
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Research Article(ISSN: 2643-6760) 
Comparison of Replacement and Linear Plication with External Wrapping Surgical Treatment in Ascending Aortic Aneurysm Volume 6 - Issue 2
Mohammad Alsalaldeh*, A Vefa Özcan and Şafak Şimşek
- Department of Cardiovascular Surgery Pamukkale University, Faculty of Medicine Hospital Denizli, Turkey
Received: February 24, 2021 Published: March 05, 2021
Corresponding author: Mohammad Alsalaldeh, Department of Cardiovascular Surgery Pamukkale University, Faculty of Medicine Hospital Denizli, Turkey
DOI: 10.32474/SCSOAJ.2021.06.000233
Abstract
This study was planned to compare and evaluate the surgical technique of linear plication and external wrapping (LPEW) to graft replacement (GR) in tubular ascending aortic aneurysms. So, we sought to perform this study of those two surgical techniques to see the possibility to consider LPEW as an alternative surgical technique to graft replacement in well-selected patients with certain circumstances. Thus, energy potential of the biosystem is essence of physical health and his foundation, and people fall ill and prematurely die from the loss of health (energy potential). The problem of forming of new paradigm of health protection becomes actual.
Keywords: Health; illness; energy potential of the biosystem; paradoxes of medicine
Introduction
The main cause of death all over the world is still cardiovascular disease [1]. The aorta is the main, and the largest vessel in our body develops atherosclerosis as any other vessel. It is always under the highest pressure. The aneurysm is one of the aortic pathologies which may open the door to possible fatal results when it ruptures or becomes dissected. In aortic aneurysm cases, attention should be always taken to keep the aneurysm under control till its diameter reaches 55 mm in normal individuals, and 4.5mm in Marfan syndrome, or when the increasing rate in the size is more than 0.6/year. In that time surgery is required. On the other hand, if this aneurysm has been found dissected it should be managed surgically, and immediately without giving any concern to the size [2]. For a long time ago, many surgeons in many regions in this world tried several procedures to treat this type of aortic pathologies. In 1982 Robicsek did an aortoplasty by excising an oval segment of the aneurysmatic ascending aorta and replacing it with a well-tailored Dacron vascular graft [3]. Robicsek’s method had not been accepted by many surgeons. In 1956, it was the first time to treat ascending aortic aneurysm by replacement of a homograft under cardiopulmonary bypass and was done by Cooley [4]. Then, the replacement became more popular by using synthetic grafts. But the trials to find safer, and practical methods continued by many surgeons. In our center, we perform graft replacement for most of our patients with ascending aortic aneurysms as well as with whom with dissection or rupture. About ten years ago we started doing linear plication with the external wrapping for selected patients with ascending aortic aneurysm [5]. We have done forty-five operations with this technique. One of them was operated without using a cardiopulmonary bypass machine (off-pump) [6]. We had observed our patients for a long time and found it is the time to compare the results of all our patients who had undergone linear plication and external wrapping to the patient who had been operated on with graft replacement.
Material and Methods
Among the period of March 2009 to December 2019, 110 Patients were admitted to our department with ascending aortic aneurysms for surgical treatment. Only 65 patients were taken into our study who had not aortic dissection, rupture, aortic root dilatation, or any connective tissue disease, and all the aneurysms diameters were less than 60 mm. Some of them were presented with an isolated tubular ascending aortic aneurysm, and others had concomitant cardiac diseases such as coronary artery disease, aortic, mitral, or tricuspid valve diseases. Patients were divided into two groups, group one contained 66.2% (n=43) of the patients, and were operated on with the LPEW technique while group 2 contained 33.8% (n=22) of them, and were operated on with GR. All the operations were done by one surgeon. The age of all the patients at the time of operation showed two peaks, one at age 58, and the other at 70 years. The mean age of the patients in group 1 was 58.5 (min 24 – ma 81) years while in group 2 was 59.1 (min 25 – max 76) years. 69.2% (n=45) of the patients were males, and 30.8% (n=20) were females. The mean aortic diameter in all patients was 48.10 mm (48.44mm in group 1, and 47.45mm in group 2). CT-Scan with contrast was performed for all patients except 5 of them who had Magnetic resonance imaging (MRI) with contrast due to their renal impairment. All patients were checked for hemoglobin (Hb), leucocytes (WBC), creatinine, and an Ejection fraction of the left ventricle (LVEF) pre, and postoperatively. The data of Comorbidities like arterial blood hypertension (HTN), Diabetes mellitus (DM), Chronic obstructive pulmonary disease (COPD), and Chronic renal failure (CRF) were collected. Revision, follow-up period, and mortality were taken into consideration too. Patients who were selected to be operated on by linear plication and external wrapping were mostly elders with comorbidities such as chronic renal failure, chronic obstructive lung disease, and concomitant heart failure, and who may be affected negatively from long cardiopulmonary bypass, and cross-clamping time. On the other hand, we had young patients too whom we found suitable for LPEW. All the plication and wrapping operations were done after releasing cross-clamp (on beating heart) while graft replacement in group two was done under cross-clamp and cardiopulmonary bypass. In concomitant cardiac surgeries, the aneurysmatic or dilated ascending aorta was replaced by vascular graft or plicated and wrapped even if its diameter is still under the recommended size to prevent further operation or possible complications in the future. 17 patients were operated on for coronary artery disease with coronary artery bypass grafting (CABG), 9 patients were from the first group while 8 from the second. 48 patients were operated on with Aortic valve replacement (AVR), 33 of them were from the first group, and 13 from the second. 18 with mitral valve replacement (MVR), 15 of them were from the first group while 3 from the second. 5 patients were operated with tricuspid annuloplasty (TAP), 2 of them from first, and 3 from the second group. The decision of which technique to use was built upon the patient’s general condition, comorbidities, concomitant cardiac surgery, surgeon’s experience, and after discussing the technique with the patients, and their relatives.
Surgical technique
Figure 1: a) After the graft has been prepared it is passed under the aorta to let its short curvature sit on the upper border of the aorta. b) The final view of LPEW.
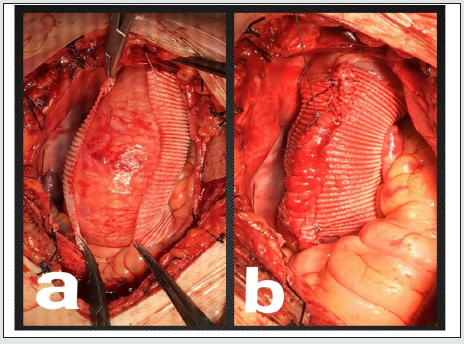
The first group of patients was operated by linear plication and external wrapping technique. In this technique, after sternotomy, the pericardium is opened vertically under full heparinization. In cases of concomitant cardiac surgery such as aortic failure or stenosis aortic, venous, and right superior pulmonary vein cannulations are done traditionally with taking caution to keep the aortic cannula at the farthest point of ascending aorta, and after passing through the cardiopulmonary bypass, cross-clamp is applied on the distal part of the aorta priorly to the aortic cannula. The cardioplegic solution is given directly via coronary ostiums every 20 minutes after aortotomy. After replacement of the aortic valve, de-airing, and closure of the aortotomy are done, then the aortic cross-clamp is removed. In MVR aorto-bicaval cannulation is done, and the mitral valve is replaced as usual. In the CABG operations, distal, and proximal coronary graft anastomosis is done as usual then crossclamp is removed from distal aorta blood pressure is maintained to be around at the acceptable minimum (systole 60-80 mmHg). A straight side vascular clamp is applied to the anterior right side of the ascending aorta (at 2 o’clock) longitudinally from the sinus of Valsalva to the beginning of the innominate artery keeping an acceptable diameter size (28-29 mm) under it after cleaning aorta from pericardial reflections, and any connected tissues. A 30 -32 mm Dacron graft with suitable length is prepared by cutting it longitudinally after bringing it into a trapezoid shape. Then the graft is passed under the aorta to let its short curvature sit on the upper border of the aorta (Figure 1a). The two edges of the graft are sewn underneath the straight clamp through the plicated zone in ‘U’ shape suturing style by using 4/0 polypropylene sutures. A straight clamp is released. A 2/0 polyester suture is used in suturing the graft edges with the plication zone in continuous style (Figure 1b). The proximal, and distal edges of the graft are fixated to the anterior adventitia of the aorta by 5/0 polyproline sutures to prevent graft immigration. In CABG cases the graft is prepared previously to allow the passage of the proximal graft through it. Then decannulation is done traditionally.
Surgical technique in group 2 patients, who had undergone graft replacement: aortic, venous, and right pulmonary artery cannulations are typically done as it is in group one. Cross clamp is applied to the distal part of the ascending aorta priorly to the aortic cannula, and resection of the aneurysmatic segment is done. The cardioplegic solution is given directly via both coronary ostiums every 20 minutes. Temperature is decreased downward to 28 C, and the replacement is done by using 26- or 28-mm Dacron grafts. Proximal anastomoses are done firstly followed by anastomosing the distal part (Figure 2). After finishing distal anastomosis deairing is done carefully, and the cross-clamp is released. Body temperature is increased gradually till normal value. The aneurysm that extended to the arch were excluded from our study. At the end of all operations, all the patients were taken to the cardiac surgery intensive care unit (ICU) where they were observed and monitored closely. We had a single case of a patient who had isolated tubular ascending aortic aneurysm with no other cardiac pathologies, but he had a family history of ascending aortic aneurysm rupture that he was operated by linear plication and external wrapping with offpump technique [6]. Postoperatively the patients were transferred firstly to the cardiovascular intensive care unit for one or a few days till their vital signs become stable, and re-fit to be transferred to the floor. All patients were followed up on the floor after had been transferred from ICU with the daily physical examination, dressing, imaging, and blood investigations. Post-discharge, the patients were followed up as an outpatient in our cardiac surgery clinics. the average follows up time for group 1 was 18.2 months (min 2 – max 60 months), and it was 19.9 months (min 0 – 63 months) for group 2 patients.
Statistical analysis
Continuous variables mean ± st, standard deviation, range (minimum-maximum); categorical variables were shown as numbers and percentages. The significance test of the difference between the two groups was done by using a compare independent test (Levene’s Test for Equality of Variances, and t-test for Equality of Means). p<0.05 was considered a statistically significant value. Data SPSS Version 21.0 Armonk, NY: IBM Corp
Results
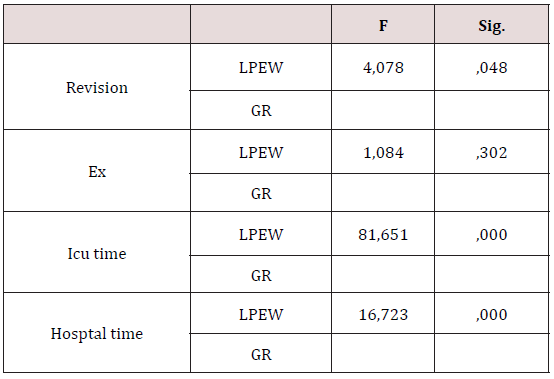
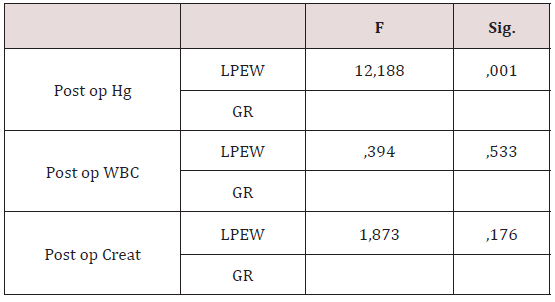
5 patients had revision for bleeding postoperatively, 1 of them was from group one, and 4 from group two. 1 patient from group one, and 3 from group two died on the same day of the operation or the following few days. There were no significant differences between the two groups in terms of mortality while there was a significant difference in revision (P=0.048) that there were 4 cases of revision in each group. Stayment period in the intensive care unit (ICU) (P=0.000), and at the hospital (P=0.000) showed significant differences (Table 1), and post-op hemoglobin value too (P=0.001) (Table 2) which was due to less bleeding i group one postoperatively.
Table 1: Comparing revision and mortality in the two groups.
ND: Not Detected; c.HGVS: Description of Coding DNA (c.) HGVS: variants by Human Genome Variation Society; p.HGVS, description of protein (p.) variants by HGVS. *describe a stop codon.
Table 2: Comparing lab test in the two groups.
ND: Not Detected; c.HGVS: Description of Coding DNA (c.) HGVS: variants by Human Genome Variation Society; p.HGVS, description of protein (p.) variants by HGVS. *describe a stop codon.
Discussion
Ascending aortic pathologies carry a high risk of mortality. Aneurysm of the aorta is considered as the pre dissection or rupture stage where the aortic diameter becomes more than one, and half of its normal average [7]. The pathogenesis of aneurysms had been suggested by many theories. Basically, in the pathophysiology of the aneurysm, cystic medial degeneration plays the main role. The elastin degeneration in the aortic wall goes side by side with proteoglycan accumulation, and smooth muscle cell loss [8]. According to Laplace law, the increase of the aortic diameter leads to an increase in the stress at the entire wall which increases vessel wall remodelling, and dilatation [7]. In this study, we tried to review our experience of the linear plication and external wrapping surgical technique in ascending aortic aneurysm management. We compared LPEW to the traditional surgical treatment method graft replacement. All the operations of our patients who were included in this study were done by two surgeons. The decision of the operation technique type was taken according to the ascending aortic aneurysm’s size, type, extension, patient’s other cardiac pathologies, and general condition. We kept in mind as a rule that any aneurysm which will be managed by linear plication, and external wrapping should not exceed 60 mm in diameter that, in general, aneurysms larger than 60mm have a very thin wall, and are not suitable for plication. Also, the aneurysm should not extend upward to the arch or downward to the sinus of the Valsalva. Any patient with acute or chronic dissection or has connective tissue disease such as Marfan syndrome is not a candidate for such a procedure. Most of the patients who were operated by this technique were in advanced age with comorbidities such as chronic renal failure, obstructive lung disease, or have low ejection fraction that may not be able to tolerate long cardiopulmonary bypass or cross-clamp time. In general, the procedure of LPEW is taking about 20-25 minutes.
During analysing the data, we have not found significant differences between the two groups in terms of costs clamp, and CPB time, we refer that result to the concomitant cardiac procedures. In fact, similar alternative surgical treatment methods were tried before but not as same as our technique. In the 1982- year Robicsek had operated on 6 patients by using the technique of aortoplasty (excision of an oval segment of the aortic wall) with external wrapping by a well-toiled dacron graft, he noticed that the procedure was not difficult, and the patients were doing well postoperatively. That technique was not accepted by many surgeons and became a historical method of treatment [4]. In 2003, Matthias Bauer et al reported a case of dislocation of an aortic wrap. The patient in that case had undergone aortic valve replacement, and aortoplasty with external wrapping by a Dacron graft 4 years priorly. The second operation was for coronary artery disease. Intraoperatively severe rarefaction of the aortic wall was found due to the dislocation of the wrap [9]. We usually prevent such complications by fixation of the proximal, and distal edges of the graft to the anterior adventitia of the aorta by 5/0 polypropylene sutures. To answer the question of the aortoplasty as an alternative surgical treatment to the traditional replacement in the patients with ascending aortic aneurysms Michael Gill et al. had published a report in 2009. In that report, there were 13 papers from potential 925 papers about aortoplasty of ascending aortic aneurysm. As a result, they found that there were only 25 (3%) patients suffered from re-dilatation during follow up. They noticed that the wrapping technique is not an innocent technique that carries the risk of dislocation, erosion, and fistula formation [10]. In our study, the technique of linear plication was done by plicating the aorta under low arterial pressure to keep an acceptable aortic diameter without excision any segment of the aortic wall. On the other h, and our external wrapping was done by giving the Dacron graft a shape suitable to the aortic major, and minor curvatures, and was fixated from its proximal, and distal edges to the adventitia of the aorta to prevent any possibility of dislocation. Our ten years follow-up does not show any late complications such as dislocation, erosion, or fistula formation.
We compared the LPEW technique in 43 patients to the traditional GR technique in 22 patients after excluded any patient with acute or chronic dissection, aneurysmatic diameter more than 60mm, or had aortic root dilatation or aneurysmatic sinus of Valsalva, also any aneurysm extended to the arcus aorta was excluded too. Patients with connective tissue diseases as Marfan syndrome were not operated on by LPEW at all. We analysed the data of all patients pre, and postoperatively in terms of blood investigations (hemoglobin, leukocytes, and creatinine), revision, mortality, ICU, hospitalization, CPB, and cross-clamp time. There was no significant difference between the two techniques in terms of mortality, but there were significant differences when we compare the need for revision. The ICU, and hospital staying time was found to be shorter in the LPEW technique. According to postoperative hemoglobin values obtained from both groups of patients, there was a significant difference that the higher hemoglobin was in group one, which shows the blood loss in the LPEW technique is lesser than it is in the GR technique. At the beginning of this study, we suggested that there will be a significant difference in creatinine values when the two groups will be compared but the statistical analysis showed that there is no significant difference. We had one case of LPEW that the operation was done without CPB (off-pump) where the patient had isolated tubular ascending aortic aneurysm which shows the possibility to do such operation without CPB with good results.
Conclusion
Even the GR surgical technique is still the ST, standard treatment method of ascending aortic aneurysms, LPEW can be considered as an alternative surgical treatment method and can be done safely with good results in well-selected patients with less need for revision, and blood transfusion, and shorter time of ICU, and hospital statement. Further, and more comprehensive studies are still needed.
Ethics Committee Approval
had been taken on 26/06/2020 under the approval number (60116787-020/38223) from Pamukkale university-Faculty of Medicine / Ethics Committee / Denizli
Declaration of conflicting interests
The authors declared no conflicts of interest concerning the authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, and/or authorship of this article.
References
- Savoji H, Mohammadi MH, Rafatian N, Toroghi MK, Wang EY, et al. (2019) Cardiovascular disease models: a game changing paradigm in drug discovery, and screening. Biomaterials 198: 3-26.
- Hiratzka LF, Bakris GL, Beckmann JA (2010) ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/ SIR/STS/SVM guidelines for the diagnosis, and management of patients with thoracic aortic disease. J Am Coll Cardio 55(14): e27–e129.
- Robicsek F (1982) A new method to treat fusiform aneurysms of the ascending aorta associated with aortic valve disease: an alternative to radical resection. The Annals of thoracic surgery 34(1): 92-94.
- Cooley DA, DeBakey ME (1956) Resection of entire ascending aorta in fusiform aneurysm using cardiac bypass. J Am Med Assoc 162(12):1158–1159.
- Ozcan A V, Alşalaldeh M, Boysan, E, Goksin, I (2013) Ascending Aortic Aneurysm Treatment with Linear Plication, and External Wrapping Technique: Mid‐T erm Results. Journal of Cardiac Surgery Including Mechanical, and Biological Support for the Heart and Lungs 28(4): 421-426.
- Alşalaldeh M, Özcan AV (2019) Isolated Ascending Aortic Aneurysm Treated by Linear Plication, and External Wrapping Via Upper-J-Sternotomy Under Off Pump Technique. EC Cardiology 6: 01-04.
- Saliba E, Sia Y, Dore A, El Hamamsy I (2015) The ascending aortic aneurysm: When to intervene? IJC Heart & Vasculature 6: 91-100.
- El Hamamsy I, Yacoub MH (2009) Cellular, and molecular mechanisms of thoracic aortic aneurysms. Nature Reviews Cardiology 6(12): 771.
- Bauer M, Grauhan O, Hetzer R (2003) Dislocated wrap after previous reduction otoplasty causes erosion of the ascending aorta. The Annals of thoracic surgery 75(2): 583-584.
- Gill M, Dunning J (2009) Is reduction a ortoplasty (with or without external wrap) an acceptable alternative to replacement of the dilated ascending aorta? Interactive cardiovascular and thoracic surgery 9(4): 693-697.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





