
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Does Covid 19 have a role in Pneumatosis Cystoides Intestinalis? Volume 7 - Issue 2
Sinan Ömeroğlu*, Onur Güven, Uygar Demir and Elif Baran
- Department of General Surgery, University of Health Sciences, Sisli Hamidiye Etfal Research and Training Hospital, Istanbul, Turkey
Received:November 14, 2022; Published:November 29, 2022
Corresponding author: Sinan Ömeroğlu, Department of General Surgery, University of Health Sciences, Sisli Hamidiye Etfal Research and Training Hospital, Istanbul, Turkey
DOI: 10.32474/SCSOAJ.2022.07.000257
Abstract
Pneumatosis cystoides intestinalis is a rare disease and can be diagnosed in patients who are asymptomatic or with gastrointestinal symptoms. Gastrointestinal symptoms were reported in 17.6% of patients diagnosed with Covid-19. There are many factors in the etiology of pneumatosis cystoides intestinalis, SARS-CoV-2 is also one of the infectious agents. Currently, the treatment is based on a conservative approach unless there is an acute abdomen. We aimed to present the life-threatening clinic in two Covid-19 positive patients diagnosed with pneumatosis cystoides intestinalis.
Keywords: Pneumatosis Cystoides Intestinalis; Pneumoperitoneum; Covid 19
Introduction
Pneumatosis Cystoides Intestinalis (PCI) is a rare disease characterized by the presence of gas-filled cysts within the submucosa or subserosa of the intestinal wall [1]. Its incidence is approximately 0.03% [2]. Two theories stand out in pathophysiology, mechanical and bacterial. Mechanical theory includes the migration of gas to the intestinal wall due to mucosal disruption, increased mucosal permeability and increased transabdominal/intraluminal pressure. Bacterial theory includes bacteria that penetrate the gastrointestinal mucosa/submucosa and bacterial gut microbiota which converts carbohydrates/other nutrients into hydrogen gas [3]. PCI may be idiopathic or secondary to pulmonary/gastrointestinal motility/ immunological disorders, mucosal disruption, malignancies, infections, iatrogenic causes and intra-abdominal complications [4]. Clinically, PCI can be diagnosed in patients who are asymptomatic or which have gastrointestinal symptoms. On radiological examination, it is characterized by welldemarcated cysts within the walls of hollow gastrointestinal organs and small-volume pneumoperitoneum may be presented. PCI can be localized as segmental or diffuse [5]. Asymptomatic patients do not require treatment, for mild and moderate cases conservative therapy including antibiotics and oxygen is recommended. Patients with refractory symptoms and intra-abdominal complications surgery should be considered [3]. Infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes coronavirus disease 2019 (Covid-19). Gastrointestinal symptoms were reported in 17.6% of patients diagnosed with Covid-19 in studies [6]. We aimed to present the life-threatening clinic in two Covid-19 positive patients diagnosed with pneumatosis cystoides intestinalis.
Case 1
A 28-year-old female patient was hospitalized in the Covid-19 pandemic clinic with diarrhea, vomiting, abdominal pain symptoms. She had a history of acute lymphocytic leukemia and bone marrow transplantation six months ago and after transplantation she received three cycles of chemotherapy. She was vaccinated with two doses of the Pfizer-BioNTech vaccine. Stool examination was negative for bacterial or parasitic infections for diarrhea. Conservative therapy was continued with the recommendations of the infectious diseases clinic. Contrast-enhanced abdominal tomography was performed on the patient after ten days, when symptoms persisted, abdominal pain increased, and acute abdomen was found on physical examination. There was air in the wall of the large intestine from the cecum to the rectum in the computed tomography. Diagnostic laparoscopy was performed. There was no intestinal perforation or ischemia. She had diffuse involvement pneumatosis cystoides intestinalis with in the wall of colon and nothing was done (Figure 1). The patient was taken to the Covid 19 intensive care unit. She died on the 5th postoperative day due to pulmonary complications secondary to Covid 19.
Case 2
A 49-year-old male patient was applied to the emergency with new onset abdominal pain. He had a history of endoscopic balloon dilatation for pyloric stenosis ten years ago and had been using prednisone for three years with the diagnosis of rheumatoid arthritis. He was on the 7th day of home quarantine after being asymptomatic Covid 19 positive and was not vaccinated. Physical examination was compatible with acute abdomen. Contrastenhanced abdominal tomography was performed. There was free air in abdomen and the wall of the segmental small intestine (Figure 2). Explorative laparotomy was performed. Pneumatosis cystoides intestinalis was present with segmental involvement of the ileum and jejunum (Figure 3). Intestinal perforation, ischemia or any gastrointestinal complications were not observed then the surgery was terminated. On the 10th postoperative day, the patient was discharged without complications after medical treatment containing antibiotics in the general surgery clinic.
Figure 2: Computed Tomography image, free air in abdomen and the wall of the segmental small intestine.
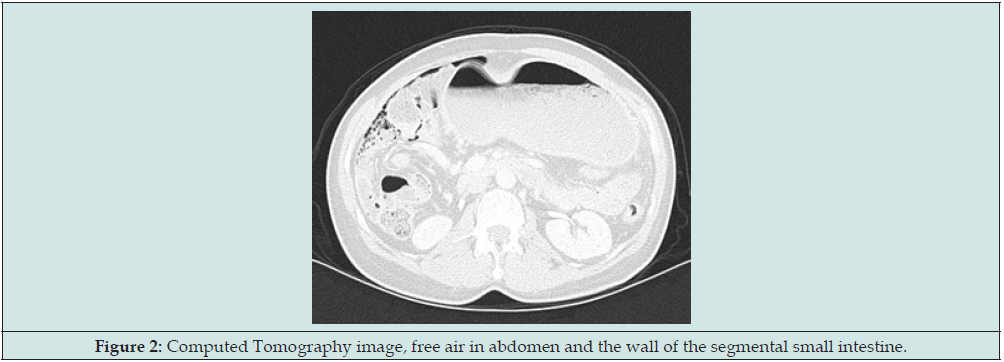
Figure 3: Pneumatosis cystoides intestinalis presented with segmental involvement of the ileum and jejunum.

Discussion
Pneumatosis Cystoides Intestinalis (PCI) is an uncommon disease. Although some conditions and predisposing factors have been defined in the etiology, 15% of cases are reported as idiopathic [1-3]. SARS-CoV-2 affects many organs throughout the human body. Gastrointestinal symptoms are reported in 10-15% of Covid-19 cases and include diarrhea, nausea, vomiting and abdominal pain [7]. PCI may be asymptomatic or may present with similar gastrointestinal symptoms. These two cases reveal that Covid 19 and PCI can coexisted and that Covid 19 may be one of the predisposing factors.
Suzuki et al. reported PCI in a patient treated with methotrexate for the diagnosis of rheumatoid arthritis [8]. Also, Iitsuka et al. reported PCI in a patient who started steroid treatment due to nephrotic syndrome [9]. In 1969, Crider described PCI in a patient with chronic lymphocytic leukemia [10]. Nobori, et al. defined asymptomatic PCI after one hundred and fifteen days later in patient who underwent hematopoietic stem cell transplantation for lymphoma and was given steroids for acute skin graft versus host disease [11]. Additionally, PCI cases have been reported in lymphoma patients receiving chemotherapy, especially asymptomatic [12]. Similar to the literature, our patients have leukemia, bone marrow transplant, rheumatoid arthritis, chemotherapy and steroid use which are classified as malignancy, immunological disturbance and iatrogenic conditions in etiology. Differently, both of our cases were Covid 19 positive. Treatment in PCI is based on clinical condition and severity of symptoms. According to the literature, for mild and moderate cases conservative therapy including antibiotics and oxygen are suitable. Surgery is recommended in patients with persistent symptoms and suspected intra-abdominal complications [3]. We preferred surgery because of refractory symptoms or acute abdomen sign on physical examination.
Conclusion
Pneumatosis cystoides intestinalis is an uncommon disease. Although there are many factors in the etiology, SARS-CoV-2 is also among the infectious agents. Currently , the treatment is based on a conservative approach.
References
- Wu LL, Yang YS, Dou Y, Liu QS (2013) A systematic analysis of pneumatosis cystoids intestinalis. World J Gastroenterol 19(30): 4973-4978.
- Wang Yj, Wang Ym, Zheng Ym, Jiang Hq, Zhang J (2018) Pneumatosis cystoides intestinalis: six case reports and a review of the literature. BMC Gastroenterol 18: 100.
- Alpuim Costa D, Modas Daniel P, Vieira Branco J (2021) The role of hyperbaric oxygen therapy in pneumatosis cystoides intestinalis – A scoping review. Front Med (Lausanne) 8: 601872.
- Koss LG (1952) Abdominal gas cysts (pneumatosis cystoides intestinorum hominis); an analysis with a report of a case and a critical review of the literature. AMA Arch Pathol 53(6): 523-549.
- Hocking J, Bell D (2011) Pneumatosis cystoides intestinalis. World J Gastroenterol 17(44): 4932–4936.
- Cheung KS, Hung IFN, Chan PPY, Lung KC, Tso E, et al. (2020) Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from a Hong Kong cohort: Systematic review and meta-analysis. Gastroenterology 159(1): 81-95.
- Trypsteen W, Van Cleemput J, Snippenberg Wv, Gerlo S, Vandekerckhove L (2020) On the whereabouts of SARS-CoV-2 in the human body: A systematic review. PLoS Pathog 16(10): e1009037.
- Suzuki E, Kanno T, Hazama M, Kobayashi H, Watanabe H, et al. (2017) Four cases of pneumatosis cystoides intestinalis complicated by connective tissue diseases. Intern Med 56(9): 1101-1106.
- Iitsuka T, Kobayashi M, Izumi Y, Koyama A (1993) [Pneumatosis cystoides intestinalis following steroid treatment in a nephrotic syndrome patient: report of a case]. Nihon Jinzo Gakkai Shi 35(3): 293-297.
- Crider RJ, Bentlif P (1969) Pneumatosis cystoides intestinalis: The report of a case associated with severe pulmonary disease and chronic lymphocytic leukemia. Henry Ford Hospital Medical Journal 17(4): 285-294.
- Nobori C, Aomatsu N, Uchima Y, Okada T, Miyamoto H, et al. (2017) Pneumatosis cystoides intestinalis after hematopoietic stem cell transplantation for malignant lymphoma - A case report. Gan To Kagaku Ryoho 44(12): 1402-1404.
- Patel RV, Sutton PA, Colliver D, Stewart R (2014) Pneumoperitoneum and pneumatosis cystoides intestinalis (PCI) following chemotherapy in an adolescent with Hodgkin's lymphoma. BMJ Case Rep 2014: bcr2013203433.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





