Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Research Article(ISSN: 2643-6760) 
Assessment of Surgical Outcome of Laparoscopic Appendectomy in Pregnant Women Volume 4 - Issue 2
Abdelrahman K Abdelrahman1*, Shaimaa Belal2, Hany M. Abd Elhameed3 and Manal Abdelwanees Elsayed3
- 1Fellow of General Surgery, El Sahel Teaching Hospital. Egypt
- 2Lecturer of Obstetrics and Gynecology, Faculty of Medicine, Helwan University. Egypt
- 3Fellow of Obstetrics and Gynecology, El Sahel Teaching Hospital. Egypt
Received: December 03, 2019; Published: December 18, 2019
Corresponding author: Abdelrahman K. Abdelrahman Department of General Surgery, El Sahel Teaching Hospital. Cairo. Egypt
DOI: 10.32474/SCSOAJ.2019.04.000181
Abstract
Introduction: Laparoscopic surgery during pregnancy is contraindicated absolutely or relatively through the last 10 years, however laparoscopic appendectomy (LA) still practiced for wome in pregnancy.
Patients and methods: 297 pregnant female diagnosed as acute appendicitis and managed with OA or LA in the emergency unit of the department of general surgery from June 2015 to December 2018.
Results: 162 patients underwent LA, while 117 patients underwent OA. No difference was noticed between both groups regarding the operative duration, fetal and maternal outcomes. However, the group of LA had faster first flatus, shorter inpatient duration than OA patients.
Conclusion: Laparoscopic appendectomy has been distinguished with efficacy and safety operation throughout pregnancy and should be considered a good replacement for open appendectomy.
Keywords: Appendix; laparoscopy; pregnancy; appendectomy
Abbreviaions: LA: Laparoscopic Appendectomy; OA: Open Appendectomy; SAGES: Society of American Gastrointestinal and Endoscopic Surgeons
Introduction
Abdominal pain in pregnant females could be caused by variant pathologies that made diagnosing of acute inflammation of appendix in pregnant women is quite difficult problem. Limitation of CT scanning, anatomical and physiological changes during pregnancy like physiological leukocytosis that could be associated with pregnancy were also contributing factors for difficult diagnosis [1]. Acute inflammation of appendix is the most common problem not related to pregnancy requiring urgent operative interference in pregnant women with an incidence between 0.05% and 0.13% [2]. The rate of complications in acute inflammation of appendix is much more increased in pregnant females [3]. Late recognition increases hazards of complications to the mother and her fetus when acute inflammation is in suspicious, so immediate intervention is better [4]. Laparoscopic appendectomy during pregnancy is recommended in the first and second trimester. Regarding the third trimester no clear guidelines for performing laparoscopic appendectomy [5]. The benefits of laparoscopic appendectomy over open appendectomy are less postoperative pain, early discharge, less risk for wound infection and giving feasibility for laparoscopic abdominal exploration [1,6]). In the current study, we assessed the feasibility and efficacy of laparoscopic appendectomy (LA) in pregnant females.
Patients and Methods
It is a retrospective study which was acheived in the casuality of the general surgery department, Elsahel Teaching Hospital and Helwan University teaching hospitals from June 2015 to December 2018. 279 pregnant women were included in this study. All of them were complaining of pain in the abdomen lower and right with or without fever, suggesting acute appendicitis. All patients underwent perioperative obstetric consultation and fetal monitoring. Complete blood count and pelvi-abdominal ultrasound were carried out to confirm the diagnosis and assess pregnancy. All pre-operative data including age, history of previous section, gestation age at operation and accuracy of the diagnostic U/S were recorded. Also, all operative data including the surgery duration, return time to normal bowel movement, inpatient length, postoperative complications and final pathology were recorded. Obstetric data and data of the fetus including the incidence of preterm labor, type of delivery, and fetal mortality were also recorded.
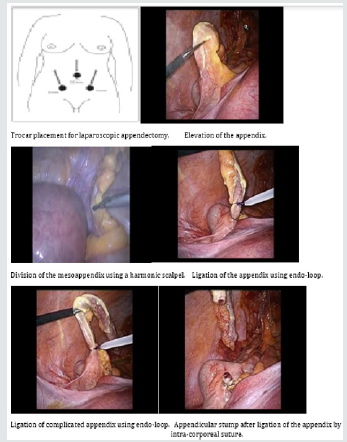
Technique of laparoscopic appendectomy (LA) in pregnant female
Procedure has been done while patient is supine and tilted slightly to the left side (20°-30°). The procedure was done using general anesthesia with maintained continuous end tidal volume CO2 monitoring. Insertion of Foley catheter was also practiced and using of pneumatic compression devices on the legs. A prophylactic antibiotic was administrated. Also, prophylactic tocolysis were administrated. We performed the operation by insertion of three ports. The first one supra-umbilical 10mm portion respect to the uterus dimentions (3-4cm higher than the uterine upper level) for the camera was inserted by open method (HASSON method) to avoid injury of the uterus. Another two working 5mm ports were inserted in both sides depending on the gestation age. Pneumoperitoneum by co2 was adjusted to be (10-12mm Hg). The appendix was elevated and the mesoappendix was divided using the bipolar diathermy or harmonic scalpel. The stump of the appendix was ligated by an endo-loop or intracorporeal stitches. Retrieval of the appendix in a glove was done through the umbilical port site. A drain was inserted to be removed after 1-2 days postoperative (Figure 1).
Statistical Analysis
Data are presented in the forms of means ± standard deviations. Comparison between patient groups was done using the Mann- Whitney U test or χ2 tes. Using of SPSS version 14.0 for all statistical comparisons, and results at p < 0.05 were considered significant.
Results
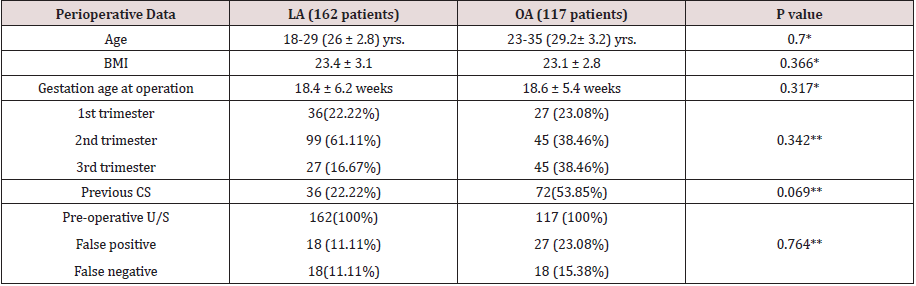
279 pregnant patients were selected for our study. 162 patients underwent laparoscopic appendectomy (LA), while 117 patients had an open appendectomy (OA). The mean age of the laparoscopic appendectomy (LA) patients’ group has been 26 ± 2.8 years and that of the OA patients’ group was 29.2 ± 3.2 years. There were no significant variations) in BMI or the gestational age before surgery between the two groups. Regarding all patients, 63 patients (36 LA and 27 OA) were in the 1st trimester, 144 patients (99 LA and 54 OA) were in the 2nd trimester, and 8 patients (27 LA and 45 OA) were in the 3rd trimester. In all patients, pre-operative ultrasound was done with a false positive rate (16.13 %) and false negative rate (12.9%) for all patients (Table 1).
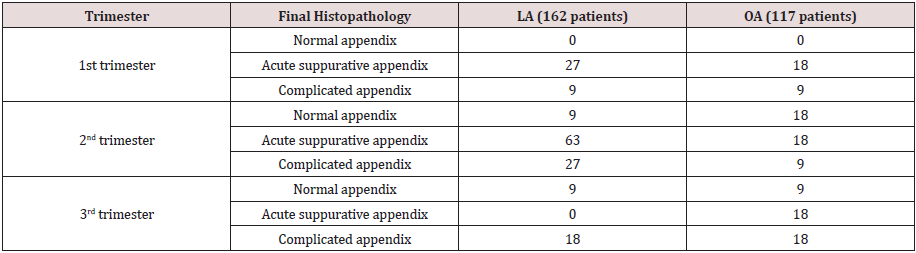
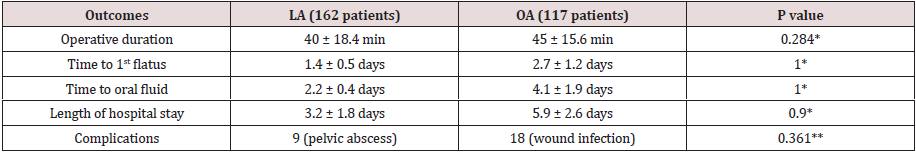
Regarding the final histopathology of the appendix, in the laparoscopic cases normal appendix was presented in 18 patients, acute suppurative in 90 cases, while complicated appendix was presented in 54 cases. In open cases, normal appendix was presented in 27 patients, acute suppurative in 54 cases, while complicated appendix was presented in 36 cases (Table 2) [7]. The duration of surgery in LA in this study was 40± 18.4 minutes, and in the OA was 45± 15.6 minutes. The time of the first flatus and the time of starting oral fluid were earlier in LA. Postoperative complications occurred in three patients. Nine patient developed intra-abdominal abscess occurred two weeks after a laparoscopic appendectomy. They were treated with application of pigtail US-guided and antibiotics. They completed their pregnancy and delivered a healthy baby. 18 patients developed wound infection after an open appendectomy, was managed with repeated dressing and antibiotics (Table 3).
Table 3: Operative data of laparoscopic appendectomy (LA) and open appendectomy (OA) while pregnancy.
* t-test p-value ** chi-square test p-value
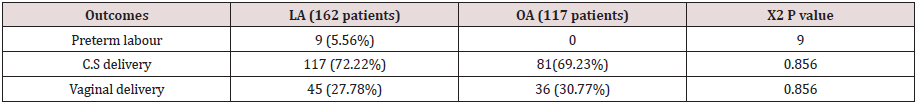
In our study, no mortality and all patients had uncomplicated deliveries. 9 patients had a preterm labor healthy baby. The two groups had the same results regarding the fetal outcomes with no problems or morbidity (Table 4).
Table 4: Operative data of laparoscopic appendectomy (LA) and open appendectomy (OA) while pregnancy.
Discussion
The most common abdominal surgery during pregnancy
for non-obstetric causes is acute appendicitis and the incidence
equals that of nonpregnant women, diagnosis is not easy due to
the physiologic and anatomic diferences that happened while
pregnancy [8]. The prevalence of acute inflammation of appendix
does not appear to be higher in pregnancy, but the incidence of
complications during pregnancy is higher than in general [3].
Complications may cause morbidity of both fetus and mother up to
loss of the fetus, hence pregnant females had to undergo immediate
surgery when appendicitis is suspected, irrespective of the
gestational age [9]. Acute appendicitis can present at any trimester,
but half of the cases can be seen on the 2nd trimester an observation
that published by Kapanet al. In our study more than half of the
cases were presented in the 2nd trimester. But in a study of Kazar et
al. and Mazze et al. they observed that the most accurate diagnosis
for acute appendicitis was during the first trimester [10,11].
It was known that the change in the physiology and the anatomy
while pregnancy made the recognition of acute inflammation of the
appenex difficult in pregnant females [7]. The number of normal
appendices after laparoscopic and open surgery while pregnancy
ranges from 0% up to 50% and 15% up to 50% in a respective
manner. In the current study, the negative appendectomy
percentage has been 16.13 % (45 patients) it was 11.11 % (18
patients) in LA and 23.08% (27 patients) in OA. In a study by Jun
Chul et al. the all negative appendectomies percentage was 9.8%
(9.1% for the laparoscopic appendectomies and 10.3% for the
open appendectomies) [7]. In our study, there was no conversion
of laparoscopic to open because the operation is done by a highly
experienced laparoscopic surgeon. Walsh et al reported 1% as a
rate of conversion of laparoscopic to open appendectomy [12].
Imaging are usually used to clarify a difficult clinical situation.
Ultrasonography has been used frequently as a first-line diagnostic
tool because it is safe for the mother and her fetus and it is highly
sensitive and specific for many intraperitoneal events. In the current
study, U/S has been done in whole patients; acute inflammation
of appendex was found in 77.78 % (126 females) in laparoscopic
appendectomy (LA) and was found in 69.23 % (81 females) in open
appendectomy (OA). In a study by Jun Chul et al; acute appendicitis
has been found in 15 (68.2%) patients in the laparoscopic
appendectomies and 28 (71.8%) in the open appendectomies [7].
In last decades, the preferred treatment for acute inflammation
of appendex while pregnancy was open appendectomy. But so
recently laparoscopic appendectomy could be done in pregnant
women with good results for both mother and her fetus [13]. Our
study supported the safety of LA; the outcomes of LA and OA were
the same. Also, many benefits of LA, including good intraoperative
visualization, lesser operative trauma, less manipulation of the
uterus, postoperative hospital stay is shorter and return to work
is faster, which is of more importance in pregnant females [14]. In
the current study, laparoscopic group had rapid return of bowel
function to normal and stay at hospital is shorter.
The Society of American Gastrointestinal and Endoscopic
Surgeons (SAGES) have previously published guidelines concerning
laparoscopic procedures while pregnancy [15] and refinements
done by Moreno et al [16]. A pneumoperitoneum pressure10-12
mmHg is advised as studies done on animals have demonstrated
hypercapnia and acidosis of the fetus due to CO2 pneumoperitoneum
in pregnancy [15]. In our study, pneumoperitoneum was adjusted
to 10-12 mmHg all the duration of the operation. There was
high recommendation to put the patient on her left side during
operation to facilitate access to the appendix and prevent pressure
on the inferior vena cava) [17]. Morrell and colleagues [18] have
advicd that operating table should be rotated to the left side to
take away the uterus for a better venous return. In the current
study, all patients have been put in a supine position slightly tilted
to the left side (20°-30°). The most important concern during
laparoscopic appendectomy (LA) in pregnancy is a possible risk of
injury to the uterus during port insertion. Hasson open technique
or the Veress needle can be used to access the abdominal Cavity.
Possible complications have been described for both methods but
the most serious is inadvertent puncture of the uterus with a Veress
needle [19]. Friedman and colleagues [20] had results in a pregnant
woman at 21 weeks of pregnancy that underwent laparoscopic
appendectomy (LA) for suspected appendicitis. Serosal tear of the uterus with Veress needle resulted in postoperative pneumoamnion
with loss of the fetus. In the current study, we insert camera port
supraumbilical 3-4cm above the uterine fundus with open method
(HASSON method) according to SAGES guidelines for laparoscopy
during pregnancy [15].
Blood stasis in the lower limbs is anticipated in pregnant
women, so pregnant females are more susceptible to
thromboembolic events. The SAGES guidelines recommended
pneumatic intermittent compression devices to be used during
intraoperative and postoperative periods with early ambulation
postoperatively to lower the incidence of deep vein thrombosis in
pregnant Women [15], and this was applied in the study with no
postoperative thromboembolic complications. The risk of preterm
labors with any operative interference during pregnancy reported
to be 10-15%. The same was observed after laparoscopic or open
appendectomies that were reported by Kazar et al. [10]. The
overall rate of preterm labors was one patient (3.22%) in LA. In
conclusion, laparoscopic appendectomy is distinguished by safety
and efficacy throughout pregnancy and had good fetal and maternal
outcome like open appendectomy. Added to all the advantages of
laparoscopy, laparoscopic appendectomy is associated with short
postoperative stay, early restoration of function of bowel and low
incidence of trauma to the gravid uterus.
References
- Pearl J, Price R, Richardson W (2011) Guidelines for diagnosis, treatment, and use of laparoscopy for surgical problems during pregnancy. Surg Endosc 25(11): 3479-3492.
- Kirshtein B, Perry ZH, Avinoach E (2009) Safety of laparoscopic appendectomy during pregnancy. World J Surg 33(3): 475-480.
- Corneille MG, Gallup TM, Bening T (2010) The use of laparoscopic surgery in pregnancy: evaluation of safety and efficacy. Am J Surg 200(3): 363-367.
- McGory ML, Zingmond DS, Tillou A (2007) Negative appendectomy in pregnant women is associated with a substantial risk of fetal loss. J Am Coll Surg 205(4): 534-540.
- Samardizic J, Delibegovic S, Latic F (2011) Laparoscopic appendectomy is safe procedure in the pregnant patients in second trimester. Med Arch 65(5): 125-126.
- Mazze RI, Kallen B (1991) Appendectomy during pregnancy: a Swedish registry study of 778 cases. Obstet Gynecol 77(6): 835-840.
- Jun Chul Chung, Gyu Seok Cho, Eung Jin Shin (2013) Clinical outcomes compared between laparoscopic and open appendectomy in pregnant women. Can J Surg 56(5): 341-346.
- Moreno-Sanz C, Pascual-Pedreño A, Picazo-Yeste JS (2007) Laparoscopic appendectomy during pregnancy: between personal experiences and scientific evidence. J Am Coll Surg 205(1): 37-42.
- Carver TW, Antevil J, Egan JC (2005) Appendectomy during early pregnancy: What is the preferred surgical approach? Am Surg 71(10): 809-812.
- Kazar RA, Roslyn JJ (1999) The appendix. In: Schwartz SI, Shires GT, Spencer FC, Daly JM, Fischer JE, Galloway AC, editors. Principles of Surgery. McGraw-Hill, USA, pp. 1384-1394.
- Mazze Richard I, Bengt K (1991) Appendectomy during pregnancy: a Swedish registry study of 778 cases. Obstet Gynecol 77(6): 835-840.
- Walsh CA, Tang T, Walsh SR (2008) Laparoscopic versus open appendectomy in pregnancy: a systematic review. Int J Surg 6(4): 339-344.
- Park SH, Park MI, Choi JS (2010) Laparoscopic appendectomy performed during pregnancy by gynecological laparoscopists. Eur J Obstet Gynecol Reprod Biol 148(1): 44-48.
- Lyass S, Pikarsky A, Eisenberg VH (2001) Is laparoscopic appendectomy safe in pregnant women? Surg Endosc 15:377-379.
- Guidelines for laparoscopic surgery during pregnancy (1998) Society of American Gastrointestinal Endoscopic Surgeons (SAGES). Surg Endosc 12(2):189-90.
- Moreno-Sanz C, Pascual-Pedreno A, Picazo-Yeste JS, Seoane-Gonzalez JB (2007) Laparoscopic appendectomy during pregnancy: between personal experiences and scientific evidence. J Am Coll Surg 205(1): 37-42.
- Curet MJ, Allen D, Josloff RK (1996) Laparoscopy during pregnancy. Arch Surg 131: 546-550.
- Morrell DG, Mullins JR, Harrison PB (1992) Laparoscopic cholecystectomy during pregnancy in symptomatic patients. Surgery 112(2): 856-859.
- Friedman JD, Ramsey PS, Ramin KD (2002) Pneumoamnion and pregnancy loss after second-trimester laparoscopic surgery. Obstet Gynecol 99(3): 512-513.
- Malangoni MA (2003) Gastrointestinal surgery and pregnancy. Gastroenterol Clin North Am 32(1): 181-200.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...