
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Gallstone Ileus in the Elderly: Still a Challenge, Report of a Case with Review of the Current Literature Volume 4 - Issue 1
Sascha Vaghiri1, Stephen N Fung1*, Dimitrios Prassas1, Lino Morris Sawicki2, Alexander Rehders1, Wolfram Trudo Knoefel1 and Andreas Krieg1
- 1Department of Surgery (A), Heinrich-Heine-University and University Hospital Duesseldorf, Moorenstrasse 5, 40225 Duesseldorf, Germany
- 2Institute of Diagnostic and Interventional Radiology, Heinrich Heine-University and University Hospital Duesseldorf, Moorenstrasse 5, 40225 Duesseldorf, Germany
Received: November 29, 2019; Published: December 11, 2019
Corresponding author: Stephen N Fung, Department of Surgery (A), Heinrich-Heine-University and University Hospital Duesseldorf, Moorenstrasse 5, 40225 Duesseldorf, Germany
DOI: 10.32474/SCSOAJ.2019.04.000176
Abstract
Introduction: Gallstone ileus is described as an intestinal obstruction caused by luminal gallstone impaction. It is a mainly geriatric disease with a prevalence of over 25 % in the elderly population. Morbidity and mortality rates are high which are caused due to the delayed presentation, diagnosis and treatment in comorbid patients. Interestingly, since the past century, the optimal surgical procedure in this type of mechanical ileus is still highly controversial and challenging.
Presentation of case: In the current paper we demonstrate our experience with a patient treated at our institution due to gallstone ileus. During surgical exploration the impacted stone in the terminal ileum was removed without preforming a cholecystectomy. This decision was made because of the unstable and septic status of the patient necessitating quick relief of the obstruction and no signs of ongoing severe peritonitis and acute Cholecystitis. She had an uneventful postoperative course.
Discussion & conclusion: While enterolithotomy is performed most commonly because of the low incidence of complications, the risk of developing recurrent biliary symptoms has led to a more aggressive approach with concomitant fistula repair and cholecystectomy.
Keywords: Gallstone ileus, elderly patients, surgical therapy, decision-making
Introduction
Gallstone ileus is a rare complication which is responsible for mechanical bowel obstruction in 1-4 % of the patients. With a higher prevalence of cholelithiais in the elderly (geriatric) predominantly female population, the incidence of gallstone ileus rises up to 25 % in this cohort [1,2]. The relatively high reported mortality and morbidity rates (12-23%) have been mainly attributed to the unspecific clinical symptoms, advanced aged patients with comorbidities and delay in diagnosis and subsequent adequate therapy (1,3,4). Gallstone ileus is mainly treated surgically with a prompt relief of the obstruction as the primary goal of every procedure[1-3-6]. The reported one or two step surgical strategies include 1) enterolithotomy alone with optional interval biliary intervention, or 2) enterololithotomy combined with cholecystectomy, fistula repair and possibly segmental bowel resection [7]. We present a case of gallstone ileus treated with simple enterolithotomy and report her postoperative clinical course.
Case Report
Our patient is a 62-year-old female initially admitted in a tertiary hospital with upper abdominal pain, recurrent vomiting, dehydration and respiratory deterioration. The past medical history included arterial hypertension and adipositas per magna (BMI 36 kg/m2). On examination her abdomen was distended in all 4 quadrants without signs of peritonitis. Lung auscultation was significant for rales on the left lung site. The laboratory results showed hypokalemia and severely elevated serum creatinine/ blood urea nitrogen levels suggesting acute renal failure. The inflammatory markers were high (CRP 33,8 mg/dl, WBC 11,600/ μl). Other blood testes including Bilirubin and LFT ‘s (Liver function test) were normal. An upper GI Endoscopy study revealed a duodenitis. A CT-scan was performed following further aggravation of the general health status with progredient septic pneumonia and hemodynamic instability. It demonstrated a large gallstone in the middle third of the ileum causing small bowel obstruction and pneumobilia of the biliary system (Figure1). Subsequently the Patient was referred on the second day after admission to our department where we performed a laparotomy. At exploration no signs of an ongoing peritonitis could be seen. The large (6 cm x 3 cm) impacted Gallstone (Figures 2&3) in the ileum was removed by opening the small intestine through a 3-cm longitudinal antimesenteric incision at the obstruction site.
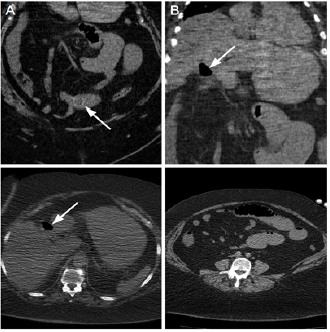
Figure 1: Computed tomography (CT) images of a 62 year-old obese woman with gallstone ileus. Coronal CT image
(A) shows a 2.5 cm ectopic gallstone in the ileum. Pneumobilia of the gall bladder as seen on coronal
(B) and transverse CT images
(C) Distended small bowel loops caused by ileal obstruction
(D) These features are consistent with Rigler’s triad and their presence is pathognomonic for gallstone ileus.
The affected bowel segment was not ischemic. Therefore, primary closure without bowel resection was performed. No other remnant stones were identified. Further exploration of the right upper quadrant revealed multiple dense adhesions between the omentum and the transverse mesocolon with the gallbladder. Because no signs of obvious severe inflammation of the surrounding tissue and the gallbladder could be elicited, further surgical exploration and cholecystectomy were not carried out with respect to the septic state of our patient. The postoperative recovery period was uneventful. Dialysis could be discontinued. Under antibiotic regimen the inflammatory parameters decreased. The patient developed an atrial fibrillation which could be managed with antiarrthymic medication. She was discharged on postoperative day 12. A second step procedure with concomitant cholecystectomy and fistula closure down will be scheduled in a disease-free interval.
Discussion
Gallstone ileus is a potentially life-threatening condition where
one or multiple migrated gallstones get impacted in the bowel
lumen. Cholelithiasis accounts for approximately 1-4 % of all cases
of mechanical non-strangulated bowel obstruction. This incidence
rises up to 25 % in patients aged over 65 years as gallstone disease
becomes more evident in the elderly [1,2,4]. The male-female
ratio is 1 to 3-16 % in favor of female patients with an average age
between 66-73 years at the time of presentation [4,5,8]. Many of
these patients have relevant comorbidities including cardiovascular
and metabolic disease which contribute to the high perioperative
mortality and morbidity. The overall mortality ranges from 7 to
23 % [1,4,7,9]. Pathophysiolagically recurrent chronic or acute
gallbladder inflammation causes adherent bowel perforation and
thus cholecystoenteric fistula formation where the stone passes
into the intestinum [5,8]. The stone can theoretically occlude
any level of the bowel, but the terminal ileum and ileocecal valve
constitute the predilection site with 54 % as the narrowest part
of the small bowel with reduced peristaltic activity. Following the
ileum, the jejunum and duodenum are affected in 27 % and 1-3 %.
The least possible site of obstruction is the colon [1,4,8]. Symptoms
of gallstone ileus are similar to those of mechanical small bowel
obstruction. They may be intermittent and variable because the
stone lodges at different levels and moves downwards until its
final destination of impaction. An observation called “tumbling”
phenomenon [8]. These characteristics of an intermittent and
incomplete obstruction in the initial stages are responsible for the
delay in diagnosis and treatment leading to deterioration of the
preoperative status.
The interval between onset of symptoms and the time of
admission to the hospital and surgical intervention averages
between 3 to 7 days [3-5, 8-11]. The perioperative diagnostic rate
ranges between 13 to 50 % which means that more than half of the
patients with gallstone ileus remain undiagnosed until laparotomy
for suspected mechanical obstruction or at autopsy [1,3,4,10,11].
The radiographic images play an important role in the perioperative
diagnosis. The rigler triad on plain abdominal films includes 1)
pneumobilia 2) an ectopic gallstone and 3) distended small bowel
loops. The presence of these features is pathognomonic. However,
they are not seen regularly and only less than 40 % of the patients
exhibit 3 or 2 criteria [4,8,10,12,13]. Plain CT- Scan shows a higher
overall sensitivity (93%) and diagnostic accuracy (77-99%) in
detecting ectopic gallstones, the site of bowel obstruction and
the bilioenteric fisula [12,13]. The proper treatment modality
in gallstone ileus is still controversially debated since the last
century [1,3,5,8]. The surgical treatment strategy encompasses
either enterolithotmy with optional interval cholecystectomy
or a one stage combined procedure with enterolithotmy,
cholecystectomy and fistula closure. The main goal of any therapy
is the prompt relief of bowel obstruction and life preservation in
an emergency situation. In many patients the delayed diagnosis
leads to a significantly instable vital status secondary to volume
depletion, peritonitis and sepsis. Therefore, a careful perioperative
resuscitation management must be applied timely prior to surgery.
Many investigators recommend a simple enterolithotomy as the
initial surgical procedure in debilitated patients [1-5,7,10,11,14]. A
short procedure time with less extensive dissection of the fragile
tissue taking into account the impaired healing capacity in this
group of high-risk patients is anticipated by this approach compared
to the one step strategy. However the late term consequences and
complications of a persistent biliary-enteric fistula (e.g. recurrent symptomatic cholecystitis[4], cholangitis, significant increase in
gallbladercarcinoma [4,5,8], malabsorption symptoms [5] and
severe upper GI bleeding [4]) have led some researchers to propose
a more aggressive and complex approach including enterolithotomy
with concomitant cholecystectomy and fistula repair in a combined
one step procedure as a feasible option [2,4-6,15].
This treatment opportunity is predominately reserved
for low risk patients with less comorbidities with absolute
indications for biliary surgery and after proper patient selection
and perioperative resuscitation. Generally, the overall mortality
rates recorded of the one-stage operation are slightly higher (17-
33 %) than the enterolithotomy alone (12-19 %) although not
statistically significant [1,3-5,7]. Because of its rarity, surgical
outcomes of patients with gallstone ileus have only been studied
retrospectively with disparities in diagnostic and treatment
strategies. Which surgical procedure is performed should also
be strongly adapted to the intraoperative findings [3] Careful
exploration of the bilioenteric fistula and gallbladder is advised
to evaluate the presence of gastrointestinal leakage, abscess or
gallbladder empyema formation and additional stones [8]. While a
subacutely inflamed gallbladder could be leaved untouched, acute
or gangrenous cholecystitis and residual stones may warrant the
one stage procedure with definitive fistula closure [3,10]. On the
other side Laparoscopic surgical interventions Soto et al. [16] and
a variety of non-surgical stone removal techniques e.g. endoscopic
mechanical and electrohydraulic lithotripsy [17] or extracorporal
shockwave lithotripsy (ESWL) [18] have been successfully applied
in selected cases but have their own limitations depending on
the site of obstruction. The presented case was a younger patient
with less comorbidities. Simple enterolithotomy was indicated
due to a fulminant pneumogenic sepsis and renal failure requiring
immediate intensive care surveillance. The choice of the surgical
method was strictly adapted to the intraoperative assessment of
the local conditions as described above. Careful exploration of the
whole bowel should be carried out to avoid remnant gallstones
causing recurrent obstruction. In the presence of residual stones the
estimated recurrence rate of gallstone ileus ranges from 5 %to 17
%, mostly within 2-6 months after the first operation [19,20]. Our
patient was asymptomatic during follow-up at 6 weeks, bringing a
second elective operation with cholecystectomy and fistula repair
down into question based on the current incongruent literature
and the lack of large scale randomized clinical trials.
Conclusion
The choice of surgical procedure is strongly depended on the clinical presentation of the patient and intraoperative findings. It should balance the risk and benefits of each approach taking in account that most cases are elderly patients with comorbid conditions and subsequent debilitated general health status due to delayed diagnosis. The one stage procedure with fistula closure has a reportedly higher mortality and morbidity rate and is therefore indicated in younger low-risk patients. Nevertheless, enterolithotomy alone predisposes to the complications of persistent bilioenteric fistula including recurrent gallstone ileus, cholangitis and cholecystitis with the necessity of a reintervention. Despite recent decreasing mortality rates and advances in the perioperative care Gallstone ileus is still a challenging and fatal disease among the elderly, a timely diagnosis and proper treatment strategy impact patient’s outcome. Simple enterotomy with stone removal is recommended by many authors as the initial surgical procedure followed by a delayed second step approach if necessary.
Conflicts of interest
There are no conflicts of interest
Funding
The authors declare that there were no sources of funding during all steps of this research project.
Ethical Approval
The Ethics Committee of the Heinrich Heine University Düsseldorf and University Hospitals Düsseldorf confirms that this Case report does not require the formal vote of its Ethics Committee based on the current laws.
Consent
An informed consent was obtained from the patient. All the patient related data and pictures were anonymised.
Author contribution
Andreas Krieg operated on the patient and contributed to the study concept and design, data acquisition, editing and critically revising the final manuscript; Sascha Vaghiri contributed to the study concept and design, data collection and analysis, writing the final manuscript, and literature review; Stephen N Fung, Dimitrios Prassas and Alexander Rehders contributed to writing of the final manuscript; Lino Morris Sawicki overwieved the radiographic examinations and provided the CT-Images; Wolfram Trudo Knoefel critically analysed and revised the final manuscript.
References
- Reisner RM, Cohen JR (1994) Gallstone ileus: a review of 1001 reported cases. Am Surg Juni 60(6): 441-446.
- VanLandingham SB, Broders CW (1982) Gallstone ileus. Surg Clin North Am April 62(2): 241-247.
- Rodríguez Sanjuán JC, Casado F, Fernández MJ, Morales DJ, Naranjo A (1997) Cholecystectomy and fistula closure versus enterolithotomy alone in gallstone ileus. Br J Surg 84(5): 634-637.
- Kasahara Y, Umemura H, Shiraha S, Kuyama T, Sakata K, et al. (1980) Gallstone ileus. Review of 112 patients in the Japanese literature. Am J Surg 140(3): 437-440.
- Clavien PA, Richon J, Burgan S, Rohner A (1990) Gallstone ileus. Br J Surg 77(7): 737-742.
- Kirchmayr W, Mühlmann G, Zitt M, Bodner J, Weiss H, et al. (2005) Gallstone ileus: rare and still controversial. ANZ J Surg 75(4): 234-238.
- Halabi WJ, Kang CY, Ketana N, Lafaro KJ, Nguyen VQ, et al. (2014) Surgery for gallstone ileus: a nationwide comparison of trends and outcomes. Ann Surg 259(2): 329-335.
- Abou Saif A, Al Kawas FH (2002) Complications of gallstone disease: Mirizzi syndrome, cholecystocholedochal fistula, and gallstone ileus. Am J Gastroenterol 97(2): 249-254.
- Ayantunde AA, Agrawal A (2007) Gallstone ileus: diagnosis and management. World J Surg 31(6): 1292-1297.
- Doko M, Zovak M, Kopljar M, Glavan E, Ljubicic N, et al. (2003) Comparison of surgical treatments of gallstone ileus: preliminary report. World J Surg 27(4): 400-404.
- Tan YM, Wong WK, Ooi LL (2004) A comparison of two surgical strategies for the emergency treatment of gallstone ileus. Singapore Med J 45(2): 69-72.
- Lassandro F, Romano S, Ragozzino A, Rossi G, Valente T, et al. (2005) Role of helical CT in diagnosis of gallstone ileus and related conditions. AJR Am J Roentgenol 185(5): 1159-1165.
- Yu C Y, Lin C C, Shyu R Y, Hsieh C B, Wu H S, et al. (2005) Value of CT in the diagnosis and management of gallstone ileus. World J Gastroenterol WJG 11(14): 2142-2147.
- Martínez Ramos D, Daroca José JM, Escrig Sos J, Paiva Coronel G, Alcalde Sánchez M, et al. (2009) Gallstone ileus: management options and results on a series of 40 patients. Rev Esp Enferm Dig 101(2): 117-20, 121-4.
- Riaz N, Khan MR, Tayeb M (2008) Gallstone ileus: retrospective review of a single center’s experience using two surgical procedures. Singapore Med J 49(8): 624-626.
- Soto DJ, Evan SJ, Kavic MS (2001) Laparoscopic management of gallstone ileus. JSLS J Soc Laparoendosc Surg Soc Laparoendosc Surg 5(3): 279-285.
- Bourke MJ, Schneider DM, Haber GB (1997) Electrohydraulic lithotripsy of a gallstone causing gallstone ileus. Gastrointestinal Endoscopy 45(6): 521-523.
- Dumonceau JM, Delhaye M, Devière J, Baize M, Cremer M (1997) Endoscopic treatment of gastric outlet obstruction caused by a gallstone (Bouveret’s syndrome) after extracorporeal shock-wave lithotripsy. Endoscopy 29(4): 319-321.
- Dai X Z, Li G Q, Zhang F, Wang X H, Zhang C Y (2013) Gallstone ileus: case report and literature review. World J Gastroenterol 19(33): 5586-5589.
- Mir SA, Hussain Z, Davey CA, Miller GV, Chintapatla S (2015) Management and outcome of recurrent gallstone ileus: A systematic review. World J Gastrointest Surg 7(8): 152-159.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...






