
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Research Article(ISSN: 2643-6760) 
Application of Oxygenation via Nasopharyngeal Tube on Rigid Bronchoscope Intubation Volume 5 - Issue 3
Haidong He1, Hongwei Wang2, Guozheng Li2, Feiyan Lou3, Huiping Hu3 and Weihua Xu1*
- 1Respiration Department, Tongde Hospital of Zhejiang Province, Hangzhou City, China
- 2Anesthesiology Department, Tongde Hospital of Zhejiang Province, Hangzhou City, China
- 3Endoscopy Department, Tongde Hospital of Zhejiang Province, Hangzhou City, China
Received: July 24, 2020; Published: August 07, 2020
Corresponding author: Weihua Xu, Respiration Department, Tongde Hospital of Zhejiang Province 234#, Gucui Road, Hangzhou, Zhejiang Province, 310012, China
DOI: 10.32474/SCSOAJ.2020.05.000215
Abstract
Rigid bronchoscopy is an invaluable tool of interventional pulmonology. Performing rigid bronchoscopy requires professional skills. Successful intubation is the first challenge, and providing enough oxygenation is important for intubation because of patient’s condition of general anesthesia and paralysis. This research reported the clinic experiences of using nasopharyngeal tube to provide ideal oxygenation during rigid bronchoscope intubation. 11 patients received 12 rigid bronchoscope operations. Among them, nine patients were pulmonary carcinoma patients, one suffered from bronchiectasis with the combination of massive hemoptysis, one was tuberculosis patient who got the right intermediate bronchus stenosis. There were three cases whose intubation of rigid bronchoscope failed. The intubation time of other nine successful cases was 3.19±1.43 minutes. The average oxygen saturation (SaO2) of 12 cases was 97.8%±1.4% (ranged from 95% to 100%). End-tidal carbon dioxide pressure (EtCO2) was 40.1±7.4 mmHg (from 31 mmHg to 58 mmHg). During rigid bronchoscope intubation, heart rate (HR), diastolic blood pressure (DBP), systolic blood pressure (SBP) was recorded as 80.2±10.9, 72.2±8.2 mmHg, 135.4±10.4 mmHg. We concluded that oxygenation via nasopharyngeal tube was a safe, easy, and effective method for supporting oxygenation during rigid bronchoscope intubation.
Keywords:Bronchoscopy and interventional techniques; Ventilation; Lung cancer
Introduction
Rigid bronchoscopy has been used for more than a century. It maintains a central role in the diagnosis and management of both malignant and benign diseases [1-2]. For interventional pulmonologists, performing rigid bronchoscopy requires professional skills, and successful intubation is the first challenge. During rigid bronchoscope insertion, most patients generally receive deep sedation. For some patients, paralysis is always performed. Under the conditions of deep anesthesia and paralysis, providing enough oxygenation is important for successful intubation. The clinic experiences of using nasopharyngeal tube to provide ideal oxygenation, different from the common oxygenation methods during rigid bronchoscope intubation, are narrated in the present report.
Methods
Clinical evaluation before operation
Patients who need stent implantation, stent removal, or central airway tumor ablation had been selected from March 2018 to July 2019. All the operations in the present study are ethically approved, and are consented by patients. Basic laboratory tests including complete blood count, blood gas test, coagulation function, chest imaging, and electrocardiogram had been done before the operations. Depending on the patients’ medical conditions, additional testing such as lung function, 6-min walk test had been performed. Anesthesiologists were invited to evaluate the medical conditions of patients. Those patients who were severe tendency of hemorrhage, intolerance of general anesthesia, were forbidden for rigid bronchoscope operations. Apart from the procedures above, attention had been paid to evaluate the conditions of the oral cavity, jaw, and neck mobility for avoiding some conditions that may prevent rigid bronchoscope intubation. These conditions included unstable cervical spine or diminished range of motion of the cervical spine, maxillofacial or oral disease resulting in difficult opening of the jaw to admit the scope intubation, and laryngeal disease such as stenosis or obstructing neoplasm.
Anesthesia Technique
The patients were put at supine position. The head of the bed was dropped a little to allow maximal extension of the neck. Prior to anesthesia, the patient received oxygenation with fraction of inspired oxygen (FiO2) of 1.0 via bag valve mask for three minutes to preserve oxygen for the following procedures. Non-invasive measurement of oxygen saturation (SaO2), heart rate (HR), diastolic blood pressure (DBP), systolic blood pressure (SBP) was monitored. During preoxygenation via bag valve mask, general anesthesia with or without paralysis were performed on patients. Medications including propofol, dexmedetomidine, remifentanil, midazolam, sufentanil, etomidate, succinylcholine, or rocuronium were used intravenously. Among them, propofol, dexmedetomidine, remifentanil was injected continuously by micro pump. Medication choice, dosage of medication was decided by anesthesiologist based on the medical conditions of the patients.
Nasopharyngeal tube intubation
Nasopharyngeal tube (Excellentcare Medical Huizhou Limited Company, Huizhou, China) with inner diameter of 7.0mm and length of 15.0cm was used after general anesthesia. Lubricant was sprayed into nasal airway for local anesthesia. Nasopharyngeal tube was also smeared with lubricant and was inserted into the nares down to the posterior pharynx. If there was resistance, the operator gently rotated the nasopharyngeal tube to fit the tube snugly into the nasal airway. At approximately 6 to 7cm in the tube, less resistance would be felt. At this point, nasopharyngeal tube passed through the nasal passageway and dropped into the nasopharynx. Then nasopharyngeal tube was fully inserted into pharynx.
Once nasopharyngeal tube was successfully placed, ventilator was connected to the proximal terminal of nasopharyngeal tube for supplying oxygen at appropriate respiratory frequency (20 to 30 times per min) with appropriate oxygen concentration (35% to 100%) and ventilation volume (10 to 15ml/kg). End-tidal carbon dioxide pressure (EtCO2) was consequently monitored by transducer inside the conduit of ventilator. For those patients with respiratory acidosis, arterial cannulation was performed to regularly monitor arterial blood gas analysis.
Rigid bronchoscope intubation
Rigid bronchoscope (KARL STORZ SE & Co. KG, Tuttlingen,
Germany) was smeared with lubricant. Prior to intubation, sterile
gauzes were placed to protect the teeth. Flexible bronchoscope
(Olympus (China) Co., Ltd, Beijing, China) was put into rigid
bronchoscope as light source to guide rigid bronchoscope insertion.
Then the mouth of patient was opened by an assistant and the rigid
bronchoscope was carefully inserted into the oral cavity. Initially
visualizing the tongue and hard palate, the rigid bronchoscope
passed through the oral cavity until the uvula was visualized. The
scope was lowered and advanced further until the epiglottis was
seen. Then the epiglottis was lifted anteriorly using the bevel of the
rigid bronchoscope to expose the vocal cords and the glottis. When
the patient’s glottis was anterior, the rigid bronchoscope was forced
towards the glottis, and was then rotated 90 degrees to allow the
bevel to pass through the vocal cords. After entering tracheal way,
the rigid bronchoscope was rotated back making the bevel of the
scope rest on the posterior membrane of the trachea.
Once rigid bronchoscope intubation achieved, ventilator
conduit was taken off from the nasopharyngeal tube and connected
to the rigid bronchoscope. Pulmonologists began to perform
operations on patients. When rigid bronchoscope had not been
successfully inserted into tracheal airway within 20 minutes,
rigid bronchoscope intubation was terminated. Instead tracheal
intubation using 8.0cm or 8.5cm diameter oral-tracheal tube was
performed for further operations. During the rigid bronchoscope
intubation, SaO2, EtCO2, HR, DBP, SBP were recorded every minute.
For each patient, the maximum value of EtCO2 was selected to be
value of EtCO2, the average value of SaO2, HR, DBP, SBP was used to
be value of SaO2, HR, DBP, SBP. Complications of nasopharyngeal
tube insertion including gastric distention, nasal mucosa injury,
vomite, epistaxis, turbinate fracture, basilar skull fracture, sinusitis,
and nasopharyngeal injury were observed.
Results
Eleven patients received twelve rigid bronchoscopic operations. Four patients were female and other patients were male. The age was 66.3±13.9 years. Among them, nine patients were pulmonary carcinoma patients, one suffered from bronchiectasis with the combination of massive hemoptysis, and one got endobronchial tuberculosis with the combination of right intermediate stenosis (Table 1). The bronchiectasis patient received two operations (Case 6 and Case 9). The first operation of the bronchiectasis patient was for implanting two straight silicon stents in the right middle lobe bronchus and right intermediate bronchus to occlude the breeding pathway from the right middle lobe. The second aimed to remove the stent in the right intermediate bronchus after hemoptysis had been successfully controlled.
Table 1: Clinic data about 11 patients, 12 operations.
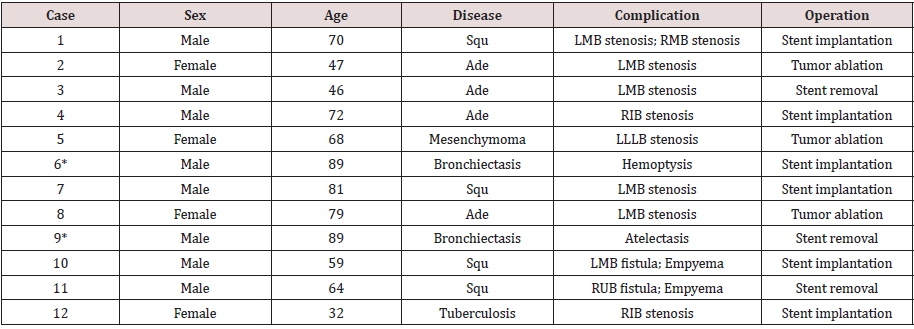
Squ: Squamous cell carcinoma; Ade: Adenocarcinoma; LMB: Left main bronchus; RMB: Right main bronchus; RIB: Right intermediate bronchus; LLLB: Left lower lobe bronchus; RUB: Right upper lobe bronchus; *: Case 6 and case 9 is the same patient.
twelve operations, stent placement had been performed
six times. Case 1 and case 10 received Y-shaped silicon stent
(Tracheobronxane, Novatech, La Ciotat, France) implantation. Two
customized straight silicon stents (Tracheobronxane, Novatech,
La Ciotat, France) were implanted on case 6 with one in the right
middle lobe bronchus and another in the right intermediate
bronchus. Covered metal stents (Ultraflex, Boston Scientific co., MA,
USA) were deployed on case 4 and case 7. Non-covered metal stent
(Micro-Tech (Nanjing) Co., Ltd, Nanjing, China) was implanted in
the right intermediate bronchus of case 12 for alleviating bronchial
stenosis. Three patients including case 2, case 5 and case 8 were
performed tumor ablation in the left main bronchus or left lower
lobe bronchus by argon beam coagulator or electrocoagulation.
Stent removal was operated on case 3, case 9 and case 11.
During rigid bronchoscope intubation, eight kinds of anesthetic
and paralysis medications were used (Table 2). Every patient
received both anesthetic and paralysis medications. All the twelve
cases received final operations. There were three cases failed to be
performed rigid bronchoscope intubation (Table 3). The intubation
time of nine successful intubation cases was 3.19±1.43 minutes.
The average SaO2 of 12 cases was 97.8%±1.4% (ranged from
95% to 100%). EtCO2 was 40.1±7.4 mmHg (from 31 mmHg to 58
mmHg). During rigid bronchoscope intubation, HR, DBP, SBP was
recorded as 80.2±10.9, 72.2±8.2 mmHg, 135.4±10.4 mmHg. No
severe complication was found. Two patients (case 3 and case 7)
suffered from epistaxis. This complication was controlled by nose
packing. After operation, nasal congestion occurred on case 10 and
self-cured 3 days later.
Table 2: Anesthetic and paralysis medications of 12 operations.
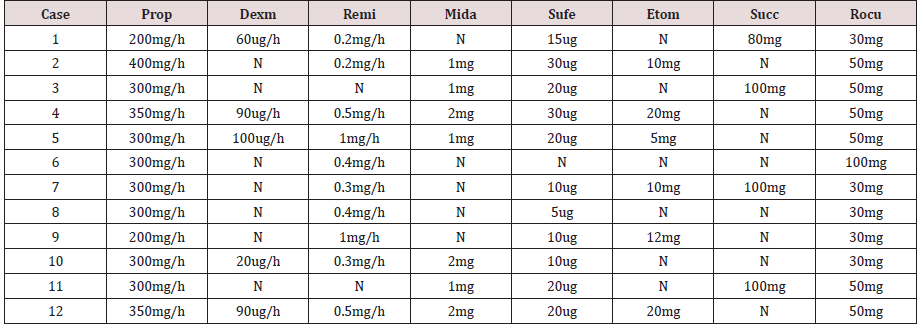
Prop: Propofol; Dexm: Dexmedetomidine; Remi: Remifentanil; Mida: Midazolam; Sufe: Sufentanil; Etom: Etomidate; Succ: Succinylcholine; Rocu: Rocuronium; N: No use.
Table 3: Data of intubation time, SaO2, HR, DBP, SBP, EtCO2 of 12 operations.
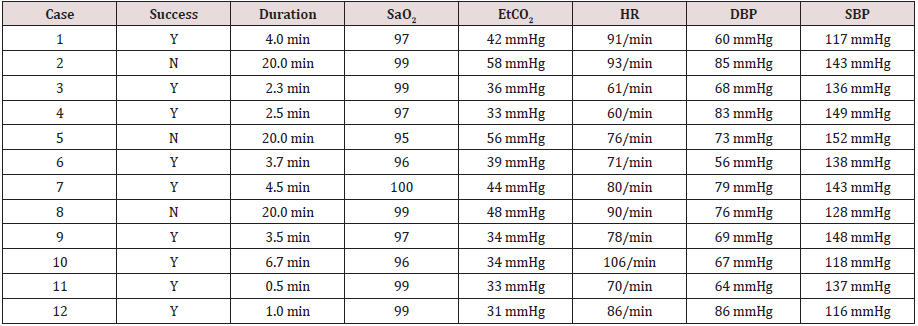
Y: successful intubation; N: failed.
Discussion
Rigid bronchoscope was firstly used by Gustav Killian in 1876
to remove a pork bone from the right main bronchus, followed by
successful removal of airway foreign bodies in other three cases
[3-4]. From then on, rigid bronchoscopy had been performed more
frequently, and its role had been expanded beyond foreign bodies
removal, including but not limited to endobronchial treatment of
tuberculosis complications, endoluminal mechanical resection
of endobronchial tumors [1]. Especially when Dr. Jean Francois
Dumon developed silicon stents for relieving airway stenosis [5],
rigid bronchoscopy came to the central position in the diagnosis
and management of airway diseases.
Like tracheal tube, rigid bronchoscope is inserted from oral
cavity to trachea, and need to be connected to ventilator for
providing oxygen. However, the outer diameter of adult rigid
bronchoscope (14 mm or 12 mm) is much larger than tracheal
cannula (6.5mm to 8.5mm). Rigid bronchoscope is made of stainless
steel, different from tracheal tube which is soft and flexible. Rigid
bronchoscope is so long, rigid, and inflexible that putting it into
trachea through oralpharyngeal airway is difficult. Intubation of
rigid bronchoscope requires more professional skills and spends
more time than tracheal tube intubation. Appropriate position of
patient and usage of anesthetic medications may be conductive to
successful intubation of rigid bronchoscope.
Comparing with flexible bronchoscopy, rigid bronchoscopy
needs general deep sedation. Under the condition of general
anesthesia and muscle relaxation, respiration of patient weakens so
far as to stop. Additional oxygen should be provided or the patient
would die of apnea. Thus, rigid bronchoscope intubation itself is
a big challenge which contains two aspects, how to successfully
intubate the scope into trachea and how to provide enough
oxygen during intubation. The common oxygenation methods
for operations of rigid bronchoscopy are apneic oxygenation,
spontaneous assisted ventilation, controlled ventilation (closed
system), manual jet ventilation, high-frequency jet ventilation [6-
7]. However, these methods are not used for rigid bronchoscope
intubation. Up till the present moment, preoxygenation with 100%
oxygen via a bag valve mask for several minutes is usually performed
to reserve oxygenation for further rigid bronchoscope intubation,
during which pulmonologists only rely on preoxygenation for
oxygen supply. When preoxygenation is performed for 3 minutes,
an adequate level of oxygen saturation can be maintained for about
5 minutes [8]. But for the patients who receive the operation of
rigid bronchoscopy, this ideal oxygen saturation time is much less
than 5 minutes because most of these patients suffered from airway
obstruction which weakens the effect of preoxygenation. This
condition requires pulmonologists accomplish rigid bronchoscope
intubation in short time or intubation should be terminated ahead
of time, and patients need to be re-oxygenated. Furthermore, even
ample preoxygenation is performed, hypoxemia occurs in 10%
to 30% of patients especially in the elderly [9]. More effective
method of oxygenation is significant for rigid bronchoscope
intubation especially when the operator is not able to perform rigid
bronchoscope intubation within short time.
Nasopharyngeal tube is hollow, soft, made of plastic or rubber.
Its intubation is relatively easy. Nasopharyngeal tube is placed
from nose cavity to the posterior pharynx, its cephalic terminal
can be connected to the ventilator. Hence the patients may get the
supplemental oxygen supply during the whole intubation process,
different from preoxygenation via bag valve mask which only support
oxygenation once before intubation. In this clinic research, effective
oxygenation was provided by ventilator via nasopharyngeal tube.
The data showed that during the intubation process, SaO2, EtCO2, HR,
DBP and SBP were all kept normal and stable. Even in three failedintubation
patients, ideal oxygenation was provided in 20 minutes
without breaking off for reoxygenation. This result certified that
oxygenation via nasopharyngeal tube immensely surpassed the preoxygenation via bag valve mask in providing idea oxygenation
for longer time during rigid bronchoscope intubation. Because of
this, the present study had not involved the preoxygenation via bag
valve mask to be the contrast.
Apart from three failed-intubation patients, the intubation
time of nine successful cases was 3.19±1.43 minutes. It is not good
enough when comparing with operations of more professional
pulmonologists. In consideration of development of rigid
bronchoscopy in the present hospital less than 3 years, intubation
time of 3.19 minutes is relatively acceptable. Most importantly, this
result indicated that nasopharyngeal tube did not exert impedance
on the intubation of rigid bronchoscope. Furthermore, few
complications relevant to nasopharyngeal tube intubation ensured
its safety.
Conclusion
Based on the data above, conclusion is drawn that oxygenation via nasopharyngeal tube is a safe, easy, and effective method for supporting oxygenation during rigid bronchoscope intubation. This method may provide a good choice for pulmonologists when rigid bronchoscopy is performed.
References
- Flannery A, Daneshvar C, Dutau H, Breen D (2018) The Art of Rigid Bronchoscopy and Airway Stenting. Clin Chest Med 39:149-67.
- Semaan R, Yarmus L (2015) Rigid bronchoscopy and silicone stents in the management of central airway obstruction. J Thorac Dis 7(4): S352-362.
- Becker HD, Marsh BR (2000) History of the rigid bronchoscope. In: Interventional bronchoscopy. Karger Publishers, Basel, Switzerland, p. 2-15.
- Kollofrath O (1897) Entfernung eines Knochenstu¨cks aus dem rechten Bronchus auf natu¨ rlichem Wege und unter Anwendung der directen Laryngoscopie. Munchener Medizinische Wochenschrift 38: 1038-1039.
- Dumon JF (1989) A specific tracheobronchial endoprosthesis [in French] Presse Med18: 2055-2058.
- Pathak V, Welsby I, Mahmood K, Wahidi M, MacIntyre N, et al. (2014) Ventilation and anesthetic approaches for rigid bronchoscopy. Ann Am Thorac Soc 11: 628-634.
- Putz L, Mayné A, Dincq AS (2016) Jet Ventilation during Rigid Bronchoscopy in Adults: A Focused Review. Biomed Res Int pp.
- Bodily JB, Webb HR, Weiss SJ, Braude DA (2016) Incidence and duration of continuously measured oxygen desaturation during emergency department intubation. Ann Emerg Med 67: 389-395.
- Kang H, Park HJ, Baek SK, Choi J, Park SJ (2010) Effects of preoxygenation with the three minutes tidal volume breathing technique in the elderly. Korean J Aneathesiol 58: 369-373.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...




