixation systems, which has been very profuse.
Clinical Case
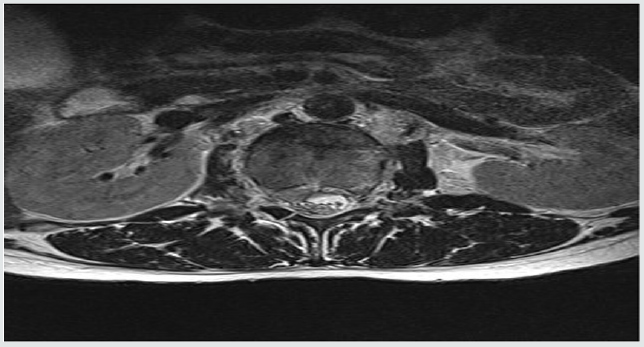
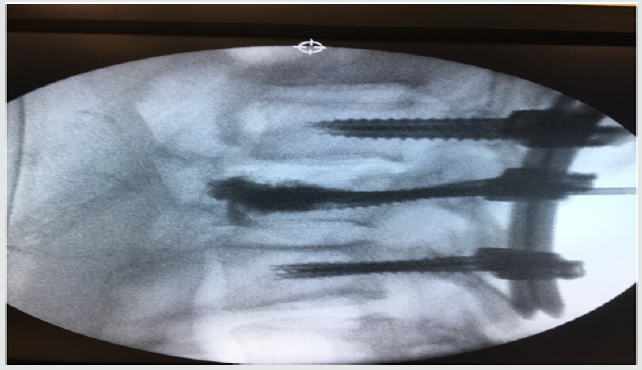
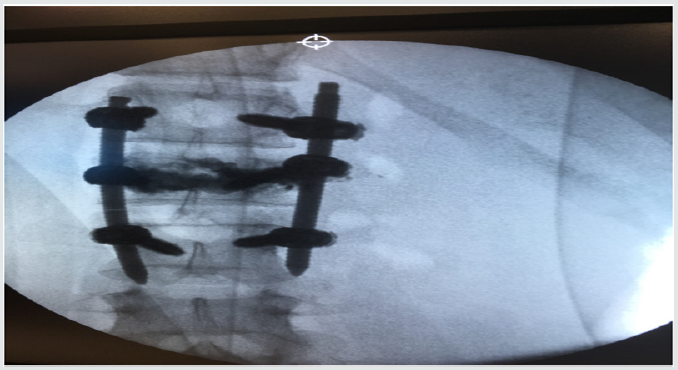
Patient who suffers a lumbar fracture secondary to precipitation due to autolysis: (Figures 1 & 2) show the lesion with displacement of the posterior wall < to 25%. The patient did not present neurological focality. After starting with the mandatory analgesic treatment, it was decided to perform an arthrodesis with vertebroplasty of the fractured vertebra, by means of minimally invasive surgery. In Figures 3 & 4 the alignment of the column is observed with recovery of the physiological lordosis at lumbar level.
Discussion
Historically, the question of what is the appropriate treatment for a thoracolumbar fracture has existed. This problem has been a constant in all articles related to the subject in world literature. Therefore, in this work, the main approach is: In the event that a thoracolumbar fracture must be operated, is it better to operate with minimally invasive surgery or conventional (open) surgery? Grossbach et al. [7], who did not find statistically significant differences between the group treated with MIS and the one treated with open surgery for the variables studied with respect to the kyphotic angle and ASIA (American Spinal Injury Association) [8]. Wild et al. [9] found a considerable decrease in intraoperative blood loss in patients treated with percutaneous fixation, like Lee et al. [10]. Vanek et al. [11] agrees with the results obtained previously, in addition to affirming a decrease in postoperative pain in MIS surgery. One of the variables under study was the operating time. They showed that this is dependent on the number of screws to be implanted (four screws carry a duration of 106 minutes, six screws, 144 minutes and eight screws, an average of 171 minutes).
Second : Postoperative recovery time, concluded that this was dependent on the patient’s condition. Non-polytraumatized patients regained the ability to get up on the 2nd postoperative day and were discharged on the 5th day.
Third : Back pain was assessed using the visual analog scale (VAS). The result obtained was considerably satisfactory, since most of the patients perceived little pain on the second postoperative day.
Fourth : Significant differences were found in the length of hospital stay. The patients treated conservatively were admitted for an average of 36 days while those treated with surgery were admitted for 2 (MIS) and 4 days (open surgery).
The next variable to treat was the return of his working life, The patients treated with surgery were the following: 4 did not return to their occupations in those treated with open surgery, while in those treated with MIS all returned to their original occupations. Finally, a lower blood loss (80 ml) was found for the group treated with MIS, as opposed to the data obtained from patients treated with conventional surgery (550 ml ) According to the different studies analyzed for this review, there are no statistically significant differences between MIS and open surgery in terms of radiological variables (such as the height of the vertebral body, the degree of kyphosis and the angle of Cobb). However, differences have been found between the clinical variables (such as return to work, hospital stay and postoperative pain) and the variables measured intraoperatively (surgery time and intraoperative blood loss), with better results seen in the patients treated. with minimally invasive surgery.
Conclusion
In relation to the best surgical technique (MIS or open surgery) with respect to the radiological variables (degree of kyphosis, vertebral body height and Cobb angle), since in both of them similar results are obtained in terms of restoration the anatomy of the column. However, better results have been obtained by comparing the clinical variables, such as the reduction of surgical time with respect to minimally invasive surgery, in addition to a lower blood loss and a reduction in the length of hospital stay, which may imply advantage for patients, especially polytraumatized patients. There has also been a reduction in the time it takes patients to return to their work and social life, As a final conclusion it could be concluded that the choice of technique to be used is related to: knowledge of the surgeon in each of the techniques and the type of fracture of the patient.
References
- Dhall SS, Wadhwa R, Wang MY, Tien Smith A, Mummaneni PV (2014) Traumatic thoracolumbar spinal injury: an algorithm for minimally invasive surgical management. Neurosurg Focus 37(1): E9.
- Court C, Vincent C (2012) Percutaneous fixation of thoracolumbar fractures: current concepts. Orthop Traumatol Surg Res 98(8): 900-909.
- De Iure F, Cappuccio, Paderni S, Bosco G, Amendola L (2012) Minimal Invasive Percutaneous Fixation of Thoracic and Lumbar Spine Fractures. Hindawi Publishing Corporation 1:1-6.
- Kumar A, Aujla R, Lee C (2015) The management of thoracolumbar burst fractures: a prospective study between conservative management, traditional open spinal surgery and minimally interventional spinal surgery. SpringerPlus 4(204): 1-10.
- McAnany Sj, Overley SC, Kim JS, Baird EO, Qureshi SA, et al. (2016) Open Versus Minimally Invasive Fixation Techniques for Thoracolumbar Trauma: A Meta-Analysis. Global Spine J 6(2): 186-194.
- Li K, Li Z, Ren X, Xu H, Zhang W, et al. (2016) Effect of the percutaneous pedicle screw fixation at the fractured vertebra on the treatment of thoracolumbar fractures. International Orthopaedics (SICOT) 40(6): 1103-1110.
- Grossbach AJ, Dahdaleh NS, Abel TJ, Woods GD, Dlouhy BJ, et al. (2013) Flexion-distraction injuries of the thoracolumbar spine: open fusion versus percutaneous pedicle screw fixation. Neurosurg Focus 35(2): E2.
- Maynard (1997) International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. Spinal Cord 35(5): 266-274.
- Wild MH, Glees M, Plieschnegger C, Wenda K (2007) Five-year followup examination after purely minimally invasive posterior stabilization of thoracolumbar fractures: a comparison of minimally invasive percutaneously and conventionally open treated patients. Arch Orthop Trauma Surg 127(5): 335-343.
- Lee JK, Jang JW, Kim TW, Kim TS, Kim SH, et al. (2013) Percutaneous short-segment pedicle screw placement without fusion in the treatment of thoracolumbar burst fractures: is it effective? Comparative study with open short-segment pedicle screw fixation with posterolateral fusion. Acta Neurochir (Wien) 155(12): 2305-2312.
- Vanek P, Bradac O, Konopkova R, de Lacy P, Lacman J, et al. (2014) Treatment of thoracolumbar trauma by short-segment percutaneous transpedicular screw instrumentation: prospective comparative study with a minimum 2-year follow-up. J Neurosurg Spine 20(2): 150-156.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...