Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Research Article(ISSN: 2643-6760) 
Bronchoscopic Management of Recurrent Tracheoesophageal Fistula in Children Volume 4 - Issue 4
Natasha L Vageriya*, Rasik Shah, Taha Daginawala and Prathamesh More
- Department of Pediatric Surgery, GGMC & Sir JJ hospital, India
Received: February 20, 2020; Published: March 03, 2020
Corresponding author: Rasik Shah, Department of Pediatric Surgery, GGMC & Sir JJ hospital, Byculla, Mumbai, India
DOI: 10.32474/SCSOAJ.2020.04.000195
Abstract
Objectives: To evaluate the results of bronchoscopic cauterisation of fistulous tract using bugbee electrode with or without injection of fibrin glue, for recurrent tracheoesophageal fistula (RTEF) in paediatric age group.
Methods: Retrospective analysis of patients of RTEF from 2004 to 2016 undergoing bronchoscopic management was performed. Four patients were identified and they were evaluated with respect to resolution of fistula, and their long-term outcomes.
Conclusion: Bronchoscopic cauterisation of fistula with bugbee diathermy along with application of fibrin glue if performed carefully can resolve RTEF. Author emphasises use of double lumen catheter for injection of fibrin glue and apnea during injection of glue as an important step to be strictly observed while performing bronchoscopic management of RTEF.
Keywords: Recurrent, TEF, Fibrin Glue, Bugbee diathermy
Introduction
Oesophageal atresia and TEF has an overall incidence of 1 in 3000 to 4500 live births. It is one of the most challenging congenital anomalies because of its high morbidity and mortality [1]. RTEF occurs in 5%-15% of patients following oesophageal atresia repair [2]. Re-thoracotomy is technically challenging, and it is associated with significant morbidity, including a re-fistulation rate of 10%- 22% [2]. As per literature Endoscopic occlusion of the RTEF with tissue adhesives (fibrin glue, Histoacryl) is reported to be safe and highly effective [2]. Till date only 99 such cases of endoscopic attempts to close RTEF in children are published. Of these, majority was approached from oesophageal side and only few cases of bronchoscopic management have been described.
Materials and Methods
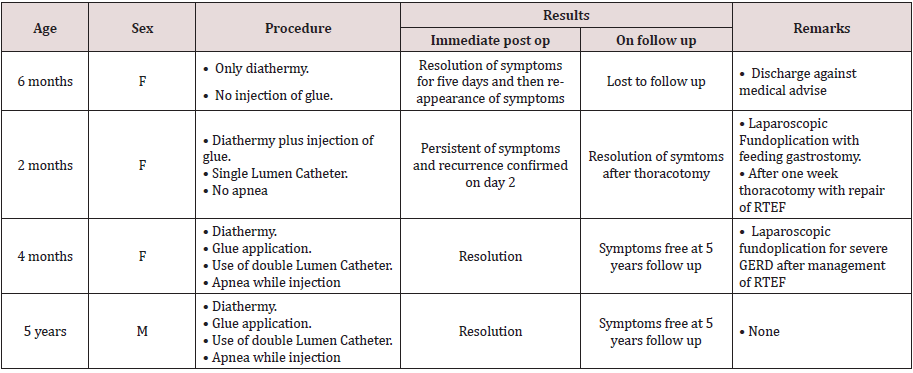
We did a retrospective analysis of all the patients having RTEF after initial repair of congenital type of TEF. From 2004 to 2016 four such patients were identified. Out of these 3 were females and 1 patient was male. These patients were subjected to evaluation by bronchoscopy along with definitive management in the form of diathermy of fistula by monopolar electrode (bugbee) and then injection of fibrin glue. These patients were then evaluated in the immediate postoperative period and then they were on long term follow up for their outcomes (Table 1).
Technique
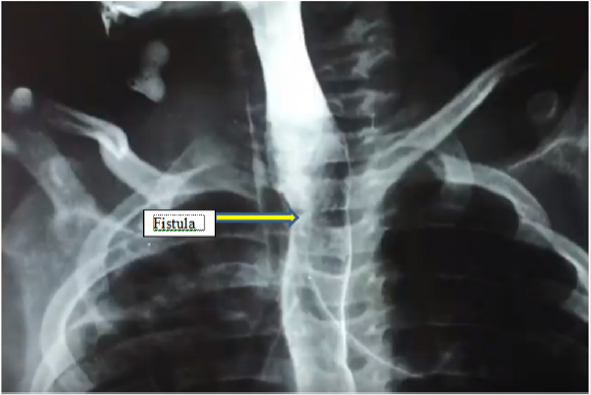
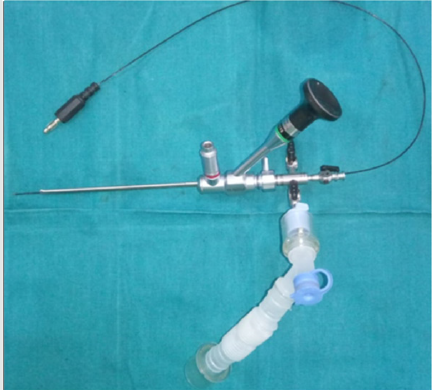
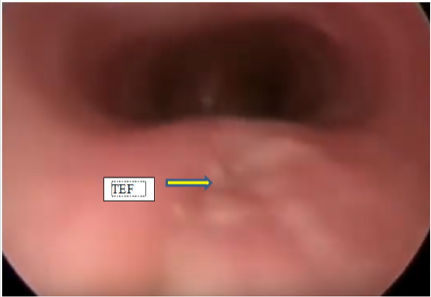
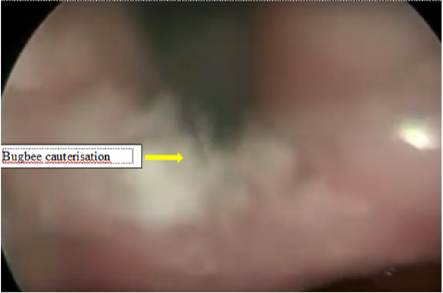
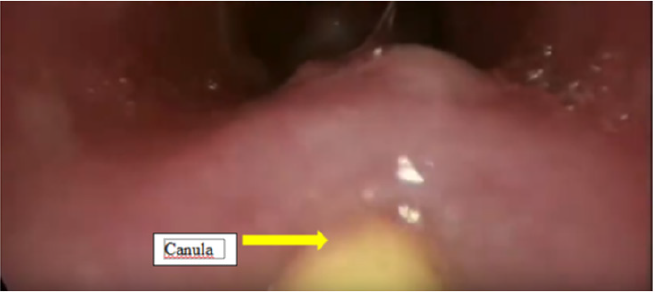
All the patients after the repair of TEF had either persistent or recurrent lower respiratory tract infections. They underwent water soluble contrast oesophagogram, which confirmed presence of RTEF(Figure1). Then these patients were subjected to the therapeutic bronchoscopy. All procedures were done under general anaesthesia with patients paralysed. An 8.5 Fr integrated cystoscope was used in infants and larger size 13 Fr cystoscope was used in a five-year-old patient. The cystoscope was introduced into the trachea under guidance of laryngoscope. These patients were ventilated through the side channel of bronchscope (Figure 2) Bronchoscopy showed a presence of fistula just proximal to carina in three patients and at a distance of 2 cm from carina in one patient (Figure 3). Then the bugbee electrode was placed through instrument channel of the cystoscope and tip of the bug bee was just introduced into the fistula. The monoploar diathermy at lower setting of 5-15 was applied and the mucosal lining of the RTEF was cauterized (Figure 4). Then the bugbee was withdrawn along with the scope. The double lumen catheter, which was to be used for injection of glue, was primed and then it was introduced into the trachea. Then by the side of this catheter scope was introduced under the guidance of direct laryngoscopy. The tip of this double lumen catheter was carefully manipulated into the opening of RTEF on tracheal side (Figure 5). Anaesthetists were informed to give apnea and 0.2 to 0.4 ml of glue was injected. After injecting it takes approximately 4 seconds for fibrin glue to solidify. The scope was then negotiated beyond RTEF and gentle ventilation was carried out for few minutes. The scope was finally withdrawn.
Post procedure all patients were fed through a nasogastric tube
for first two days. Patients underwent contrast swallow study to
evaluate status of RTEF. If RTEF was resolved, then the oral feeding
was resumed and patients were discharged. All patients received
per-operative antibiotics along with proton pump inhibitors.
A. Case 1: A 6 months old female child, who was operated at
day 2 of life for congenital TEF with open thoracotomy and ligation
of fistula with primary anastomosis, presented with complaints
of recurrent lower respiratory tract infection (LRTI) with failure
to gain weight. A contrast swallow study was carried out which
confirmed a RTEF. She underwent a bronchoscopic evaluation of
fistula with only cauterisation of same. Nasogastric tube was kept
for two days and feeding was continued through it. Then a dye
study was done, which did not demonstrate any fistula and she
was started on oral feeds. Patient was clinically alright till fifth day
postoperatively when she developed LRTI. A repeat dye study at
this time showed a persistent fistula and was advised thoracotomy
and ligation of same. But the parents did not agree for same and
took discharge against medical advice. She was then lost to follow
up since then.
B. Case 2: A two-month-old female child was admitted for
pneumonia. She had undergone repair of congenital TEF at day 1
of life. Since 20 days after surgery child had been re-admitted for
severe LRTI and then transferred to our institute. On investigating
she was found to have a recurrent TEF on contrast study. She
was then subjected to bronchoscopic evaluation along with
cauterisation and fibrin glue injection by above technique. But
only single lumen catheter was used; also, the ventilation was not
withheld during injection. So, the proper injection was not achieved.
In the postoperative period after 2 days a repeat contrast study
showed persistence of fistula. She then underwent a laparoscopic
fundoplication with a feeding gastrostomy to prevent reflux and for
feeding. Seven days later a thoracotomy with ligation and division
of fistula was done. After 5 days of this procedure contrast study
showed resolution of fistula. Oral feeds were then started. Patient
was on regular follow up, gaining weight and taking oral feeds
adequately. At 6 years closure of persistent gastrocutaneous fistula
was done.
C. Case 3: A 4months old female child was brought with
complaints of failure to gain weight with recurrent LRTI. She was
operated on day 2 of life for congenital TEF by thoracotomy and
ligation of fistula with primary anastomosis. A contrast study
confirmed a RTEF. She then underwent bronchoscopic procedure
with diathermy cauterisation with glue application by the technique
as mentioned. This time a double lumen cannula was used, and the
ventilation was withheld during the procedure. A nasogastric tube
was kept, and child fed through it for two days. Dye study after2
days showed no fistula. Patient was then started on oral diet. On
follow up patient had symptoms of severe gastroesophageal reflux
disease. She then underwent a laparoscopic fundoplication after
which she had complete resolution of symptoms. She has been on
regular follow up and has no recurrence on follow up even after 5
years.
D. Case 4: A 5-year-old boy presented with complaints of
failure to gain weight and recurrent LRTI since 1 year age. He had
undergone thoracotomy on day three of life for congenital TEF. On
thorough evaluation; contrast swallow dye study demonstrated
a recurrent TEF. He underwent bronchoscopy with a 13 French
bronchoscope and diathermy cauterisation along with fibrin glue
application as per the technique as mentioned earlier. Two days
later dye study showed resolution and child was started on full
feeds. He is on yearly follow up since then and has no recurrence
even after 5 years (Table 1).
Discussion
After primary repair of oesophageal atresia and TEF, reported
incidence of RTEF is 5-15 % [1,2]. RTEF present with chronic
cough, cough associated with ingestion of food which is also known
as Ohno’s sign [3], episodes of choking and /or cyanosis associated
with ingestion of food, recurrent pneumonia, chronic lung disease
and malnutrition should lead to diagnostic suspicion [1]. The
diagnosis of RTEF can be confirmed by contrast swallow study or
by HRCT (high resolution Computed tomorised scans). However,
diagnostic bronchoscopy is the choice of investigation for diagnosis
and it can be converted into therapeutic procedure with help of
various techniques [1,2].
Although surgical re-explorations are the standard treatment
of RTEF; Endoscopic therapy offers a safe and elegant definitive
alternative. As per Richter et al and Tzifa et al some patients may
require repeated attempts of endoscopic therapy for successful
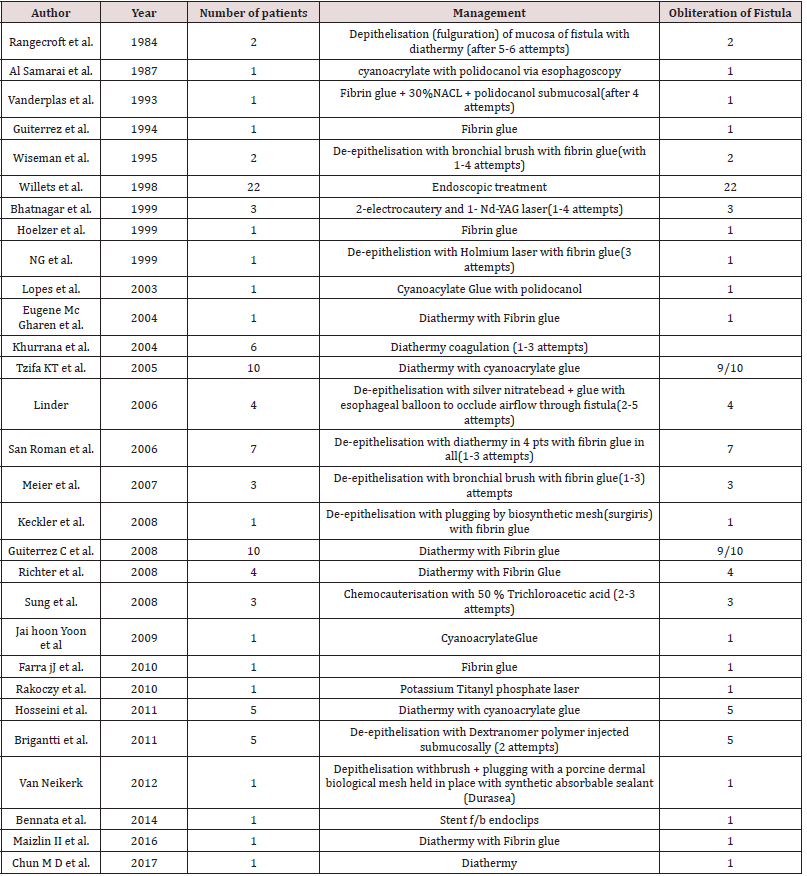
closure of RTEF [2]. Many techniques for endoscopic management
of RTEF have been described in children, the details of which are
illustrated in Table 2 and are self-explanatory [1,2,4].
As per R.K. Yellapu et al, glue and clipping are considered good
for
Authors on review of English literature have found only 99
children with RTEF, who have been managed by endoscopic
procedures till date (Table 2). Of these reported patients, majority
have been benefitted with help of diathermy along with application
of tissue adhesive glue. Majority of these patients were managed
esophagoscopically. On review of literature very few cases of
bronchoscopic management of RTEF have been reported. Authors
have reported 4 patients who developed RTEF after primary repair
TEF, which were managed bronchoscopically. Authors in first case
had reported use of diathermy alone, which lead to recurrence. In
second case, diathermy with injection of glue was carried out but
anaesthetists were not instructed to give apnea and glue flew off.
In second case, glue injection was carried out using single lumen
catheter which further complicates the procedure as there is a
possibility of glue to get solidified within the lumen of the catheter.
Authors, learning from the experience of first two patients,
improvised the procedure in the last two patients with use of a
double lumen catheter, where the two chemicals get mixed at the
tip of the catheter which is manipulated right at the mouth of fistula
and glue after injection solidify within seconds as chemical are
mixed. As patients were given apnea when the glue was injected,
it stayed at the site of RTEF and solidified. These two patients did
well in immediate postoperative period as well as on longer follow
up of 5 years. Authors recommend use of a double lumen catheter
and apnea during procedure as important steps in bronchoscopic
management of RTEF.
In endoscopic management of RTEF, use of fibrin glue or cyanoacrylate glue along with diathermy have been mainly described in literature. Gutierrez C reported 10 children with RTEF, who were subjected to bronchoscopy with the use of diathermy and fibrin glue injection. In 9 out of 10 patients, authors could achieve the complete obliteration of RTEF. Of these 5 patients required single session while 4 patients needed second attempt [1]. Fibrin glue (also called fibrin sealant) is a surgical formulation used to create a fibrin clot for hemostasis or wound healing. It is made up of fibrinogen (lyophilised pooled human concentrate) and thrombin (bovine, which is reconstituted with calcium chloride. When these two chemicals are mixed at the site of application it glues them together. Thrombin is an enzyme and converts fibrinogen into fibrin monomers within seconds, giving rise to a three-dimensional gel. There are multiple formulations available in market and in some aprotinin, fibronectin and plasminogen is also added [5,6]. The authors propose bronchoscopic cauterisation along with injection of fibrin glue by the technique described, as the first option to treat RTEF. If RTEF is resolved endoscopically then it can reduce morbidity significantly and it can also reduce the period of hospitalisation.
Conclusion
Authors propose bronchoscopic use of monopolar bugbee electrode for cauterisation followed by injection of fibrin glue on tracheal side of RTEF as a safe and effective method for managing RTEF. Endoscopic management of RTEF can reduce morbidity of the disease significantly.
References
- Upadhyaya VD, Gopal SC, Gangopadhyaya AN, Gupta DK, Sharma S, et al. (2007) Role of Fibrin Glue as a Sealant to Oesophageal Anastomosis in Cases of Congenital Esophageal Atresia with Tracheoesophageal Fistula. World Journal of Surgery (World J Surg) 31(12): 2412-2415.
- Willets Willetts IE, Dudley NE, Tam PK (1998) Endoscopic treatment of recurrent tracheo-oesophageal fistulae: long-term results. Pediatr Surg Int 13(4): 256-258.
- Yellapu RK, Gorthi JK, Kiranmayi Y, Sireesh I (2010) Endoscopic occlusion of idiopathic benign esophago-bronchial fistula Year. 56(4): 284-286.
- Richter GT, Ryckman F, Brown RL, Rutter MJ (2007) Endoscopic management of recurrent tracheoesophageal fistula. World J Surg 31(12): 2412-2415.
- Atrah HI (1994) Fibrin glue. BMJ 308(6934): 933-934.
- Spotnitz WD (2010) Fibrin sealant: past, present, and future: a brief review. World Journal of Surgery 34(4): 632-634.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...