Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Fibrous Dysplasia of the Orbital Roof : A Case Report Volume 7 - Issue 1
Kadiri Alaoui N *, Abdenbaoui B, Lakhdar F, Benzagout M, Chakour K, Chaoui MF
- Department of Neurosurgery, University Hospital Hassan Ii, Morocco
Received:June 25, 2022; Published:July 14, 2022
Corresponding author: N Kadiri Alaoui, Department of Neurosurgery, University Hospital Hassan Ii, Morocco
DOI: 10.32474/SCSOAJ.2022.07.000251
Abstract
We present the case of an 17-year-old man who was referred to our department for right proptosis. Preoperative imaging showed an aneurysmal cyst like images. Complete tumor removal was performed via a subfrontal Approaches, no reconstruction was needed. Histology suggested a Fibrous Dysblasia.
Introduction
FD is a benign fibro-osseous developmental disorder of the growing bone in which fibrous and osseous tissue replace the normal medullary bone It represents approximately 2.5% of all bone tumors the majority of patients diagnosed before the age of 30 years [1]. FD is classified into two types: Monostotic Fibrous Dysplasia (MFD) and Polyostotic Fibrous Dysplasia (PFD). MFD accounts for 70% of the total. Only 2-3% of cases of FD are associated with endocrine disorders (MAS) [2]. It occurs mostly in the craniofacial skeleton [3]. Proptosis is considered Primary ocular complications of craniofacial FD [4]. The most common type of malignant transformation is sarcomatous change, which occurs in 5% of cases [5].
Case Report
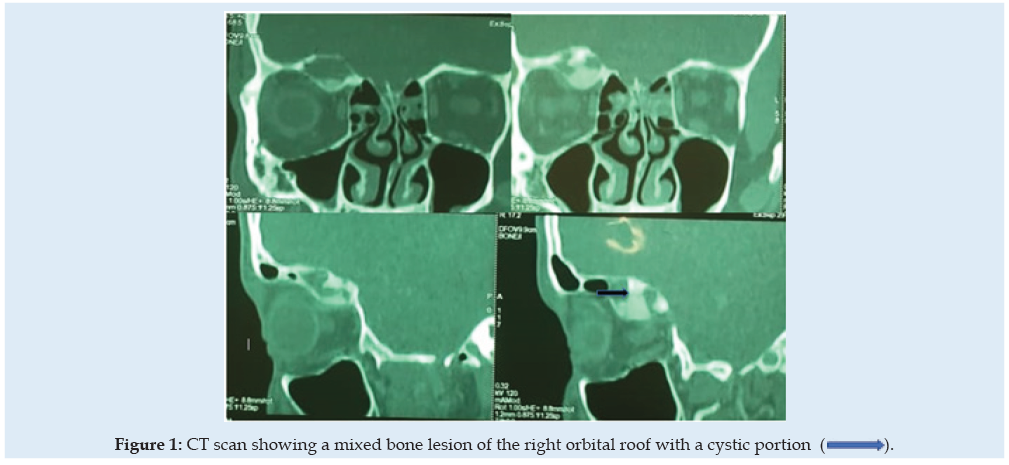
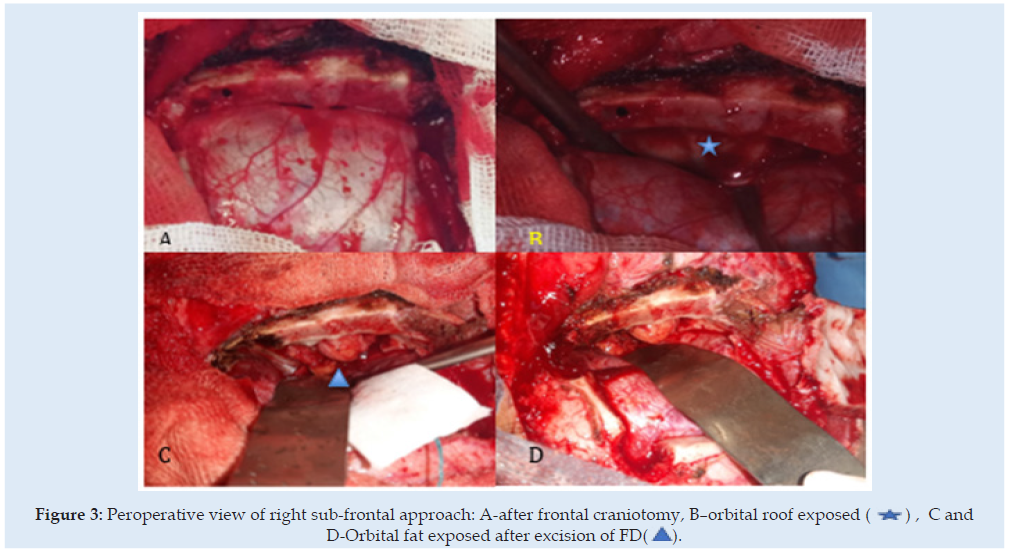
A 17-year-old man was referred to our hospital for a nonpulsatile, painless right eye exophtalmy. His acuity and field of vision were both normal. A CT scan revealed an expansile bone mass and cystic swelling on the right orbital roof Figure 1. An orbital MRI revealed a homogeneously dense pattern with a high contrast inhence in T1 Figure 2. The right globe and optic nerve were not damaged, the all was suggestive of an aneurysmal bone cyst. We decided to remove the lesion because of the right proptosis using a right extradural subfrontal approach Figure 3. No reconstitution of the orbital roof was required. The regression of the exophtalmy highlighted, the post-operative findings. The histopathological concluded to a FD. A six months follow-up, didn’t show any abnormal sensations or pain. There was no proof of tumoral recurrence.
Figure 2: Heterogeneously dense pattern with a high contrast inhence in T1, CSF like density in T2 sequence.
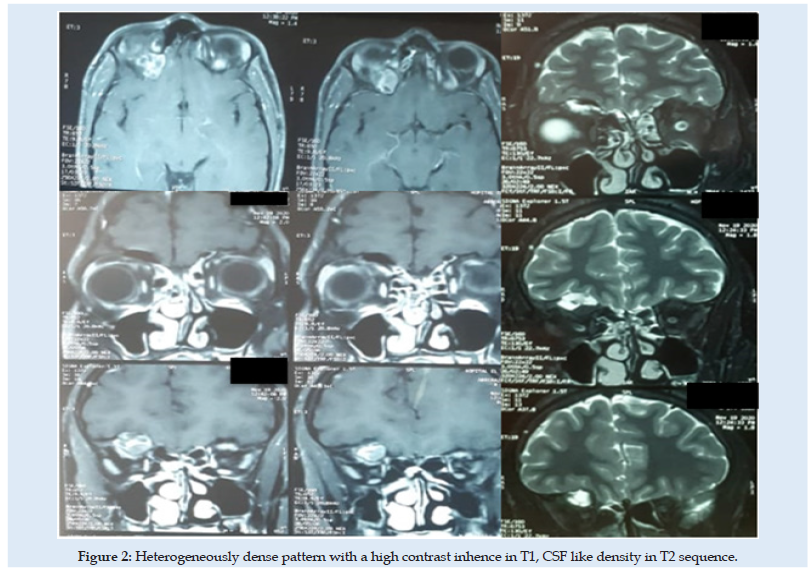
Figure 3: Peroperative view of right sub-frontal approach: A-after frontal craniotomy, B–orbital roof exposed (*) , C and D-Orbital fat exposed after excision of FD( ).
Discussion
A craniofacial FD is defined as a FD in which the lesions are confined to contiguous craniofacial skeleton bones. Because of the involvement of multiple adjacent craniofacial skeleton bones, most cases of craniofacial FD cannot be classified as monostotic. They are also not truly polyostotic because bones outside of the craniofacial complex are not affected [1]. The most frequent ophthalmic sign is proptosis [4], the typical characteristics of FD on CT may vary from a“ground-glass” or homogenous appearance to a mixed lesion as the patient ages, it changes from a homogenous, radio-dense lesions in prepeburtial patients. The FD lesions progress to a hetergenous appearance, as presented in our case [6].
In patients with FD, the presence of cortical destruction is an indicator of malignant transformation [7]. More than half of all malignant neoplasms in FD are osteosarcomas [8]. Secondary cystic degeneration within FD rarely occurs, and is radiologically interpreted as a secondary aneurysmal bone cyst [3]. The goal of treating FD in the skull base, around vital structures such as the optic nerve is to correct functional problems, to achieve asthetic improvement, but rarely to prevent function problems because optic nerve decompression is not warranted [1,7]. In asymptomatic patients, observation is appropriate [7], but when Surgery is decided, one should balance between performing a total excision and just correcting the deformed craniofacial skeleton [1].
Conclusion
Fibrous dysplasia is described as a benign disease, though severe and defigurating presentations have been described.
Radiological finding may be not suggestive. Here we describe a case of a 17-year-old male with monostotic FD of the roof orbit miming an aneuvresmal cyst. Management may vary from observation to large excision with special consideration to asthetic aspects.
References
- Pruksapong C, Lohwongwatana B (2020) Orbitocranial Fibrous Dysplasia: Immediate Reconstruction with Titanium 3-dimensional Printing. Plast Reconstr Surg Glob Open 8(9): e3114.
- De Salvo S, Pavone V, Coco S, Dell’Agli E, Blatti C, et al. (2022) Benign Bone Tumors: An Overview of What We Know Today. Journal of Clinical Medicine 11(3): 699.
- Lee HS, Koh YC, Roh HG, Park HK, Kim SY (2018) Secondary Aneurysmal Bone Cyst in a Craniofacial Fibrous Dysplasia: Case Report. Brain Tumor Research and Treatment 6(2): 86-91.
- Bibby K, McFadzean R (1994) Fibrous dysplasia of the orbit. Br J Ophthalmol 78(4): 266-270.
- Schwartz DT, Alpert M (1964) The Malignant Transformation of Fibrous Dysplasia. Am J Med Sci 247: 1–20.
- Lee J, FitzGibbon E, Chen Y, Kim H, Lustig L, et al. (2012) Clinical guidelines for the management of craniofacial fibrous dysplasia. Orphanet Journal of Rare Diseases 7(Suppl 1): S2.
- Singh V, Gupta K, Salunke P (2019) Monostotic craniofacial fibrous dysplasia: report of two cases with interesting histology. Autops Case Rep 9(2): e2018092.
- Riddle NM, Yamauchi H, Caracciolo JT, Johnson D, Letson GD, et al. (2009) Dedifferentiated chondrosarcoma arising in fibrous dysplasia: A case report and review of the current literature. PLMI 1: 1-6.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...