Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Research Article(ISSN: 2643-6760) 
Diagnostic Accuracy of RIPASA Scoring System in Presumptive Accurate Diagnosis of Acute Appendicitis: A Cross Sectional Study Volume 6 - Issue 4
Mehwish Mooghal1*, Wajiha Khan2, Shahid Mehmood Khan3, Lal Bux Brohi3, Asrar Ahmad4, Kamran Rahim4 and Mahwish Mahboob Bhutta1
- 1PNS Shifa hospital Karachi, Bahria University Medical and Dental College Karachi, Pakistan
- 2Student at Dow University of Health and Sciences Karachi, Pakistan
- 3Consultant General Surgery at PNS Shifa hospital Karachi, Bahira University Medical and Dental College Karachi, Pakistan
- 4Assistant Professor and Consultant Surgery, PNS Shifa Karachi, Bahria University Medical and Dental College Karachi, Pakistan
Received:December 11, 2021; Published:January 3, 2022
Corresponding author: Mehwish Mooghal, PNS Shifa hospital Karachi, Bahria University Medical and Dental College Karachi, Pakistan
DOI: 10.32474/SCSOAJ.2022.06.000244
Abstract
Introduction: The RIPASA scoring system of acute appendicitis was established specifically for Asian population, in view that its diagnostic dilemma will persist despite medical advancements and the financial constraints in developing world. Chong CF formulated RIPASA score both to reduce the diagnostic dilemma and have financial acceptance in resource limited regions, so the score can be implemented widely.
Objective: We conducted this study to address the diagnostic precision of RIPASA score in presumptive accurate diagnosis of acute appendicitis, taking histopathology as gold standard.
Materials and Methods: This Cross-Sectional study was conducted ata tertiary-care hospital over a period of 6 months (15th December 2019-15th June 2020). 141 patients of both genders with suspected signs/symptoms of acute appendicitis were included in study after taking consent. Patients underwent pre-inclusion assessment and scoring of patients according to RIPASA scoring scale was done. The decision for appendectomy was made on the basis of RIPASA score. Removed appendix samples were sent for histopathology.
Results: Among 141 patients, age range was15-50 years with mean age 30.191±6.09 years, and mean RIPASA score was 5.375±1.77. Majority of patients were males (58.9%). RIPASA score diagnosed 28(19.9%) and histopathology diagnosed 27(19.1%) patients of acute appendicitis. RIPASA score showed sensitivity of 85.2%, specificity 95.6%, diagnostic accuracy 94%, PPV 82.1% and NPV was 96.4%.
Conclusion: We concluded that RIPASA scoring system is the scoring system of choice in diagnosing acute appendicitis with good sensitivity and specificity. The results of study led us to consider that, this scoring system can be used as a routine assessment tool in acute appendicitis, as it is easy to apply and does not cost the patients an arm and a leg.
Keywords: Acute Appendicitis; Diagnosis; Histopathology; Negative Appendectomies; RIPASA Score
Introduction
Vermiform appendix has surgical importance as it tends to undergo inflammation and cause acute pain. Acute appendicitis is on top of the list producer of acute abdomen in adolescents &young adults, and appendectomy tops the most frequently performed surgical procedure by any surgeon [1]. Epidemiologic studies have showed that approximately 50% (13-77%) of the population will have appendicitis in their life time Butt MQ, et al. [7,8-11], with the peak incidence is in teens 20s, while it’s rare in infancy; risk of acute appendicitis decreases after middle age. Incidence is equal among males and females before puberty and increases to 3:2 at age 25, thereafter incidence declines in males. No cause is yet confirmed but the factors responsible can be decreased dietary fibers and increased consumption of refined carbohydrates, because incidence in developing countries is gradually increasing as they are adapting more western lifestyle Quartey B [4]. The diagnosis is basically clinical along with lab findings. Therefore, combined scoring system, comprising of both the clinical and lab findings, has devised to reduce negative appendectomy rates (15-25%) [5]. Most widely used scoring systems are Alvarado scoring system, PAS (Pediatric Appendicitis Score) as well as AIR (Appendicitis Inflammatory Response) score; however, RIPASA scoring system is a new development in recent years [6-8].
Raja Isteri Pengiran Anak Saleha Appendicitis (RIPASA) scoring system was established in 2008 peculiarly for Asian populations. Chong C F in the retrospective study consisting of 312 patients who had undergone an emergency appendectomy between October 2006 and May 2008 in Department of Surgery, Raja Isteri Pengiran Anak Saleha (RIPAS) Hospital, Brunei Darussalam, concluded that optimal cut-off threshold score for negative appendectomy was 7.5, with a sensitivity of 88%, a specificity of 67%, a Positive Predictive Value (PPV) of 93% and a Negative Predictive Value (NPV) of 53%. The negative appendectomy rate decreased significantly from 16.3% to 6.9%, which was a 9.4% reduction (p is 0.0007) [8]. Another study conducted by Butt MQ, et al. [3] at one of tertiary hospitals of Pakistan from sept 2011 to March 2012 showed that out of 267 patients, 152 positive cases were identified on histopathology while RIPASA diagnosed 152 cases. Overall, 147 were true positives, 8 were false positives, 5 were false negatives, and true negatives were 107. The sensitivity of score was found to be 96.7%, specificity 93.0%, Diagnostic Accuracy (DA) was 95.1%, PPV was 94.8% and NPV was 95.54% respectively [3]. There is scarce local data available on this topic in our region and internationally, so, the aim of our study is to evaluate the diagnostic authenticity of this new scoring system for presumptive accurate diagnosis of acute appendicitis by taking histopathology as gold standard. This study might be helpful in order to eliminate negative appendectomy rates in our local population by avoiding lavish investigations, keeping in consideration limited local facilities available for already overburdened healthcare system of our region.
Materials and Methods
This Cross-sectional study was conducted at the Surgery department of a tertiary care hospital in Karachi. The data was collected over a duration of six months from 15th December 2019 till 15th June 2020; using non- probability consecutive sampling technique. Our primary outcome measure was to assess applicability of RIPASA score in our population, and assessment of relation of secondary measures like age, gender, and socio-economic status with this score. By making use of sample size calculator for sensitivity and specificity by Dr. Lin Naig, statistics were found by taking: Sensitivity = 96.7%, Specificity = 93%, Prevalence of acute appendicitis = 50%, Margin of error for sensitivity = 4.2% and specificity = 6% [3]. The calculated sample size came out was 141.
Our Inclusion Criteria was
a) Genders: Male/Female
b) Age 15–50 years
c) Suspected cases presenting in emergency department within 48 hours of onset of pain right iliac fossa and VAS (visual analog scale) pain score ≥ 4 (score 1-3 = no to mild pain, score 3.1-6= mild to moderate pain, score 6.1-10= moderate to severe pain).
The Exclusion Criteria was
a) Patient with co-morbids (hypertension, ischemic heart disease, chronic liver disease, acute kidney injury, chronic kidney disease, diabetes)
b) Patients with history of appendectomy
c) Pregnant females
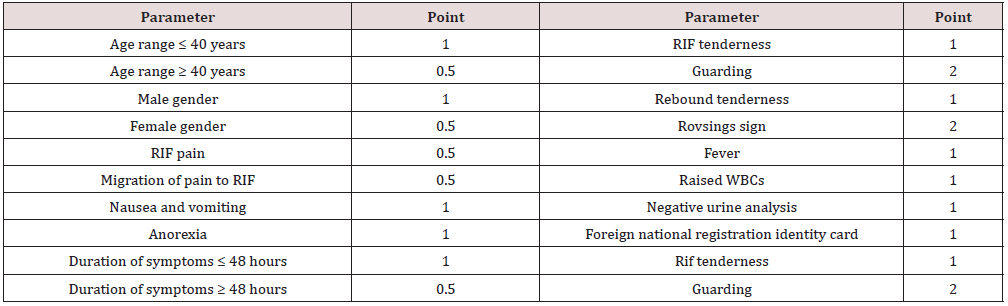
d) Diagnosed cases of appendicular abscess which were confirmed by (ultrasound and CT scan). The parameters of RIPASA scoring system are shown in Table 1 below:
The cut-off limit of 7.5 points was deemed as positive for acute appendicitis and used as a diagnostic tool in our study [8]. After approval by ethical review committee of our hospital, patients were selected after taking written informed consent prior to inclusion in study. Those patients presenting in emergency with pain right iliac fossa were included. Patients underwent detailed history, general and physical examination and scoring of patients according to RIPASA scoring scale and then decision of appendectomy was taken based on RIPASA score. Patients were observed by same researcher to exclude observer/interviewer bias. Patient’s particulars were noted, and a Performa was filled and attached with admission form. Removed appendix samples were sent for histopathology (Gold Standard), for confirmation of acute appendicitis. The data was analyzed using SPSS version 23. Mean and standard deviation was calculated for age and RIPASA score. Frequency and percentage were calculated for gender, education, findings on RIPASA and histopathology. 2×2 table was used to calculate sensitivity, specificity, PPV, NPV, diagnostic accuracy for RIPASA scoring system taking histopathology as gold standard. Effect modifiers like age, socio-economic status and gender were addressed through stratification. Post stratification Positive Predictive Value (PPV), Negative Predictive Value (NPV), Diagnostic Accuracy (DA), sensitivity and specificity were done.
Results
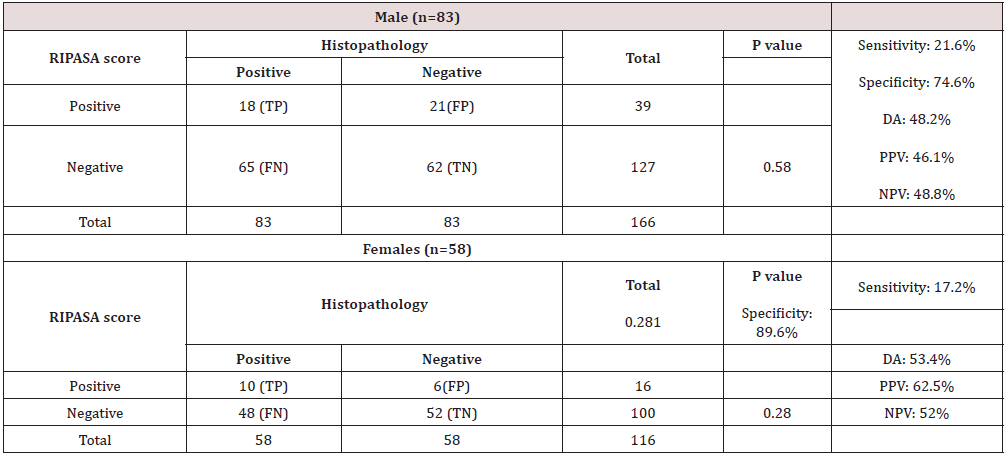
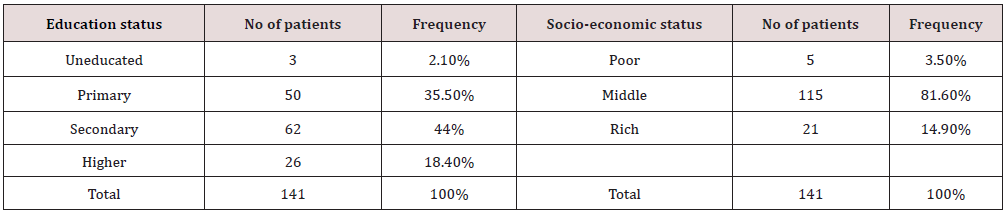
Total 141 patients included in the study. Age range in this study was from 15 to 50 years with mean age was 30.191±6.09 years and mean RIPASA score was 5.375±1.77. Majority of patients were males 83(58.9%). Percentages/frequency of patient’s presentation according to education and socio-economic status is shown in Table 2. Overall RIPASA score diagnosed 28(19.9%) and histopathology diagnosed 27(19.1%) patients with acute appendicitis. The negative appendectomies using RIPASA score was 113(80.1%) and on histopathology it was 114(80.9%). Table 3 shows comparison of RIPASA Score versus Histopathology for Acute Appendicitis. The sensitivity of results was 85.2%, specificity 95.6%; diagnostic accuracy 94%, PPV 82.1% and NPV was 96.4%. Stratification with respect to age among ranges (15-30 years) and (31-50 years) of RIPASA score versus histopathology is shown in Table 4. Stratification with respect to socioeconomic status (poor) of RIPASA score versus histopathology (n=5) shows p value = 1.00, Sensitivity: 20%, Specificity: 80%, DA= 50%, PPV= 50%, NPV= 50%. Stratification with respect to Socioeconomic status (middle) of RIPASA score versus histopathology (n=115) with p value = 0.737, Sensitivity: 20%, Specificity: 81.7%, DA= 50.9%, PPV= 52.2%, NPV= 50.5%. Stratification with respect to Socioeconomic status (rich) of RIPASA score versus histopathology (n=21), p value = 0.707, Sensitivity: 19%, Specificity: 76.1%, DA= 47.6%, PPV= 44.4%, NPV= 48.4%. Stratification with respect to gender (male/ female) of RIPASA score versus histopathology is shown in Table 5.
Table 2: Frequency/percentages of patient’s presentation according to education and socio-economic status.
Chi square = 89.55, P value = 0.000 (TP=true positive, FP=false positive, FN=false negative, TN=true negative).
Discussion
VAcute appendicitis being the main surgical crunch of ED for surgical residents/surgeons, needs due importance, as its prevalence demands correct diagnosis and prompt decision making in emergency departments to avoid unnecessary delays and sequelae of its delayed presentation in already pre-occupied emergency departments of the region.9In our study, overall sensitivity of RIPASA Score at a cut-off value of 7.5 come out to be 85.2%, specificity 95.6%, diagnostic accuracy 94%, PPV 82.1% and NPV 96.4% respectively. These results are reinforcing our confidence to use RIPASA score as an assessment tool in patient’s triage.
As already known, well timed arbitration is the need of time in suspected cases of acute appendicitis to bypass the risks of complications (peritonitis, perforation, sepsis). Weather to go for a surgical option or to plan conservative management, is the real enigma faced by a primary surgeon. Surgical removal of appendix in routine is not an answer to every case, rather many cases are seen to be managed conservatively on antibiotics alone; the protocol which is endorsed in many writings [10,11]. Another aspect of acute appendicitis is negative appendectomy, which is not just cumbersome for the patient only but also exhausts the healthcare resources [12]. For diagnosing the equivocal cases of acute appendicitis, ultrasounds and CT scans can provide an insight to make further plans [11,13,15]. Ultrasound being operant reliant, has variable degrees of reported specificities and sensitivities [11,14]. While the specificity of CT scan is around 84%, but it is at cost of rendering the patient exposed to radiation hazards and subjected high costs [15]. Therefore, none of the available diagnostic modalities can be labeled as ideal in decision making process in emergency settings, as they are not cost effective and easily available in all emergency set-ups of our region, with already limited resources [11]. The advent of Alvarado score to help diagnose acute appendicitis using pre-set clinical parameters, worked liked an appeal to surgeons, as it significantly reduced the rate of negative appendectomy overall. It was first forwarded in 1986, the system readily gained acceptance in surgical fraternity as it was a handy tool to make a presumptive diagnosis initially, but the system also reported high false positive results of acute appendicitis, particularly among females of fertile age group, so additional adjustments in score was proposed later on and presented as “modified Alvarado score” in 1994, which disqualified shifting of neutrophil to the left, 16 this further enhanced understanding of the system and cutback the false positive cases; but the said specificity and sensitivity of Alvarado system stood flat [17].
Likewise, same goes for scores like PAS score and AIR score [6,7]. Despite the fact that these scoring systems were applicable for population in rest of the world, in due course within surgical set-ups of Asia, it was observed that both Alvarado and modified Alvarado score were underprovided systems for functioning accurately in diagnosing acute appendicitis cases with reported low sensitivity and specificity [18,19]. Later in year 2010, Dr. Chong C F in his retrospective study, presented a new scoring system that could comprehend better to set apart ethnic groups with diverse dietary habits [19]. Consequently, RIPASA score was introduced for peoples with Asian ethnicity, with improved specificity and sensitivity of 85.7% & 96.2% respectively, for uncovering cases of acute appendicitis. This is to consider that, RIPASA score is now accepted widely and been tested for accuracy across multiple tertiary care set-ups in Pakistan and has revealed encouraging results [20]. Butt et al. [3] in his study has concluded the sensitivity of 96.7%, specificity 93.0% and DA95.1%of RIPASA score respectively.3 Our results also summarized the same profile as reported by Butt et al. [3]. Interestingly, the age range distribution is considerable for practicing surgeons, as most relevant age range for majority of presentations of acute appendicitis is in between teens and twenties [21] identical age group statistics(15-30yrs) is reported in our study, which further buttress the evidence that below par, erratic and unsafe dietary habits, which are more prevalent in this age group; perhaps contributes to the elevated prevalence of acute appendicitis in this alleged division of the people [21,22]. Likewise, observations proposed that majority of the false positive cases emerge from females of reproductive age group, amongst whom the symptoms of underlying primary pathology are masked due to mimicking symptoms of inflamed appendix, but primary cause is often identified intra-operatively; like ovarian cyst rupture/ovarian torsion, ectopic pregnancy [23,24]. Moreover, few studies reported false positive patients who falls among age group of 40–55years and are mainly diabetics& females, adding up another outlook to consider while managing patients of acute appendicitis and making differentials during assessment of patients, so the rate of negative appendectomy can be decreased [25,26]. The limitations of our study are multiple i.e.: small sample size, patients less than 15 and more than 50 years were not included in the study, high rate of negative appendectomies on histopathology results, non- inclusion of patients who presented after 48 hours of onset of symptoms, pregnant females and patients with co-morbidities were not included in this study. While having these pitfalls we cannot make our results applicable on all patients. However, our results supported the diagnostic effectiveness of RIPASA scoring system for majority of patients presenting to emergency departments, we believe that our research and results can provide an insight to future researchers to carry out more research work in this domain and formulate/modify the scoring systems of acute appendicitis, which are both surgeon friendly and financially cost effective.
Conclusion
By considering the results of our study we can put forward our recommendation that RIPASA scoring system can become the preferred scoring system for doctors working in ED. Not only it can aid in diagnosing acute appendicitis cases accurately with high specificity and sensitivity, but it also obviates the need to use expensive investigations. Moreover, it is supported that the patients presenting in age range of 15-30 years should be taken as highly suspicious and taken on low brink for diagnosis. Furthermore, careful assessment must be done before labeling acute appendicitis in women of fertile age group, so the number of false positive cases can be circumvented.
References
- Alvarado A (1986) A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med 15(5): 557-564.
- Quartey B (2012) Interval appendectomy in adults: A necessary evil? J Emerg Trauma Shock 5(3): 213-216.
- Butt MQ, Chatha SS, Ghumman AQ, Farooq M (2014) RIPASA score: A new diagnostic score for diagnosis of acute appendicitis. J Coll Physicians Surg Pak 24(12): 894-897.
- Arnbjornsson E (1983) Acute appendicitis and dietary fiber. Arch Surg 118(7): 868-870.
- Chan J, Fan KS, Mak TLA, Loh SY, Ng SWY, et al. (2020) Pre-operative imaging can reduce negative appendectomy rate in acute appendicitis. Ulster Med J 89(1): 25-28.
- Pogorelić Z, Rak S, Mrklić I, Jurić I (2015) Prospective validation of Alvarado score and Pediatric Appendicitis Score for the diagnosis of acute appendicitis in children. Pediatr Emerg Care 31(3): 164-168
- Pogorelić Z, Mihanović J, Ninčević S, Lukšić B, Elezović Baloević S, et al. (2021) Validity of Appendicitis Inflammatory Response Score in Distinguishing Perforated from Non-Perforated Appendicitis in Children. Children (Basel) 8(4): 309.
- Chong CF, Thien A, Mackie AJ, Tin AS, Tripathi S, et al. (2011) Comparison of RIPASA and Alvarado scores for the diagnosis of acute appendicitis. Singapore Med J 52(5): 340-345.
- Mohan D, Barnato AE, Rosengart MR, Farris C, Yealy DM, Switzer GE, et al. (2013) Trauma triage in the emergency departments of nontrauma centers: An analysis of individual physician caseload on triage patterns. J Trauma Acute Care Surg 74(6): 1541-157.
- Huston JM, Kao LS, Chang PK, Sanders JM, Buckman S, et al. (2017) Antibiotics vs. appendectomy for acute uncomplicated appendicitis in adults: Review of the evidence and future directions. Surg Infect (Larchmt) 18(5): 527-535.
- Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, et al. (2020) Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg15(1):
- Ambe PC (2019) Negative Appendectomy. It is Really Preventable? Journal of Investigative Surgery Taylor and Francis 32(5): 474-475.
- Mostbeck G, Adam EJ, Nielsen MB, Claudon M, Clevert D, et al. (2016) How to diagnose acute appendicitis: Ultrasound first. Insights Imaging 7(2): 255-263.
- Pinto F, Pinto A, Russo A, Cuppolino F, Bracale R, et al. (2013) Accuracy of ultrasonography in the diagnosis of acute appendicitis in adult patients: review of the literature. Crit Ultrasound J 5 Suppl 1(Suppl 1): S2.
- Kim DW, Suh CH, Yoon HM, Kim JR, Jung AY, et al. (2018) Visibility of normal appendix on CT, MRI, and sonography: A systematic review and meta-analysis. Am J Roentgenol 211(3): 140-150.
- Kalan M, Talbot D, Cunliffe WJ, Rich AJ (1994) Evaluation of the modified Alvarado score in the diagnosis of acute appendicitis: A prospective study. Ann R Coll Engl 76(6): 418-419.
- Díaz Barrientos CZ, Aquino González A, Heredia Montaño M, Navarro Tovar F, et al. (2018) The RIPASA score for the diagnosis of acute appendicitis: A comparison with the modified Alvarado score. Rev Gastroenterol Mex 83(2): 112-116.
- Noor S, Wahab A, Afridi G, Ullah K (2020) Comparing Ripasa Score and Alvarado Score In An Accurate Diagnosis Of Acute Appendicitis. J Ayub Med Coll Abbottabad 32(1): 38-41.
- Khan I, Ur Rehman A (2005) Application of Alvarado scoring system in diagnosis of acute appendicitis. J Ayub Med Coll Abbottabad 17(3): 41-44.
- Khan S, Usama M, Basir Y, Muhammad S, Jawad M, et al. (2020) Evaluation of Modified Alvarado, Ripasa and Lintula Scoring System As Diagnostic Tools For Acute Appendicitis. J Ayub Med Coll Abbottabad 32(1): 46-50.
- Sulu B (2012) Demographic and Epidemiologic Features of Acute Appendicitis. Append Collect Essays World Rij InTech pp. 169-178.
- Sartelli M, Baiocchi GL, Di Saverio S, Ferrara F, Labricciosa FM, et al. (2018) Appendicitis Worldwide (POSAW). World J Emerg Surg 16: 13:19
- Lopes Vendrami C, Xu X, McCarthy RJ, Shin JS, Goodhartz LA, et al. (2020) Body mass index as an indicator of the likelihood of ultrasound visualization of the appendix in pregnant women with suspicion of appendicitis. Abdom Radiol (NY) 45(9): 2637-2646.
- Kereshi B, Lee KS, Siewert B, Mortele KJ (2018) Clinical utility of magnetic resonance imaging in the evaluation of pregnant females with suspected acute appendicitis. Abdom Radiol (NY) 43(6): 1446-1455
- Tsai SH, Hsu CW, Chen SC, Lin YY, Chu SJ (2008) Complicated acute appendicitis in diabetic patients. Am J Surg 196(1): 34-39.
- Bach L, Donovan A, Loggins W, Thompson S, Richmond B (2016) Appendicitis in Diabetics: Predictors of Complications and Their Incidence. Am Surg 82(8): 753-758.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...