Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Short Communication(ISSN: 2643-6760) 
Influence of obesity on the results of minimally invasive spine surgery to minimize surgical risks in patients with degenerative Lumbar disc disease Volume 1 - Issue 4
Inaki Arrotegui*
- Department of Neurosurgery, Spain
Received: December 17, 2018; Published: January 02, 2019
Corresponding author: Inaki Arrotegui, Department of Neurosurgery, Spain
DOI: 10.32474/SCSOAJ.2019.01.000120
Introduction
It is known that overweight / obesity is a factor of risk demonstrated for a multitude of diseases metabolic, cardiovascular, visceral and osteoarticular. In addition, there is growing literature evidence that relates obesity with an acceleration of the process of lumbar disc degeneration and this with the presence of chronic low back pain. Currently, obesity is defined based on the BMI, which can be calculated by means of a simple formula that relates the weight of the individual in kilograms with its height in meters raised to square (BMI = Kg /m2) [1-3].
Also, the interventions that are carried out in overweight/ obese patients present difficulties specific to the surgical technique itself, in general, because of the need for broader approaches, for the greater surgical time employed and a greater blood loss or worse healing of the wounds. Although obesity is not considered, in principle, an absolute contraindication for lumbar spine surgery, its presence does imply to assume a higher rate of perioperative complications compared to the general population [4].
Material
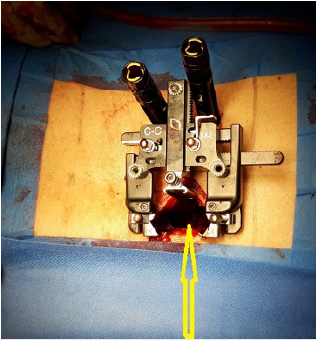
The osteoarthrosis in the obese at the level of the joints that support the weight of the body, is frequent, by altering its biomechanics and having to support great tensions above the normal resistance of the tissues the appearance of the minimally invasive surgery of the spine allows the surgery with less damage to soft tissues (muscles and ligaments) compared to open surgery, the potential benefits of MI surgery they are: better cosmetic results thanks to smaller incisions that heal better less blood loss during surgery. less muscle injury, with which recovery is faster (2-3 days of hospital stay) and the need for much less rehabilitation, less risk of infection, as there is much less tissue exposed during the intervention, less postoperative pain derived from the minimal tissue injury.
We included Degenerative Disc Disease patients undergoing surgical management with lumbar instrumentation, were divided into two groups according to their body mass index in obese (MIS) and obese (standard). An Oswestry questionnaire of functional capacity was applied to them preoperatively and one year later, the correlation between it and the BMI was measured. We included 50 patients in each group, 56 women and 44 men from 2014 to 2016. Clinical variables (such as return to work, hospital stay and postoperative pain) and variables measured intraoperatively (surgery time and loss of life) were evaluated. intraoperative blood).
Results
Patients treated with minimally invasive surgery techniques obtained better results comparing them with open surgery techniques and conservative methods, with a shorter hospital stay and greater speed at the time of recovering their work and social life. As for the other variables studied (especially the radiological ones, such as the height of the vertebral body or the kyphotic angle), there are no significant differences between the different therapeutic techniques. The average of the presurgical Oswestry disability index in obese patients was 47%, with one-year postsurgical follow-up, with an index of disability in obese patients of 23.84%.
Discussion
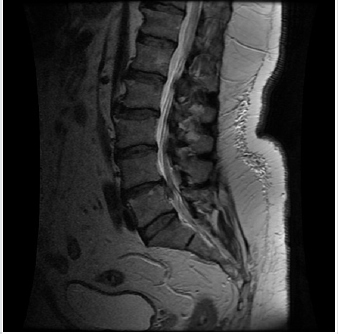
Obesity has been associated with longer surgical times, greater intraoperative blood loss, more surgical wound infections, higher incidence of postoperative thromboembolism, higher probability of peripheral nerve injury, higher overall mortality and worse wound healing of the surgical wound. The published works in which this issue is addressed are all retrospective series of cases [5,6]. An increase in surgical time implies more time anesthetic and may be associated with a higher rate of complications due to tissue ischemia that involves maintaining soft tissue retractors or retractors for longer periods of time. In addition, it can increase the likelihood of contamination of the surgical field as the time of surgical exposure increases. A larger surgical field can lead to an increase in blood loss and greater chances of surgical bed hematoma and the need for transfusion (Figure 1,2).
In the obese (BMI> 30) it at least doubles and, often triples, the rate of the non-obese. These data have been corroborated [7]. In the metanalysis of Shiri et al.9 where 93,183 are collected subjects and a global infection risk of 2.33 is reported times greater in the obese (95% CI: 1.97-2.79). This same study confirmed the relationship between obesity and incidence of thromboembolism (OR: 3.15, 95% CI: 1.92-5.17), mortality (OR: 2.6, 95% CI: 1.50-4, 49), need for revision surgery (OR: 1.43, 95% CI: 1.05-1.93), longer surgical time (OR: 14.55, 95% CI: 10.03-19.07) and greater blood loss (MD: 28.89, 95% CI: 14,20-43,58) [8,9].
Conclusion Obese Patients
BMI> 30% with the MIS technique presented a more favorable clinical evolution compared to the group of Obese patients with Standard surgery. The effect of minimally invasive surgery seems like a good alternative in these patients although, for the moment, is insufficiently substantiated in the literature. After this study, it is the technique of choice in our unit.
References
- National Institutes of Health (1998) Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults-The evidence report. Obese Res 6(Suppl2): 51S-209S.
- WHO (2017) Global Health Observatory (GHO) data. Overweight and obesity.
- Heymsfield SB, Wadden TA (2017) Mechanisms, pathophysiology, and management of obesity. N Engl J Med 376: 254-266.
- Urquhart DM, Berry P, Wluka AE, Strauss BJ, Wang Y, et al. (2011) 2011 Young Investigator Award winner: Increased fat mass is associated with high levels of low back pain intensity and disability. Spine (Phila Pa 1976) 36(16): 1320-1325.
- Samartzis D, Karppinen J, Cheung JP, Lotz J (2013) Disk degeneration and low back pain: Are they fat-related conditions? Global Spine J 3(3): 133-144.
- Balistreri CR, Caruso C, Candore G (2010) The role of adipose tissue and adipokines in obesity-related inflammatory diseases. Mediators Inflamm.
- Cao J, Kong L, Meng F, Zhang Y, Shen Y (2016) Impact of obesity on lumbar spinal surgery outcomes. J Clin Neurosci 28: 1-6.
- Jackson KL, Devine JG (2016) The effects of obesity on spine surgery: A systematic review of the literature. Global Spine J 6(4): 394-400.
- Shiri R, Karppinen J, Leino Arjas P, Solovieva S, Viikari Juntura E (2010) The association between obesity and low back pain: A meta-analysis. Am J Epidemiol 171(2): 135-154.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...