Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Fasciotens© Abdomen ICU: Novel Device Prevents Abominal Wall Retraction and Facilitates Early Abdominal Wall Closure of Septic Open Abdomen Volume 4 - Issue 1
Stephen N Fung, Vaghiri S, Ashmawy H*, Kropil F, Rehders A and Knoefel WT
- Department of Surgery (A), Heinrich-Heine-University and University Hospital Duesseldorf, Moorenstrasse 5, 40225 Duesseldorf, Germany
Received: November 30, 2019; Published: December 11, 2019
Corresponding author: Ashmawy H, Department of Surgery (A), Heinrich-Heine-University and University Hospital Duesseldorf, Moorenstrasse 5, 40225 Duesseldorf, Germany
DOI: 10.32474/SCSOAJ.2019.04.000177
Abstract
One of the major challenges in the management of patients with open abdomen (OA) due to septic peritonitis (SP) or abdominal compartment syndrome (ACS) is to control abdominal wall retraction. We herein present a novel device which was successfully implemented on a 49 years old patient with OA caused by necrotizing pancreatitis. Based on a dynamic Fascia-Mesh-Thread- Tensioning System (FMTTS), this device named Fasciotens© Abdomen ICU prevented abdominal wall retraction and even displayed abdominal wall extension. Fasciotens© Abdomen ICU has been successfully implemented in preclinical studies of animal models and was approved for CE-1 certification.
Keywords: Fasciotens® Abdomen ICU; prevention of fascia retraction, open abdomen
Abbreviaions: CECT: Contrast-Enhanced Computed Tomography; OA: Open Abdomen; FMTTS: Fascia-Mesh-Thread-Tensioning System; NPWT: Negative Pressure Wound Therapy; VACM: Vacuum and Mesh Mediated Fascial Traction
Introduction
Open abdomen (OA) therapy is often indispensable and lifesaving
in patients with septic peritonitis, abdominal compartment
syndrome, or at damage control surgery after trauma [1]. Patients
with OA have a high risk of major complications such as multiple
organ failure (30%-40%) [2,3], intraabdominal abscess formation
(83%), abdominal wall hernia (25%) [4], and enterocutaneous
fistula formation (2%–25%) [5,6]. Mortality of OA has been reported
with rates up to 40% and it is associated with increased rates in
cases with infection [1]. In a recent study, a significant increase
of complication rates after 8 days of OA therapy was reported [7].
Therefore, early closure of OA should be one of the major goals.
One of the major challenges for treatment of patients with OA
is primarily to control sepsis and prevent multiple organ failure
and secondly, to prevent fascia retraction of temporary closed
abdominal wall for delayed primary closure. Previously, various
temporary abdominal closure techniques of OA have been proposed
[2,8-10]. All of these methods insufficiently counteracted fascia
retraction and displayed only, if perfomed, higher traction on the
fascia by stepwise closing of the fascia during repeated abdominal
exploration [11]. Hence, many OA patients frequently develop
large ventral hernias of the abdominal wall, that require complex
repair surgery at a later stage [4]. Fasciotens© Abdomen ICU (Essen,
Germany) is a novel device based on dynamic Fascia-Mesh-Thread-
Tensioning System (FMTTS). This device allows decompression
of increased abdominal pressure, prevents fascial retraction
and facilitates early abdominal wall closure in patients with OA.
Fasciotens© Abdomen ICU has been successfully implemented in
preclinical studies of porcine animal model [12]. In the present
case, we report the use of Fasciotens© Abdomen ICU in an OA
patient with generalized sepsis due to necrotizing pancreatitis.
Case Report
A 49 years old patient with a history of alcohol induced
necrotizing pancreatitis previously diagnosed with Contrastenhanced
Computed Tomography (CECT) scan and treated
conservatively at the department of internal medicine of an
associated teaching hospital of our university clinic was relocated due to generalized sepsis in December 2018 for further treatment
in the ICU of our surgical department. On admission, the patient
was on mechanical ventilation and hemodynamic unstable. Blood
chemistry on admission showed increased levels of leucocytes
(25.5 x 1000/μl), C-reactive protein (20.2 mg/dl) and serum
amylase (629 U/L). Despite conservative therapy with calculated
antibiotics, analgesia and intravenous fluid substitution, the
patient´s clinical condition progressively worsened. CECT-scan
four days after admission showed a progression of the necrotizing
pancreatitis with peripancreatic fluid collection as well as ascites.
Because of the high risk of bowel perforation, image-guided
percutaneous catheter drainage of the necrotic peripancreatic
fluid collection, was not performed. On the fifth day of clinical
course, the patient developed ACS. After emergency decompressive
laparatomy, necrosectomy and abdominal lavage, the abdominal
cavity was sealed temporary with a Bogotá bag. On a period of two
weeks, daily abdominal lavage with necrosectomy of the pancreatic
necrosis was performed. Here, temporary closure of the abdominal
cavity was carried out with a vicryl mesh. Three weeks after
pulmonary and hemodynamic stabilization, Fasciotens© Abdomen
ICU was applied.
Despite the unfavourable Björck grade 3 [12] (Figure 1)
classification of the patients OA and initially retracted fascia,
Fasciotens© Abdomen ICU was implemented. Prior to application,
the patient was intraoperative fully relaxed using a muscle relaxant
agent (Esmeron®), before the gap between both fascial margins was
measured (15 cm)(Figure 2). After abdominal lavage and surgical
debridement of the fascia to create clean mobile fascia margins, a
doubled vicryl mesh (maximum. width: 2-3cm) was sewed at both
fascial margins. Hereafter, twelve commercial surgical threads, with
six attached at each side to defined areas on both meshes (Figure 2)
were then crossly tensed on the Fasciotens© Abdomen ICU clamping
system (Figures 3&4). The abdominal cavity was temporary sealed
with a Bogotá bag and abdominal cloths (Figures 2&4). During
repeated abdominal exploration 48 hours after Fasciotens©
Abdomen ICU implementation, a significant gap reduction of 5 cm
between both fascial margins was evident (initialy 15 cm). Further
abdominal exploration on-demand using the dynamic tension of
Fasciotens© Abdomen ICU also proved abdominal wall extension.
Two weeks after the device application, the abdominal wall was
successfully closed (Figure 5). Four days prior to abdominal wall
closure, the patient was extubated and the extended abdominal
wall temporary closed with a vicryl mesh to facilitate surgery for
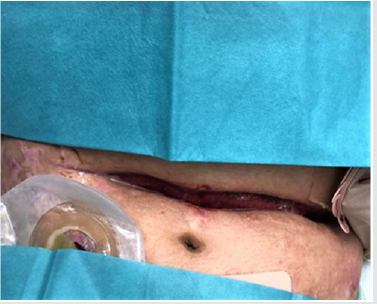
repeated lavage. A postoperative subcutaneous wound healing
disturbance (Figure 5) which occured after abdominal wall closure
was successfully treated one week later at our outpatient clinic. A
ventral hernia was not evident during Follow-up at our outpatient
clinic.
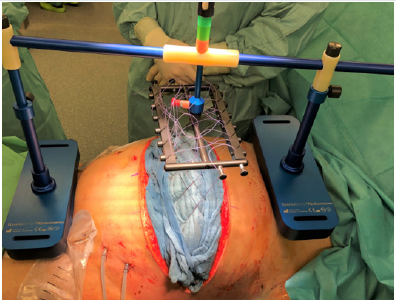
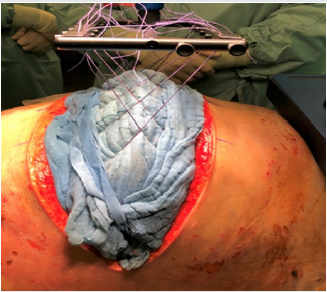
Figure 2: After abdominal lavage and debridement of the fascia, a double vicryl mesh was attached on both fascial margins and 6 commercial surgical threads were sewed on each side of the vicryl mesh. The abdomen was temporary sealed with a Bogotá bag. The gap between both fascial margins was measured.

Figure 3: Surgical cloths placed on the Bogotá bag. The surgical threads are crossly tensed on the common supension of Fasciotens© Abdomen ICU.
Device description
The main principle of the device is the application of ventrallydirected traction along both fascial margins over a clamping system (Figure 4). It consists of a beam with two buttresses applied to the thorax and anterior pelvic ring. After midline or transverse laparatomy, a doubled vicryl mesh sewed at both fascial margins and looped using commercial sutures distributes traction force along the entire length of the fascial edges. Six sutures on the mesh of each fascial margin carried through eyelets are fastened on a common suspension. The eyelet suspension is attached to the longitudinal beam with a height-adjustable connection. Using this dynamic connection, the fascial traction can be increased or decreased as needed. In this case, we adjusted the fascial traction to the dark green field of the longitudinal beam. This field corresponds to a traction force of 80 Newton according to the manufacturer´s specifications. Once suspended and tensed on the ajustable longitudinal beam, the fascial margins are pulled anteriorly relative to the thorax and pelvis. This prevents the natural muscle traction and the resulting fascial retraction and also promotes anterior extensive tissue development. Simultaneously, the open abdomen allows pressure release.
Discussion
In this case report, a novel device which prevents facial retraction and facilitates early abdominal wall closure was successfully implemented for the first time on a patient with open abdomen (OA). Despite OA for three weeks prior to Fasciotens© Abdomen ICU application, closure of the patient´s septic abdomen was achieved in two weeks. However success rate of abdominal closure depends on the etiology [13]. Patients with septic abdomen or higher Björn grade (grade 2B-4) have lower chance of fascial closure compared to non-septic or lower Björn grade (1A-2A) [2,10]. Up to date, treatment of the OA underlies a negative pressure wound therapy (NPWT). Although NPWT has been reported to have the best closure results, NPWT is also associated with a high rate of incisional hernias [15]. Recently, various closure methods for OA have been proposed. In the study of Acosta et al. [10] high rates (>90%) of primary delayed fascial closure were achieved with vacuum and mesh mediated fascial traction (VACM) after aortic repair. Here, the median duration of OA was 11 days. However, this high rates of fascial closure were observed in patients with non-septic abdomen (Björn grade 1A). In contrast, in the study of Verdam FJ al [2] primary abdominal closure rate of 88 % of patients with septic open abdomen was achieved using an Abdominal Reapproximation Anchor System (ABRA®). Here, primary abdominal closure of the midline was accomplished in 15 days (range: 7–30 days). Supported with NPWT, the ABRA® system approximates the wound margins through dynamic traction exerted by transfascial elastomers. Despite primary midline closure with ABRA®, high rates of pressure sores of the skin and dermis as well as ventral hernias were observed. In this case, Fasciotens© Abdomen ICU was applied on a patient with OA under general anesthesia. 48 hours after Fasciotens© Abdomen ICU application and during further repeated abdominal exploration, we observed a significant reduction of the gap between both fascial margins. Fascia traction und fascia extension leading to delayed primary closure was achieved with the dynamic tension of this device. Application of NPWT was not perfomed due to frequent lavage. As reported on the preclinical porcine model of Eickhoff et al. [12], the exerting pressure of this device on the thorax did not affect the breathing and vital signs of our patient. Furthermore, we observed no pressure sores of the skin despite pressure exerted by the buttresses on the thorax and the anterior pelvic ring. However, repositioning of the buttresses and readjustment of the longitudinal beam was frequently undertaken after positioning of the patient, in order to maintain tension on the fascia.
Conclusion
In conclusion, the implementation of Fasciotens© Abdomen ICU prevented in this case further fascia retraction and also enhanced abdominal wall extension. This could reduce the necessity of complex abdominal wall reconstructions as well as the rate of mesh graft transplantation. Moreover, this could be of socio-economic importance due to reduction of the length of hospitalisation. However, a prospective study with a large number of patients is needed to investigate feasibility and efficacy regarding fascial conditioning.
Conflicts of interest
There are no conflicts of interest
Funding
Fasciotens GmbH (Essen, Germany) provided the device. They were not involved in analysis, interpretation of data and in writing the manuscript.
Ethical Approval
The Ethics Committee of the Heinrich Heine University Düsseldorf and University Hospitals Düsseldorf confirms that this Case report does not require the formal vote of its Ethics Committee based on the current laws.
Consent
An informed consent was obtained from the patient. All the patient related data and pictures were anonymised.
Author contribution
Fung SN designed, wrote the report, analyzed and interpreted the data; Vaghiri S and Rehders A were attending doctors of the patient; Kröpil F, Fung SN and Vaghiri S performed the operation; Ashmawy H, Rehders A. and Knoefel WT critically revised the report and gave important intellectual input
Acknowledgements
none
References
- Bruhin A, Ferreira F, Chariker M, Smith J, Runkel N (2014) Systematic review and evidence based recommendations for the use of negative pressure wound therapy in the open abdomen. Int J Surg 12: 1105-1114.
- Verdam FJ, Dolmans DE, Loos MJ, Raber MH, de Wit RJ, et al. (2011) Delayed Primary Closure of the Septic Open Abdomen with a Dynamic Closure System. World J Surg 35: 2348-2355.
- Balogh Z, McKinley BA, Holcomb JB, Miller CC, Cocanour CS, et al. (2003) Both primary and secondary abdominal compartment syndrome can be predicted early and are harbingers of multiple organ failure. J Trauma 54: 848-859.
- Nicholas JM, Rix EP, Easley KA, Feliciano DV, Cava RA, et al. (2003) Changing patterns in the management of penetrating abdominal trauma: the more things change, the more they stay the same. J Trauma 55: 1095-1108.
- Gäddnäs F, Saarnio J, Ala-Kokko T, Laurila J, Koivukangas V (2007) Continuous retention suture for the management of open abdomen: a high rate of delayed fascial closure. Scand J Surg 96: 301-307.
- Perez D, Wildi S, Demartines N, Bramkamp M, Koehler C, et al. (2007) Prospective evaluation of vacuum-assisted closure in abdominal compartment syndrome and severe abdominal sepsis. J Am Coll Surg 205(4): 192-586.
- Hecker A, Hecker B, Hecker M, Riedel JG, Weigand MA, et al. (2016) Acute abdominal compartment syndrome: current diagnostic and therapeutic options. Langenbeck’s Arch Surg 401(1): 15-24.
- De Waele JJ, Kaplan M, Sugrue M, Sibaja P, Bjorck M (2015) How to deal with an open abdomen? Anaesthesiol Intensive Ther 47: 372-378.
- Roberts DJ, Zygun DA, Grendar J, Ball CG, Robertson Hlet al. (2012) Negative-pressure wound therapy for critically ill adults with open abdominal wounds: a systematic review. J Trauma Acute Care Surg 73(3): 629-639.
- Acosta S, Seternes A, Venermo M, Vikatmaa L, Sörelius K, et al. (2017) Open Abdomen Therapy with Vacuum and Mesh Mediated Fascial Traction after Aortic Repair: an International Multicentre Study. Eur J Vasc Endovasc Surg 54(6): 697-705.
- Wondberg D, Larusson HJ, Metzger U, Platz A, Zingg U (2008) Treatment of the open abdomen with the commercially available vacuum-assisted closure system in patients with abdominal sepsis: low primary closure rate. World J Surg 32(12): 2724-2729.
- Eickhoff R, Guschlbauer M, Maul AC, Klink CD, Neumann UP, et al. (2019) A new device to prevent fascial retraction in the open abdomen - proof of concept in vivo. BMC Surg 19: 82.
- Björck M, Bruhin A, Cheatham M, Hinck D, Kaplan M, et al. (2009) Classification-important step to improve management of patients with an open abdomen. World J Surg 33: 1154-1157.
- Hofmann AT, Gruber-Blum S, Lechner M, Petter-Puchner A, Glaser K, et al. (2017) Delayed closure of open abdomen in septic patients treated with negative pressure wound therapy and dynamic fascial suture: the long-term follow-up study. Surg Endosc 31(11): 4717-4724.
- Tsuei BJ, Skinner JC, Bernard AC, Kearney PA, Boulanger BR (2004) The open peritoneal cavity: etiology correlates with the likelihood of fascial closure. Am Surg 70(7): 652-656.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...