
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
Critical Ischemia of the Forefoot as Delayed Complication of a Posttraumatic Pseudoaneurysm of the Superficial Femoral Artery Volume 6 - Issue 5
Eliane von Klitzing1, Eberhard Grambow2, Katharina Kopetschke3, Ivan Dobroskok1 and Malte Weinrich1*
- 1Department for Vascular Medicine, DRK Kliniken Berlin Köpenick, Berlin, Germany
- 2Department of General, Visceral, Thoracic, Vascular and Transplantation Surgery, University Medicine Rostock, Rostock, Germany
- 3Department for Diagnostic and Interventional Radiology, DRK Kliniken Berlin Köpenick, Berlin, Germany
Received:June 2, 2022; Published:June 16, 2022
Corresponding author: Malte Weinrich, Department for Vascular Medicine, DRK Kliniken Berlin Köpenick, Berlin, Germany
DOI: 10.32474/SCSOAJ.2022.06.000249
Abstract
We present the rare case of a posttraumatic pseudoaneurysm of the proximal superficial artery with distal embolization years after an explosive trauma. Following emergency revascularization by thrombembolectomy the pseudoaneurysm was excluded with a covered stent graft by percutaneous intervention.
Keywords: Posttraumatic Pseudoaneurysm; Superficial Femoral Artery; Embolization; Covered Stent Graft
Introduction
Posttraumatic pseudoaneurysms of the superficial femoral artery presenting with distal embolization years after the initial trauma are a rare condition. We present the case of a patient with acute limb ischemia of the right forefoot after being injured by shrapnels years ago.
Case Report
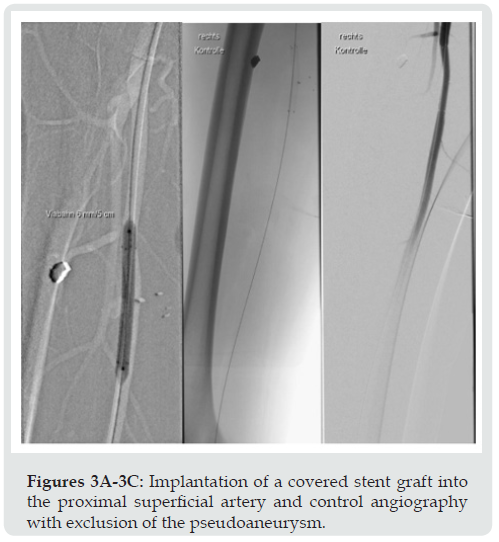
46-year-old otherwise healthy male presented to the emergency department complaining of a painful right forefoot since the previous day without history of recent trauma or injury. On physical examination the right forefoot was found to be pale, cold and aching without paresthesia or paralysis. With exception of the dorsal pedal artery all pulses of the right lower limb were palpable. The creatine kinase was slightly elevated. After being asked about the origin of several scars visible on the proximal right thigh, the patient reported of an injury from shrapnels in Syria years ago with shell splinters still remaining in the soft tissue. There was no history of atrial fibrillation or a coagulopathy. Due to the isolated occlusion of the dorsal pedal artery by duplex sonography performed by the vascular surgeon on call, fine needle angiography for more detailed visualization of the crural arteries was performed. As suspected, there was a distal occlusion of the anterior tibial artery as well as of the fibular artery and medial plantar artery. The posterior tibial artery was open. There were no aspects of abnormal atherosclerosis based on the patient’s age. Remarkably, a perfused pseudoaneurysm with a diameter of 8 mm located in the proximal superficial femoral artery as well as a large shell splinter close-by could be seen (Figure 1). The patient was transferred to the operating room and transpopliteal as well as transpedal thrombectomy of the crural and pedal arteries was performed. Due to pronounced vasospasm following thrombectomy intraarterial prostaglandin and fibrinolytic treatment was given (Figure 2). Postoperatively the patient was admitted to the intermediate care unit with continuous infusion of prostaglandin and heparin. Further diagnostics with longterm electrocardiography and transesophageal echocardiography revealed no other source for peripheral embolism, so we assumed the posttraumatic pseudoaneurysm as the source of peripheral arterial embolization. In a second step this pseudoaneurysm was excluded by percutaneous implantation of a covered stent graft (6 mm x 5 cm Viabahn: W.L. Gore) three days after surgery with access via the left common femoral artery (Figure 3). The patient was discharged nine days after admission fully recovered with palpable dorsal pedal artery and posterior tibial artery. Since the source of embolism was eliminated we stopped therapeutic anticoagulation in favor of dual inhibition of platelet aggregation following stenting of the superficial femoral artery.
Figure 1: Angiography showing the pseudoaneurysm of the proximal superficial artery and shell splinters within the soft tissue close-by.
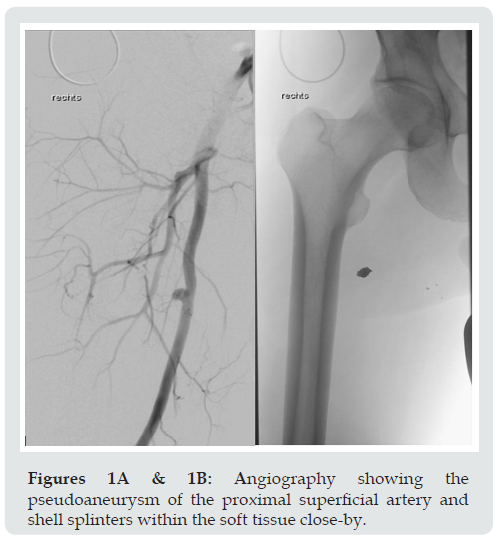
Figure 3: Implantation of a covered stent graft into the proximal superficial artery and control angiography with exclusion of the pseudoaneurysm.
Discussion
Pseudoaneurysms located in the proximal superficial femoral artery after vascular trauma does certainly not belong to the common sources of lower extremity embolism. Most commonly iatrogenic pseudoaneurysms occur in the common femoral artery following puncture or open reconstruction [1]. The clinical manifestations of femoral pseudoaneurysms are mainly pulsating masses, painful swelling and rupture leading to a potential life threatening situations whereas distal embolization leading to acute limb ischemia is unusual [1,2]. Furthermore, isolated aneurysms of the superficial femoral artery are rare [1]. Mostly they present as degenerative aneurysms in elderly men [2,3] more commonly leading to rupture (42%) than distal ischemia (13%) [1,2]. According to a systematic review of the literature performed by Ramakrishnan et al. there are only 13 cases published in the literature presenting delayed clinical manifestations of posttraumatic pseudoaneurysms of the lower limb arteries [4]. Due to the rare occurrence of isolated superficial femoral artery aneurysms, there are no guidelines available suggesting a specific aneurysm diameter and method for treatment. In general, long-term outcomes after surgical treatment of superficial femoral artery aneurysms are good with 5-year survival, limb salvage and graft patency rates of 62%, 88% and 85%, respectively [3]. Methods used were resection of the aneurysm with graft interposition, exclusion of the aneurysm with a femoropopliteal bypass and resection of the aneurysm and ligation only [3]. In our case we performed a two-stage approach by surgical thromembolectomy of the crural and pedal arteries and, secondarily, an endovascular repair with implantation of a covered stent graft three days after surgery. During the whole timeline we maintained therapeutic anticoagulation with heparin. Due to ongoing development of endovascular devices, endovascular repair of isolated superficial femoral artery aneurysms will become more prevalent [1].
Conclusion
A two-staged approach for acute limb ischemia following distal embolization out of a posttraumatic pseudoaneurysm of the superficial femoral artery is a proper way of vascular reconstruction. Similar cases should be reported to generate long-term data on the validity of this treatment method.
Conflicts of Interests
All authors declare no conflict of interests concerning the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/ or authorship of this article.
References
- Jacobowitz G (2019) Lower extremity aneurysms; in: Rutherford’s Vascular Surgery and Endovascular Therapy 83: 1078-1094.e3.
- Leon Jr LR, Taylor Z, Psalms SB, Mills Sr JL (2008) Degenerative aneurysms of the superficial femoral artery. Eur J Vasc Endovasc Surg 35(3): 332-340.
- Perini P, Jean-Baptiste E, Vezzosi M, Raynier JL, Mottini F, et al. (2014) Surgical management of isolated superficial femoral artery degenerative aneurysms. J Vasc Surg 59(1): 152-158.
- Ramakrishnan P, Vaswani P, Hote MP, Choudhary SK (2020) Delayed presentation of superficial femoral artery pseudoaneurysm 45 years following gunshot injury. Indian J Thorac Cardiovasc Surg 36(5): 526-529.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





