
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Jejunal Metastasis from Clear Cell Renal Cell Carcinoma Volume 3 - Issue 5
Juan Pablo Montemayor-Lozano1, Karla Ivonne Chávez-Blanco1, Rodolfo Morales-Avalos2, Matías Salinas-Chapa2 and Guillermo Elizondo-Riojas1
- 1Department of Radiology, University Hospital “Dr. José Eleuterio González”, Universidad Autónoma de Nuevo León, (UANL), México
- 2Department of Orthopedics and Traumatology, University Hospital “Dr. José Eleuterio González”, Universidad Autónoma de Nuevo León, (UANL), México
Received: November 29, 2019; Published: December 05, 2019
Corresponding author: Juan Pablo Montemayor-Lozano, Department of Radiology, Faculty of Medicine and University Hospital, Universidad Autónoma de Nuevo León, Ave. Madero y Dr. Eduardo Aguirre Pequeño, s/n Col. Mitras Centro, C.P.64460, Monterrey, Nuevo León, México
DOI: 10.32474/SCSOAJ.2019.03.000174
Abstract
Introduction: To present a case of a jejunal metastasis from a clear cell renal cell carcinoma (RCC) in an old-aged woman, with a history of radical left nephrectomy 20 years before the actual diagnosis.
Case report: 78 years old female presented to the emergency department, with a 7-day history of melena, diffuse abdominal complains and hyporexia. The only relevant history was a left radical nephrectomy because a RCC, which was treated only with surgery. After the medical evaluation and a normal upper gastrointestinal endoscopy an abdominal angiotomography was requested, demonstrating a bowel intussusception at the jejunum caused by an hypervascular mass, suspecting a metastasis from the RCC. The patient undergone a small bowel resection of the affected jejunum, with primary anastomosis, the histologic diagnosis of jejunal metastasis of clear cell RCC was made. After that the patient went on chemotherapy, finishing all the cycles without major complications. Actually the patient is on oncologic surveillance and refers clinically asymptomatic.
Conclusión: RCC accounts for 3% of the total of adult malignancies, the most common subtype is the clear cell carcinoma. The prevalence of metastasis in patients with RCC is approximately 33%, but less than 2% of this correspond to small intestine metastasis. Strict follow up is recommended because the recurrence of metastatic RCC is 11% after 10 years of the initial diagnosis. The radiological characteristics of the primary clear cell RCC depends on the modality of imaging used, but it will commonly demonstrate as a hypervascular exophytic mass. The metastatic lesions from the RCC tend to be similar of the primary tumor (hypervascular mass), when they appear on bone they show as lytic lesions. For the relapse of the clear cell RCC the treatment will from sole medical treatment to metastasectomy plus medical treatment.
Keywords: Kidney; carcinoma; metastasis; small intestine; clear cells
Introduction
The renal cell carcinoma (RCC) is among the 10 most common types of cancer in men and women, with an incidence of 64,000 cases per year in the United States. The clear cell subtype of RCC is the most common (70-88%) [1]. Approximately one third of the patients with RCC present with metastasis at the time of diagnosis [2], although the small intestine metastasis is a rare event, with reported prevalence that ranges from 0.7 to 14.6% and 1.7% [3,4], with only a few cases reported in the literature [3]. Here we report a case of jejunal metastasis from clear cell RCC in a 78 year old female with a personal history of left RCC treated with simple nephrectomy 20 years ago, presenting with the clinic of an upper gastrointestinal bleeding.
Case Report
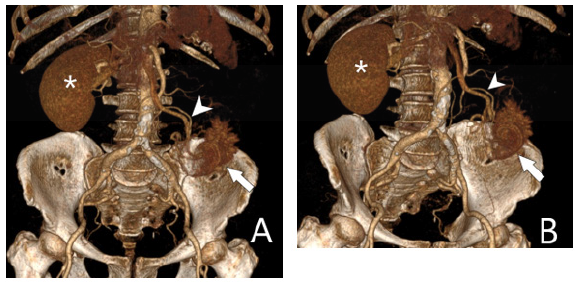
A 78 years old female presented to the emergency department, with a 7-day history of melena plus diffuse abdominal complains and hyporexia. The only relevant history was a left radical nephrectomy because a RCC, which was treated only with surgery. After the medical evaluation the hematic biometry showed an hypochromic microcytic anemia, after a normal upper gastrointestinal endoscopy an abdominal angiotomography was requested, demonstrating a bowel intussusception at the jejunum caused by an hypervascular mass (Figure 1), measuring 4.8 x 4.2 x 5.8 cm and the virtual rendering (VR) images demonstrates a rich vascular supply by the superior mesenteric arteries (Figure 2); no other relevant alterations where found. A metastasis from the RCC was suspected by imaging.
Figure 1: Abdominal Angiotomography demonstrating a jejunal intussusception originated by a lobulated hypervascular mass (arrowhead).
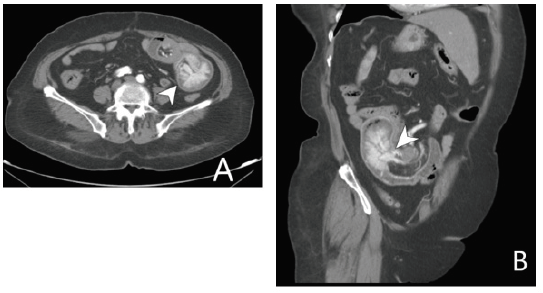
Figure 2: VR demonstrates the vascular supply (arrowhead) to the jejunal metastases (arrow); only the right kidney is seen (*).
The patient was prepared to surgery, she undergone a small bowel resection of the affected jejunum (30 cm), with primary anastomosis, the histologic diagnosis of jejunal metastasis of clear cell RCC was made by intraoperative frozen section and confirmed again by the final pathology. The patient had an excellent postoperative evolution. After that the patient went on chemotherapy, finishing all the cycles without major complications. Actually the patient is on oncologic surveillance and refers clinically asymptomatic.
Discussion
RCC accounts for 3% of the total of adult malignancies, arising
from the proximal tubular epithelium of the kidney, with a male
preponderance (M:F 2:1) [5]; the most common subtype of RCC
is the clear cell carcinoma [1], the other common subtypes are
papillary and chromophobe, accounting this three for more of
95% of the total [6]. The prevalence of metastasis in patients with
RCC is at least of one third of the total [2], but less than 2% of
this correspond to small intestine metastasis [4], which are rare,
occurring only in 0.4-4% patients with known malignancies [7].
The recurrence of metastatic RCC is 11% after 10 years of the initial
diagnosis, this is why a strict follow up is recommended after the
radical nephrectomy [8].
The incidence of small bowel metastases may be explained by
some factors that include, high change rate of the intestinal mucosal
cells and rapid transit of intestinal content, which causes a shorter
exposure to carcinogens [9]. The most common gastrointestinal
tract metastases originate from breast cancer (8.2–33%), melanoma
(10–26%), lung cancer (14%), and squamous cell carcinoma of the
esophagus; although the metastasis to the small intestine constitute only 2 % of the total of the gastrointestinal metastasis [10]. Spread
in RCC is lymphatic, haematogenous, transcoelomic, or by direct
invasion [8].
The radiological characteristics of the primary clear cell
RCC depends on the modality of imaging used, on ultrasound it
appears as an exophytic mass with abundant vascular flow in the
color Doppler [11]; on computed tomography (CT) it appears as
an heterogeneous mass, which is hypervascular (hyperdense) in
the arterial phase, with central necrosis and a tumor thrombus
extending into the renal and cava veins, CT is also useful because
it can be used to staging [6]. Magnetic resonance also plays a role
in the diagnosis of the RCC because the lack of use of ionizing
radiation and when the patient has a diminished renal function
[11]. The metastatic lesions from the RCC tend to be similar of the
primary tumor (hypervascular mass), when they appear on bone
they show as lytic lesions with soft tissue component [11]. For the
relapse of the clear cell RCC the treatment will depend on the risk
model to direct treatment and it will vary from medical treatment
(chemotherapy, immunotherapy) to metastasectomy plus medical
treatment [12].
Conclusion
The metastasis from RCC to the gastrointestinal tract constitutes a rare entity, but they need to be always considered in the presence of intestinal symptoms in a patient with prior history of RCC, even when it has passed more than 10 years after the initial treatment, because of the presence of the late metastases of the RCC which is a well described entity. The treatment for the relapse of the RCC consists of metastasectomy and chemotherapy.
References
- Weiss RH, Jaimes EA, Hu SL (2019) Kidney Cancer. In Brenner and Rector’s The Kidney, Philadelphia, USA, pp. 1392-1406.
- Gong J, Maia MC, Dizman N, Govindarajan A, Pal SK (2016) Metastasis in renal cell carcinoma: Biology and implications for therapy. Asian Journal of Urology 3(4): 286-292.
- Estévez-Boullosa P, Martínez-Turnes A, Carracedo-Iglesias R, Rodríguez-Prada JI (2017) Jejunal metastasis of renal cell carcinoma. Revista Española de Enfermedades Digestivas 109(2): 147-148.
- Bianchi M, Sun M, Jeldres C, Shariat SF, Trinh QD, et al. (2012) Distribution of metastatic sites in renal cell carcinoma: A population-based analysis. Annals of Oncology 23(4): 973-980.
- Sadler GJ, Anderson MR, Moss MS, Wilson PG (2007) Metastases from renal cell carcinoma presenting as gastrointestinal bleeding: Two case reports and a review of the literature. BMC Gastroenterology 7: 1-5.
- Muglia VF, Prando A (2015) Renal cell carcinoma: histological classification and correlation with imaging findings. Radiologia Brasileira 48(3): 166-174.
- Chang WT, Chai CY, Lee KT (2004) Unusual Upper Gastrointestinal Bleeding due to Late Metastasis from Renal Cell Carcinoma: A Case Report. Kaohsiung Journal of Medical Sciences 20(3): 137-141.
- Chawla A, Mishra D, Bansal R, Chundru M (2013) Rare sites of delayed metastasis in renal cell carcinoma. BMJ Case Reports 1(C): 1-5.
- Loualidi A, Spooren PFMJ, Grubben MJAL, Blomjous CEM, Goey SH (2004) Duodenal metastasis: An uncommon cause of occult small intestinal bleeding. Netherlands Journal of Medicine 62(6): 201-205.
- Hsu CC, Chen JJ, Changchien CS (1996) Endoscopic features of metastatic tumors in the upper gastrointestinal tract. Endoscopy 28: 249-253.
- Leveridge M, Bostrom P, Koulouris G (2010) Imaging renal cell carcinoma with ultrasonography, CT and MRI. Nat Rev Urol 7: 311-325.
- Motzer RJ (2019) Kidney Cancer.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




