Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Research Article(ISSN: 2643-6760) 
Laser Transcanalicular Dacryocystorhinostomy Comparative Study between ENT and Ophthalmology Group Volume 3 - Issue 4
Pedro Clarós1*, Cristina María Blebea1,2, Marta López-Fortuny3, Gorka Martinez-Grau3 and Andrés Clarós1
- 1Department of Otolaryngology, Clarós Clinic, Spain
- 2Scholarship in Clarós Clinic, Spain
- 3Department of Oculoplasty, Barraquer Clinic, Spain
Received: October 30, 2019; Published: November 19, 2019
Corresponding author: Pedro Clarós, Department of Otolaryngology, Clarós Clinic, Barcelona, Spain
DOI: 10.32474/SCSOAJ.2019.03.000170
Abstract
Background: Obstruction of the nasolacrimal system is a pathology that involves an ophthalmologist and also an otorhinolaryngologist. Epiphora, or watery eye, represents an overflow of tears onto the face and it can produce a great impact on the quality of life of the patient.
Aims/Objectives: The purpose was to analyse the results of transcanalicular diode laser-assisted dacryocystorhinostomy of patients treated in Barraquer Ophthalmology Center Oculoplasty Department, and in Clarós Clinic ENT Department, Barcelona, Spain, and to determine whether there is an association between the surgeon’s speciality and the outcome of the intervention.
Materials and Methods: A comparative, retrospective, non-randomized, non-interventional case review of 409 patients with nasolacrimal duct obstruction treated in these two clinics between 2004 and 2016.
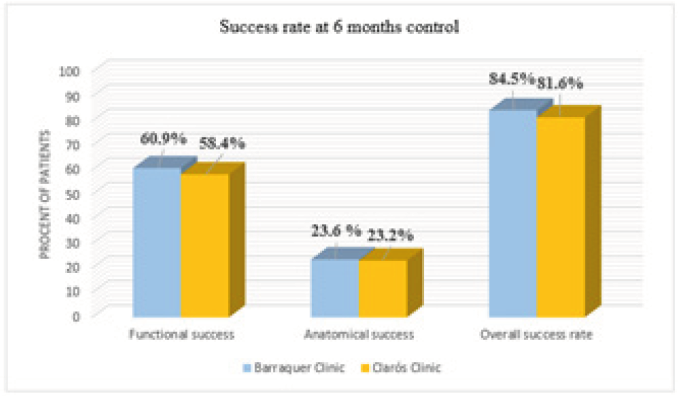
Results: Female patients were most affected by this pathology and the main cause of it was the idiopathic stenosis of the nasolacrimal duct. The functional success rates were similar between the two groups, and the overall success of the intervention at 6 months follow-up presented no statistically significant difference. Also, having no surgical antecedents was statistically significant associated with a better outcome on the 6 months control (x2; p > 0,035).
Conclusion and Significance: Implementation of diode laser-assisted dacryocystorhinostomy for nasolacrimal duct obstruction can be a reliable method, with good aesthetic results, shorter time of procedure, and good functional outcome. A combined surgical team would be beneficial for a faster recognition of anatomical elements, management of the complications and to improve surgical time.
Keywords: Dacryocystorhinostomy; transcanalicular; epiphora; diode; laser; ent; ophthalmology
Pedro Claróshttps://orcid.org/0000-0002-7567-0370
Cristina Blebeahttps://orcid.org/0000-0003-2230-3435
Andrés Claróshttps://orcid.org/0000-0001-6084-3470
Introduction
Obstruction of the nasolacrimal system is a frequent pathology that involves an ophthalmologist and also an otorhinolaryngologist. Tearing can be a predisposing factor for infections of the lacrimal system [1] and can also produce a great impact on the quality of life of the patient. Epiphora can be the consequence of a lacrimal overproduction caused by alteration of the ocular surface, in which the treatment tends to be medical, or can be caused by lacrimal drainage deficiency by means of obstruction or anatomical anomalies of the lacrimal system [2]. Lacrimal pathway obstruction can be congenital or acquired and can affect different segments of it. This way we can classify the causes as: congenital, idiopathic stenosis, or secondary to trauma, skin burns, inflammatory systemic disease, infections, neoplasia infiltration, and drugs for glaucoma, chemotherapeutic or functional epiphora [3]. Idiopathic obstruction of the nasolacrimal duct is more frequent in women (50% - 83% of the cases). Shigeta [4] determined the diameters of the bony nasolacrimal canal and evaluated how they are affected by sex and age and concluded that the bony structure of the nasolacrimal canal in females has a significantly smaller anteroposterior and transverse diameters, also the acute angle between the bony canal and the nasal floor, both considered predisposing factors to chronic inflammation of the nasolacrimal drainage system. Surgical intervention by dacryocystorhinostomy (DCR) is the mainstay treatment for epiphora resulting from nasolacrimal duct obstruction, and its objective is to create a new communication between the lacrimal sac and the nasal cavity that facilitates the lacrimal drainage. In 1904 Addeo Toti described dacryocystotomy through the medial can thus, what is considered the first modern description of external DCR [5], which remains the election procedure for many ophthalmologists, with success rates of 90% to 95% [6]. In 1910 West, and then Polyak in 1913, published a procedure for intranasal opening of the lacrimal sac [7]. Performing this procedure endoscopically, provides better cosmetics with excellent outcomes [1] and is the method preferred by most otorhinolaryngologists. In 1990 was published the first cadaveric study in which an osteotomy was achieved by means of laser energy delivered through an optic fibre [8] and in 1992, Christenburry [9] described the first transcanalicular approach for DCR. This minimally invasive technique represents an option to the ‘gold standard’ external surgical approach though it has a relatively lower success rate [10]. The benefits of this technique in comparison with the external approach are: no skin scarring on the face, less surgical manipulation of the medial canthal tissues and lacrimal pump, faster recovery time, minimal or no postoperative ecchymosis and oedema and minimal bleeding, which recommends this technique for patients under treatment with anticoagulants or other bleeding disorders [9]. The objective of this article is to evaluate and to compare the success rate of transcanalicular diode laser-assisted dacrycystorhinostomy (TCL-DCR) followed by 2 months of bicanalicular silicone tube for nasolacrimal duct obstruction of 409 patients treated in Barraquer Clinic and Clarós Clinic, Barcelona, Spain, and to determine whether there is an association between the surgeon’s speciality and the outcome of the intervention.
Materials and Methods
We conducted a comparative, retrospective study, nonrandomized; non-interventional that included 409 consecutive patients that underwent diode laser transcanalicular dacryocystorhinostomy. Two hundred eighty-four patients were operated in the Department of Oculoplasty of Barraquer Ophthalmology Center, and 125 patients in the ENT Department of Clarós Clinic, Barcelona, Spain, since October 2004 until November 2016, by the same ophthalmologist specialised in oculoplastic surgery and by the same otorhinolaryngologist, respectively. Informed consent was obtained from every patient before surgery, after they were explained the surgical procedure, risks and benefits on evidence-based medicine results. The information required to conduct this study was collected from patient database and introduced in an Excel database. The diagnostic of nasolacrimal duct obstruction was established based on symptoms, preoperative irrigation of the lacrimal pathways performed following topical anaesthesia and imaging (contrast dacryocystography) whenever deemed necessary to determine the exact level of obstruction. Regardless of the medical centre where the surgical procedure was performed, patients had a complete ophthalmic examination including slit-lamp examination to rule out other causes of watery eyes: blepharitis, conjunctivitis, conjunctivochalasis, entropion, ectropion, lagophthalmos, keratitis, trichiasis and also a rhinologic evaluation was performed to assess any concomitant nasal pathology, such as septum deviation, concha bullosa, chronic sinusitis or nasal polyposis. We established as inclusion criteria: congenital nasolacrimal duct stenosis, acquired nasolacrimal duct stenosis.
Also, the exclusion criteria were established as follow: acute dacryocystitis, mucocele, and common canalicular obstruction, previous trauma with disfigurement, nasal polyps, nasal cavity neoplasia and important nasal septum deviation. The surgical procedure was performed under local anaesthesia and intravenous sedation and in some selected cases, under general anaesthesia. Ten minutes before the intervention, we anaesthetized the nasal mucosa of the lateral nasal wall by packing with gauze soaked with vasoconstrictor solution in order to limit the bleeding. We dilated both lacrimal punctae with the purpose to facilitate the placement of the laser fibre. The laser fibre we used to have a 600 microns diameter, 980 nm wavelength and 10 W power (FOX by ARC Laser GmbH). The middle nasal meatus was inspected with a rigid 00 nasal endoscope (Storz, Tübingen, Germany), while the diode laser fibre was inserted through a canalicular probe. Transillumination of the lateral nasal wall from the side of the saccus, while inspecting the middle nasal meatus allowed us to determine the exact site of osteotomy, just anterior and inferior to the attachment of the middle concha. The laser beam was properly focused and was used to create the osteotomy. The size of osteotomy was controlled through the nasal endoscope and was around 5 mm diameter or more. In order to prevent excessive fibrosis and minimise mucosal scars, we applied a swab with 0, 01% Mitomicin C solution, for 1 minute. Mitomicin C is an antineoplastic agent that markedly prevents fibroblastic proliferation. Next step of the procedure consisted of lacrimal canal intubation with a bicanalicular silicone tube (FCI BIKA® bicanalicular intubation 0.64 mm silicone tube). Both ends of the tube were tied together and left free in the nasal cavity.
There was no postoperative nasal packing and all patients were discharged the same day having an uneventful recovery. Systemic antibiotics were administrated in a single dose, perioperative. We explained to our patients that the silicone tubs are intended to remain in place for 2 months. Functional success was defined as the absence of epiphora as indicated by the patient. Anatomical success was defined as patency of the neo-ostium with irrigation. The surgical procedure was performed by the same surgeon in each centre. Postoperative treatment included: antibiotic and corticoid eye drops and nasal spray corticoids and was recommended for 10 days. Follow-up examinations were planned at 1 week, 4-6 weeks, 3-4 months and 6 months. During each visit we documented the patient’s symptoms, performed a control irrigation to assess the patency of the new lacrimal pathway and nasal endoscopy. We performed more investigations if epiphora was present, no matter the gravity considering Munk scale. (measures the grade of the epiphora) The statistical analysis of data was performed using the soft Statistical Package for the Social Sciences 10.0 (SPSS Inc., Chicago, IL, USA).
Results
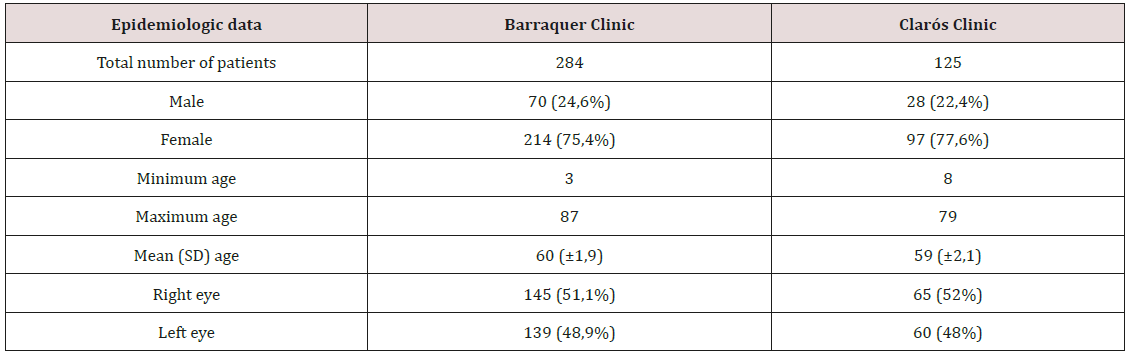
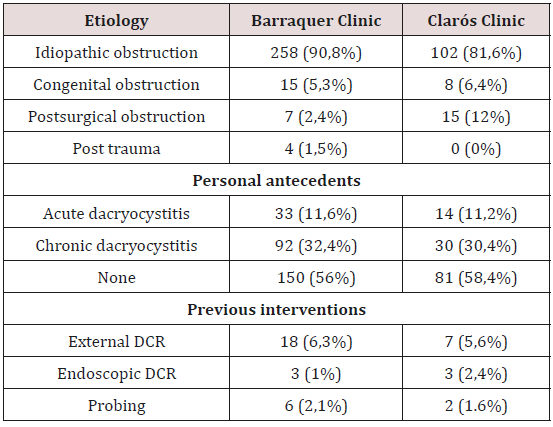
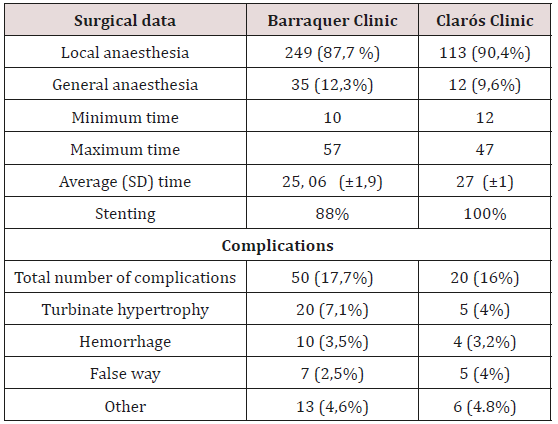
Of 409 patients included in this study, 284 of them were treated in Barraquer Ophthalmology Centre, and 125 patients in Clarós Clinic. There was no difference in distribution of the sex, age and predominance of the affected eye (Table 1). Based on the anamnesis, clinical examination and imaging investigations (dacryocystography), both groups presented epiphora as main complain and the foremost cause of this symptom was established to be idiopathic primary obstruction of the lacrimal pathway followed by congenital obstruction. Both specialities encountered cases of obstruction due to previous surgery, probing or facial trauma. During the clinical history, half of the patients recall that before attending the consult, they had suffered either multiple episodes of conjunctivitis, chronic dacryocystitis or one or more episodes of acute dacryocystitis during their life (Tables 2 & 3). Both departments preferred to realise this procedure in local anaesthesia, and just in selected cases, general anaesthesia with sedation was used. The average procedure time was 25 respectively 27 minutes with a range of values between 10 to 57 minutes. Bicanalicular silicone tubes were used by both surgeons, 250 (88%) patients in the Ophthalmologic Center and in 100% of the patients treated in the Clarós Clinic. Among the complications encountered during surgery the most frequent were nasal haemorrhage, or false way. The inferior conchae hypertrophy difficult and disturbs the vision during the surgical procedure especially for the ophthalmologist. We examined our patients 24 hours after surgery, and planned our follow-up at one week, 4-6 weeks, 3-4 months and 6 months, and established the rate of functional success, defined as no presence of epiphora. Irrigation was performed in all patients who noted an improvement after surgery but not full resolution of epiphora, and this way we could establish the anatomical success rate. The results of the follow-up are resumed in Figure 1.
Discussion
Lacrimal pathway obstruction is more frequent in women, representing 50-83% of the cases [4] and the main cause is considered to be idiopathic [11]. Both clinics experienced the pathology to be more frequent in female patients, 75,4% vs 77,6% and the most invoked cause was primary idiopathic stenosis of the nasolacrimal duct. Between 10% to 20% of the patients with DCR presented episodes of acute dacryocystitis with an average of 2,4 episodes-person [12]. Our study groups had similar values, 11,6% of the patients treated in Barraquer Clinic presented acute dacryocystitis in their medical background and 10% of those treated by otorhinolaryngologist. External DCR is considered the gold standard surgery for primary acquired nasal duct obstruction. The data regarding this affirmation may be controversial. Uludag et al. [13]. conducted a study on 19 patients with bilateral duct obstruction who underwent EX-DCR on one eye and TC-DCR on the other eye with bicanalicular silicon tube placement. At the 3 months follow-up, the anatomical success rates were 84.2% and 89.4% in the TC-DCR and EX-DCR groups, respectively, but the difference was not statistically significant.
In the study conducted by Balikoglu-Yilmaz M [14] comparing dacryocystorhinostomy surgeries by external versus endoscopic versus transcanalicular diode laser approach, were found similar success rate with no significant differences between the groups regarding anatomical (81.8%, 75.9%, and 76.7% in EX-, EN-, and TC-DCR groups, respectively; p = 0.824) and functional success rates (81.8%, 72.4%, and 73.3% in EX-, EN-, and TC-DCR groups, respectively; p = 0.626). Therefore, transcanalicular diode laserassisted dacryocystorhinostomy is a daycare procedure that has a shorter procedure time, a more rapid recovery, decreased complication rate, no surgical skin scars, and can be done under local anaesthesia. Both surgeons obtained similar mean time of surgery values (25, 06 min vs 27 min), that are in the range of what other surgeons have reported [1,15,16]. It is important to mention that the ENT surgeon found it more difficult to access the lacrimal punctae (most of the time he did not use magnifying spectacle) and the ophthalmologist required a greater amount of time to manoeuver the endoscope and to rapidly identify the nasal cavity anatomic elements and its modifications, especially the twisted nasal septum or hypertrophic turbinates or allergic rhinitis. In our study, the rate of surgical complications was under 20%, a percentage that corresponds with the data sustaining the efficacy of the laser assisted transcanalicular DCR approach [17].
The odds of post-operative bleeding were not significantly different between the two groups, but the otorhinolaryngologist found it easier to control an epistaxis or to handle demanding anatomical situations (e.g. conchae hypertrophy, septal spurs). We mention that accidental false way had a greater rate of incidence in the ENT group. At 24h after surgery, more than 97% of patients of each group presented an improvement of the symptomatology, but in order to evaluate the success of the intervention, we need to follow-up our patients up to 6 months, when it is considered that the local inflammation process has concluded. It is normal to detect a downward trend of the level of satisfaction of the patients in the following months after surgery, considering the local inflammation that can reduce or obstruct the neo-ostium. This course tends to stop and stabilise around 6 months after surgery. At this point we could observe that there was no significant difference between the results obtained in the group treated by an ENT surgeon or by the ophthalmologist. The functional success (60,8% vs 58,4% in Barraquer vs Clarós), and the anatomical success (23,6% vs 23,2% in Barraquer vs Clarós) presented no statistically significant difference. Therefore, we consider a surgical success rate of 84,5%, in the group treated in the Ophthalmology Centre and 81,6% in the ENT treated group. We need to mention that patients have a tendency of not attending the late follow-ups, because of various personal reasons or either the pathology has a favourable course. We suppose that this was the reason that during the 3 months follow-up, the Barraquer group registered a lower functional success rate by almost 6% compared to the 6 months control.
The number of patients having no epiphora were 155 (55,2%) and 24,9% (70) of the patients registered an anatomical success rate, but during this control was the highest absenteeism rate: 15,3% (43) patients did not attend the consult. The study conducted by Woog JJ [17] in 2001 reported a success rate of 63-71%, in 2004 Alañón follows a series of 43 patients up to 20 months after surgery and reports a success rate of 90,7% [9]. In 2005 Hong J et al. [18] reports a success rate of 81,5%, in 2007 Plaza et al. [9] obtains 88% of asymptomatic patients after surgery and 83,3% are reported by Drnovsek-Olup B et al. [8] in 2010. More recent studies, like the one presented by Kaynak P et al. [19] in 2014, obtained a functional success rate of 67.7% at 6 months and an anatomical success of 93.1%, and the retrospective study carried out by Mor JM et al. [20] in 2018, using the same surgical method but with a 810 nm wavelength diode laser, reported a surgical success rate of 97% and a functional success rate of 77% at 6 months from the intervention. In our study, more women than men presented a patent lacrimal pathway at the 6-month control as well as less surgical complications. From our study we came to the conclusion that, patients who conserved the bicanalicular stent up to 60 days had a greater percentage of ostium patency. Patients with no surgical antecedents were associated with a better outcome regardless of the surgeon who realized the intervention.
Conclusion
Laser transcanalicular dacryocystorhinostomy is a viable surgical alternative for patients suffering from nasolacrimal obstruction, being minimally invasive. Although external DCR is considered the gold standard surgery for primary acquired nasal duct obstruction, recent comparative studies between diode laser transcanalicular, external and endoscopic dacryocystorhinostomy, with bicanalicular silicon tube placement, found similar success rates. Laser assisted approach comes to avert the need of some patients for having a no scar intervention, quick recovery and also address patients who cannot interrupt drugs that alter coagulation or have contraindications for general anaesthesia. Patient selection criteria and preoperative medical evaluation are important factors when considering the possibility of an office-based procedure in order to obtain a great outcome. How we have showed, the incidence of this type of pathology in the Ophthalmologic Department was nearly double than the ENT group. It is of utmost importance that both specialities collaborate in order to bridge the gap regarding this pathology and this way to obtain the best clinical outcome. It is recommended a combined surgical team approach with ophthalmologist, or training periods for the possibility to exchange ideas, surgical techniques and most important, key points in controlling possible surgical complications. Collaboration of both teams occurs when the case is difficult enough with this association, we can cover all the cases.
Disclosure of Interest
All authors declare no conflict of interest.
References
- Eichhorn K, Harrison AR (2010) External vs. Endonasal dacryocystorhinostomy: six of one, a half dozen of the other? Curr Opin Ophthalmol 21(5): 396-403.
- Ali MJ (2018) Principles and Practice of Lacrimal Surgery. (2nd edn), Singapore, Springer pp. 173-178.
- Kanski JJ (2009) Oftalmología clí (2nd edn). Barcelona, Spain, pp. 150-157.
- Shigeta K, Takegoshi H, Kikuchi S (2007) Sex and age differences in the bony nasolacrimal canal. Arch Ophtalmol 125(12): 1677-1681.
- Chandler P A (1936) Dacryocystorhinostomy. Trans Am Ophthalmol Soc 34: 240-263.
- Ayala Barroso E, Mendel Jiménez R, González Candial M (2006) Dacriocistorrinostomía: externa, endonasal o endocanalicular? Arch Soc Canar Oftal 17: 35-42.
- West J M (1910) A Window Resection of the Nasal Duct in Cases of Stenosis. Trans Am Ophthalmol Soc 12(2): 654-658.
- Drnovsek-Olup B, Beltram M (2010) Transcanalicular diode laser-assisted dacryocystorhinostomy. Indian J Ophthalmol 58(3): 213-217.
- Plaza G, Beteré F (2005) Effectiveness of transcanalicular dacryocystorhinostomy in treatment of epiphora in elder patients. Mapfre Medicina 16(2): 140-146.
- Moore W, Bentley CR, Olver JM (2002) Functional and Anatomic Results after Two Types of Endoscopic Endonasal Dacryocystorhinostomy: Surgical and holmium laser. Ophthalmol 109(8): 1575-1582.
- Holds JB (2012) Curso de ciencias básicas y clí Barcelona: Elsevier; Seccion 7, Orbita, párpados, y aparato lagrimal pp. 287.
- Toledano Fernández N (2001) Manejo actual de las obstrucciones del conducto nasolagrimal. In: Comunicación Solicitada 77 Congreso de la Sociedad Española de Oftalmologí Sociedad Española de Oftalmología, Barcelona, Spain, p. 71-83.
- Uludag G, Yeniad B, Ceylan E, Yildiz-Tas A, Kozer-Bilgin L (2015) Outcome comparison between transcanalicular and external dacryocystorhinostomy. Int J Ophthalmol 8(2): 353-357.
- Balikoglu-Yilmaz M, Yilmaz T, Taskin U, Taskapili M, Akcay M, et al. (2015) Prospective comparison of 3 dacryocystorhinostomy surgeries: external versus endoscopic versus transcanalicular multidiode laser. Ophthalmic Plast Reconstr Surg 31(1): 13-18.
- Lee DW, Chai CH, Loon SC (2010) Primary external dacryocystorhinostomy versus primary endonasal dacryocystorhinostomy: a review. Clin Exp Ophthalmol 38(4): 418-426.
- Wali U, Sabt B, Al Badaai Y, Al-Mujaini A (2018) Transcanalicular laser-assisted dacryocystorhinostomy: First report from Oman. Indian J Ophthalmol 66(1): 170-172.
- Woog JJ, Kennedy RH, Custer PL, Kaltreider SA, Meyer DR (2001) Endonasal dacryocystorhinostomy: a report by the American Academy of Ophthalmology. Ophthalmology 108(12): 2369-2377.
- Hong JE, Hatton MP, Leib ML Fay AM (2005) Endocanalicular laser dacryocystorhinostomy analysis of 118 consecutive surgeries. Ophthalmol 112(9): 1629-1633.
- Kaynak P, Ozturker C, Yazgan S, Karabulut GO, Akar S (2014) Transcanalicular diode laser assisted dacryocystorhinostomy in primary acquired nasolacrimal duct obstruction: 2-year follow up. Ophthalmic Plast Reconstr Surg 30(1): 28-33.
- Mor JM, Matthaei M, Schrumpf H, Koch KR, Bölke E (2018) Transcanalicular laser dacryocystorhinostomy for acquired nasolacrimal duct obstruction: an audit of 104 patients. Eur J Med Res 23(1): 58.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...