
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Research Article(ISSN: 2643-6760) 
Application of 3D Visualization Technology in Preoperative Planning of Giant Goiter Volume 7 - Issue 2
Yisong Wang1†, Hongzhen Zhang2†, Yongtian Li1†, Wenping Wang3, Danqing Cheng3, Dingfei Ren5 and Feng Zhao4*
- 1Anhui University of Science and Technology, China
- 2Shanghai Fengxian Hospital, affiliated to Anhui University of Science and Technology, China
- 3Graduate School of Bengbu Medical College, China
- 4The First Hospital of Anhui University of Science & Technology (Huai nan first people’s Hospital), China
- 5Occupational control hospital of Huai He energy group, Huai Nan, Anhui Province, China
Received: January 11, 2023; Published: January 26, 2023
Corresponding author: Feng Zhao, The First Hospital of Anhui University of Science & Technology, Huai nan first people’s Hospital, China
DOI: 10.32474/SCSOAJ.2023.07.000260
Abstract
Background and Objectives: 3D visualization technology provides a more intuitive visual virtual reality surgical presentation for preoperative simulation planning, inhand visualization operation and accurate postoperative assessment in surgical procedures, but there is a lack of evidence to support whether this technology is more advantageous in preoperative planning of giant goiter. The aim of this study was to investigate the value of 3D visualization technology in the preoperative planning of giant goiter.
Methods: The clinical data of eight patients with giant goiter admitted to the First People’s Hospital of Anhui University of Technology for general surgery from October 2020 to August 2022 were retrospectively analyzed. The image data were imported into 3D visualization software (3D Slicer software) in DICOM format for 3D reconstruction to analyze the 3D positional relationship between the giant thyroid nodules and the surrounding tissues and organs, to perform preoperative simulation operations, and to develop precise surgical pathways.
Results: All patients were operated according to the optimal plan selected by the simulation operation, and the actual surgical procedure conformed to the preoperative simulation plan 100%, and all of them successfully completed the total resection of giant thyroid nodules without any perioperative death and no new symptoms appeared after the operation.
Conclusion:The use of 3D visualization technology in the preoperative planning of giant goiter can accurately obtain 3D anatomical information of the lesion and its adjacent tissues, select the optimal surgical path, and reduce surgical risks, which is of great clinical guidance value in guiding the preoperative precise surgical planning of giant goiter.
Keywords: 3D visualization; thyroid surgery; giant goiter; preoperative planning; precision treatment
Background
Giant goiter refers to the largest diameter of thyroid ≥10cm or goiter with grade III or above [1,2]. Although the vast majority of thyroid giant nodules are benign nodules, because of their huge volume, they are easy to oppress adjacent tissues and organs, which can easily lead to serious complications such as obstruction of blood flow in the head and neck, dyspnea and even suffocation [3], Therefore, surgical resection is urgently needed to relieve the compression of the tumor on the trachea, vascular nerves, etc. According to the 2015 American Thyroid Association management guidelines, large thyroid nodules are an absolute indication for surgery [4]. However, due to the enlarged vascular malformation on the surface of the giant thyroid nodules, some of them have reticulated sinuses on the surface of the giant thyroid nodules, which can bleed easily when touched. At the same time, the compression of the giant nodules leads to deformation or displacement of the trachea by compression, and the anatomical relationship of the surrounding tissues and blood vessels can be altered, leading to increased surgical operations, increased surgical risks and serious postoperative complications.
In recent years, 3D visualization technology has been more and more widely used in surgery. 3D visualization technology can visually and three-dimensionally display the size and location of the tumor and its anatomical position in relation to the surrounding blood vessels and nerves, which has significant preoperative guidance value [5-7]. Therefore, favorable application of noninvasive 3D visualization technology in the preoperative planning of giant goiter will become a trend in the surgical treatment of patients with this disease. Through 3D visualization technology, the anatomical structure, morphology, size and relationship with neighboring tissues and organs of the giant thyroid lesion are precisely analyzed, and a detailed surgical plan is made; the unnecessary exploration of head and neck structures is reduced intraoperatively to achieve precise positioning, reduce The operation was performed to reduce unnecessary exploration of head and neck structures, achieve precise positioning, reduce trauma, greatly shorten the operation time, and preserve the healthy thyroid tissue to the maximum extent. In this study, we retrospectively analyzed eight postoperative patients with giant goiter, all of whom used 3D visualization technology to construct preoperative models, analyze the 3D anatomical relationships of the giant thyroid nodule, surrounding vascular nerves and trachea, and develop accurate surgical preoperative plans and simulations during surgery. The surgeons finally confirmed the value of 3D visualization technology as an important guide for preoperative planning in the actual operation of giant goiter surgery.
Data and Methods
Nano-emission Standard
Inclusion criteria: (1) Preoperative diagnosis of giant thyroid nodules and compliance with absolute surgical indications. (2) Patients and family members were aware of the risks of surgery and voluntarily signed the informed consent form. Exclusion criteria: (1) Patients with pathological diagnosis of thyroid malignancy by fine needle aspiration biopsy of the thyroid gland. (2) Patients and family members who do not agree to perform thyroid surgery. (3) Patients with major organ organ dysfunction, cardiac insufficiency, and hepatic and renal insufficiency. (4) Patients with impaired consciousness or mental disorders. (5) Those with incomplete inpatient medical history.
General Information
From September 1, 2020 to August 31, 2022, 8 cases of giant goiter were treated in the general surgery inpatient department of the First Affiliated Hospital of Anhui University of Science and Technology, including 5 females and 3 males, with an average age of 51.4 years, ranging from 33 to 68 years, with a course of 4 to 11 years. Among them, 1 case of TI-RADS 2, 6 cases of TI-RADS 3 and 1 case of TI-RADS 4a were evaluated by ultrasound. All patients underwent neck color Doppler ultrasound and CT scan before operation. Imaging results showed huge goiter, with 5 cases of bilateral occupying and 3 cases of unilateral occupying. The minimum diameter of ultrasonic nodules was 10.8 cm, the maximum diameter was 19.6 cm, and the average diameter was 14.5 cm. CT showed that all patients with goiter had different degrees of tracheal deformation or displacement. The maximum displacement of trachea on X-ray film was about 3.0 cm, and the degree of tracheal compression was reduced by 0.5~0.85 cm. All patients’ tumor tissues were sent to routine frozen sections for pathological examination.
Inspection Method
The CT examination was performed with a GE Light Speed 16-layer spiral CT scanner, and the MRI examination was performed with an OPEN MARK-II MRI scanner (thin layer scanning, layer thickness 1.0 mm), and the patient’s preoperative CT and MRI imaging data of thyroid nodules were collected and stored in DICOM format, and the 2D image data were imported into 3D-Slicer software to construct a 3D visualization model of the giant thyroid nodules and their A 3D visualization model of the giant thyroid nodule and its surrounding tissues was constructed. Through the model, a complete and clear 3D anatomical virtual reality model of the thyroid tumor, trachea, jugular artery and other organs and tissues can be obtained, especially to further grasp accurately the location of the tumor, the tumor pointing, the adjacent relationship between the tumor and the surrounding important blood vessels and nerves, the details of the tumor compressing the trachea, simulate the surgical procedure, and formulate a more accurate preoperative planning path. In addition, the 3D model interface can be rotated, cut, edited, and computerized to measure the size of the tumor and adjust the transparency, and it can also be rotated and magnified to observe from different angles and directions for fine surgical plan planning.
Results
Preoperative evaluation of giant thyroid nodules
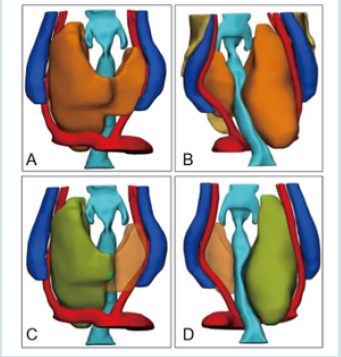
Eight patients with giant thyroid (nodules > 3 cm) were admitted to hospital. In the three-dimensional reconstruction model of head, neck and chest, the lower thyroid pole exceeded the thoracic entrance. After evaluation, the vertical length of all patients was 0 ~ 23.9mm (13.8±10.4 mm), and the total volume of the three-dimensional model of thyroid was 10.78 ~ 184.97cm3 (81.20±68.42cm3). The volume above the thoracic entrance was 10.78 ~ 160.68cm3 (66.73±59.61 cm3), and the volume below the thoracic entrance was 0 ~ 50.51cm3 ( 21.71±18.17 cm3), which did not meet the target of combined thyroidectomy. Therefore, all 8 patients could be completely removed by cervical incision. A patient was selected to show that the measured vertical length is about 10.5mm, the volume of thyroid gland (orange part) below the thoracic entrance is about 23.6 cm3 (accounting for 29.7% of the whole), and the volume of giant thyroid nodule (green part) above the thoracic entrance is about 54.5 cm3, with an angle Z of about 86 (Figure 3).
Preoperative simulated surgical path
In all patients, the thyroid nodules were clearly identified, and the maximum diameter could be measured on preoperative CT 3D reconstruction in the cervical extension position, providing a quick and accurate view of the spatial location of the nodules in the entire thyroid gland, and a quick and accurate view of the spatial location of the nodules in the entire thyroid gland. Assessment of the nodule’s proximity to the trachea, esophagus, etc. Because of the huge nodule, it is easy to oppress the adjacent tissues and organs of the neck, resulting in serious complications such as dyspnea, dysphagia, and obstruction of blood flow in the head and face. Therefore, surgical resection is needed to relieve the oppression of trachea, esophagus, blood tube, nerves, etc. To know the vocal cord activity, the degree of tracheal compression and stenosis before operation, and to evaluate the tracheomalacia. Contrast-enhanced CT of the neck can know the nodule size, the relationship with the surrounding tissue structure and the depth of falling into the upper mediastinum in detail.
The upper incision should reach the upper pole of thyroid gland, so inclined arc incision is often used. If the tumor can be completely removed after detailed preoperative evaluation, oblique shuttle incision can be designed. Firstly, the design is centered on the middle and low neck striations, and the width of the cut skin is determined according to the size of the nodules. After rehabilitation, the skin scar on the neck of the patient is still like the skin lines of the neck itself, which can achieve a certain cosmetic effect on the neck (Figure 3). Because of the long-term compression and traction of the anterior cervical banded muscles by the tumor, the anterior cervical banded muscles of most patients become thin and membranous. If the lower pole of the tumor falls deep into the upper mediastinum, it can’t be resected through the neck, and the resection of mediastinum by combined cervicothoracic surgery is more safe and reliable.
Surgical effect
All surgical cases were treated with tracheal intubation and general anesthesia. Due to the long-term compression of giant thyroid nodules, some patients’ tracheas are severely narrowed, and intubation is difficult under induced anesthesia. Therefore, we can choose to intubate under the guidance of fiberoptic bronchoscope in awake state, which can prevent dyspnea and even suffocation due to the failure to insert endotracheal tube after induced anesthesia. In this group, 3 cases were intubated in awake state, and the anesthesia effect was very good.
All the 8 patients in this group successfully used 3D visualization technology to construct 3D thyroid model preoperative precise planning and preoperative surgical simulation. The actual implementation of the operation was consistent with preoperative planning, and all operations were performed by the same group of surgeons. Unilateral lobectomy was performed in 3 cases, bilateral lobectomy in 2 cases, total thyroidectomy in 1 case, unilateral lobectomy plus isthmus resection in 1 case. One case of anaplastic thyroid cancer with abscess formation severely compressed trachea and esophagus with dysphagia. The tumor abscess was cut and decompressed to relieve the tumor’s compression on trachea and esophagus. No invasion of the trachea and esophagus by thyroid nodules was found in this group, but the trachea and neck vessels in all cases were compressed and displaced in different degrees.
The coincidence rate of all patients’ actual operation conditions with the three-dimensional visualization guidance plan was 100%. After general anesthesia, all patients successfully removed the huge thyroid nodules, and the intraoperative blood loss was 5~10ml. All the operations were successfully completed. CT and MRI of thyroid gland were reexamined 2 weeks and 6 months after operation. The scope of resected tissue was consistent with the preoperative plan, and there were no complications such as injury of cervical great vessels and injury of recurrent laryngeal nerve.
Typical cases
The patient is a female, aged 49. After physical examination, the right thyroid nodule was found. After 2 months, the nodule was obviously enlarged and felt suffocated. He came to our hospital on June 2, 2022 (Figure 1). Physical examination after admission: clear speech, good mental state, good nutritional development, independent posture, cooperation in physical examination and accurate answers. There is no special past history, personal history and family genetic history. Post-hospital CT showed that the thyroid gland was enlarged, its density decreased unevenly, it was calcified, and nodular goiter was waiting to be discharged (Figure 2). 3D-Slicer software was used to reconstruct the two-dimensional image data of preoperative examination. It can be seen that the huge thyroid nodule on the right side is close to the level of the ipsilateral mandibular angle, down to the back of the chest, the lower edge of the aortic arch, and the deep posterior edge of the sternocleidomastoid muscle on both sides. The tracheal deflection is obvious, and the lumen is flattened to about 1/4th of the normal lumen (Figure 3). Through the 3D visualization model, we can clearly understand the actual size and growth direction of giant thyroid nodules, clearly grasp the three-dimensional anatomical relationship between tumors and organs and tissues such as trachea, superior laryngeal nerve, recurrent laryngeal nerve, carotid artery and vein, parathyroid gland, etc., and formulate accurate surgical paths and perform preoperative simulated surgery.
Figure 1: The neck of a typical patient with huge goiter is obviously swollen and inverted “pear-shaped” before operation. (Figure A is the right side view; B is the left side view).

Figure 3: Reconstruction of neck structure by preoperative 3D visualization technique. (Figure A shows the upper edge of a giant thyroid nodule reaching the level of the maxillary angle; Figure B shows a giant thyroid nodule compressing the trachea by >70% at its widest point; Figure C shows the lower edge of a giant thyroid nodule reaching the level of the lower edge of the aortic arch to the posterior sternum).
The patient underwent thyroidectomy on June 8, 2022. The bilateral recurrent laryngeal nerves were dissected in the whole process, and the parathyroid glands were preserved. The operation lasted for 200 minutes, and the bleeding was about 5ml. The tracheal compression was relieved, and the operation was successfully completed. 3D-Slicer was used to construct 3D model to locate neck tumor, and the accuracy of preoperative evaluation was verified by actual operation and postoperative measurement. The preoperative simulated operation path was highly consistent with the actual operation path, and the anatomical position of tumor and its adjacent organ tissue structure were consistent with the preoperative 3D visualization model. After bilateral total thyroidectomy, the actual size of the removed thyroid gland is about 10.6cm×4.2cm×3.8cm, which is equivalent to the preoperative model evaluation. 48 hours after operation, CT scan showed that the thyroid tumor was completely removed, and there was no damage to the surrounding blood vessels and no bleeding. After 3 months follow-up, there was no recurrence of CT.
Discussion
At present, surgery is still the most important treatment for giant goiter. Huge thyroid tumors are prone to serious postoperative complications such as large blood vessel injury, parathyroid gland injury, superior laryngeal and recurrent nerve injury, and postoperative tracheal collapse [8,9]. The tumor itself is easy to adhere to adjacent tissues and organs, which makes the operation more difficult, resulting in greater surgical damage to normal thyroid tissues [10]. Therefore, it is very necessary to accurately evaluate the situation of giant tumor before operation and make individualized operation plan. At present, the preoperative evaluation of goiter is mainly performed by thin-slice CT or MRI two-dimensional sectional anatomical images [11,12]. Therefore, pre-operative reconstruction of the 3D model of the neck by 3D visualization technology, combined with the three-dimensional anatomical relationship between the whole thyroid gland and the nodules, has unique advantages in evaluating the basic situation of giant thyroid nodules, choosing the surgical path and protecting the surrounding normal blood vessels, and helps to form a good surgical treatment strategy.
To evaluate the resection of giant goiter before operation, one is to evaluate the basic situation such as the type, size and growth direction of the tumor, the other is to look at the anatomical relationship between the tumor and peripheral blood vessels and nerves, and the trachea. At present, the two-dimensional preoperative evaluation of giant thyroid nodules is mainly based on CT, MRI and other imaging examinations. Fully understanding the anatomical relationship between giant thyroid nodules and surrounding tissues and organs is a necessary condition for the successful implementation of this operation. Senior surgeons rely on rich surgical experience and solid clinical skills to abstract the spatial conformation of giant thyroid nodules and realize preoperative evaluation, while junior doctors or inexperienced primary medical institutions give up surgical treatment because of the difficulty and high risk of operation.
In this study, 3D visualization technology is beneficial to more accurate preoperative evaluation and surgical path planning of giant goiter, which effectively avoids the damage of normal tissues and organs. The main advantages are as follows:
a) The three-dimensional model based on two-dimensional CT and MRI images can be rotated, enlarged and cut, which can visualize the relationship between giant nodules and surrounding tissues and organs more intuitively;
b) Giving different colors to different tissues, organs, nodules and blood vessels, and adjusting the transparency of thyroid gland, can show the giant nodules more clearly and integrally;
c) Surgeons can easily analyze the three-dimensional model without the assistance of imaging professionals, and the operation team can make a more stereoscopic and accurate judgment on the size, position and relationship with important tissues and organs of nodules, thus avoiding the influence of subjective judgment of clinicians on preoperative evaluation.
The latest research in the past mainly applied 3D visualization technology to preoperative planning of intracranial lesions and liver tumors [13-19],Through the 3D visualization technology, a 3D stereo model is constructed, and the size, specific location of the tumor and the anatomical relationship between the tumor and the surrounding adjacent tissues can be observed more intuitively [20,21], so that a fine surgical path can be formulated, which is similar to the content of this study. In all cases in this study, patients with giant goiter had varying degrees of tracheal compression, displacement, malformation, or luminal stenosis, which may make intraoperative anesthetic intubation difficult. Therefore, our research team used 3D visualization models to comprehensively assess the tracheal compression and stenosis in patients with giant goiter and took preoperative corrective treatment measures accordingly to effectively overcome these difficulties. In addition, many patients with giant goiter also have multiple enlarged lymph nodes in the neck, and the 3D visualization model allows a more intuitive observation of the number, location and fusion of the lymph nodes in the neck, which is of additional value for intraoperative guidance of lymph node dissection in the neck. The evaluation of peripancreatic lymph nodes by 3D visualization model will play a more important role.
However, there are still some shortcomings in the clinical application of 3D visualization technology for giant goiter:
a. Highly accurate 3D visualization model construction relies on high-quality CT or MRI scanning equipment, which requires imaging technologists to adjust the scanning parameters of the equipment and scan the 2D image images required for highquality model construction.
b. Current 3D visualization techniques only allow preoperative assessment of the morphological anatomy of giant thyroid nodules and cannot determine the nature of thyroid nodules.
c. Intraoperative protection of the superior laryngeal nerve and the recurrent laryngeal nerve from injury has been a challenge in thyroid surgery. The current 3D visualization technology needs to further increase the recognition of the nerve display to facilitate the surgeon’s accurate preoperative surgical path planning and avoid injury to the superior laryngeal nerve and the recurrent laryngeal nerve.
Conclusion
In summary, due to the relatively high surgical risk of giant thyroid nodule surgery, this study preoperatively performed 3D visualization reconstruction based on traditional 2D medical images in 8 patients undergoing giant thyroid nodule surgery to more intuitively understand the anatomical location relationship of giant thyroid nodules, to achieve accurate preoperative assessment, preoperative simulation of surgical path, and to make the actual surgical procedure more process-oriented and standardized. Therefore, it is more conducive to the successful completion of radical resection of giant goiter, while reducing unnecessary damage to normal tissues and organs and reducing surgical risks, which has very important surgical guidance and clinical application value for patients undergoing surgery for giant thyroid nodules.
Data Availability Statement
The original contribution presented in this study is included in the article/supplementary material and further details can be obtained by contacting the corresponding author.
Ethics Statement
The study was applied for and ethically approved by the ethical review committee of the First People’s Hospital of Anhui University of Technology (Huainan First People’s Hospital) (approval number: 2022-YJ-020-01), and all study subjects had an exemption from informed consent.
Author Contributions
All authors made significant contributions to the research process of this manuscript. Yisong Wang contributed to the writing of the manuscript, Hongzhen Zhang contributed to the conception and design of this study, Yongtian Li and Wenping Wang design of the study, Danqing Cheng and Dingfei Ren contributed to data collection and data collection, Feng Zhao contributed to data retrieval and manuscript review.
Funding
This research is supported by the doctoral program of Innovation Fund of Anhui University of Science and Technology (No. Postgraduate [2022] No.17), the key scientific research program of Anhui Education Department (No. KJ2019A0094), the key scientific research program of Anhui Education Department (No. KJ2019A0095) and the research program plan of Bengbu Medical College (No. BYKY2019318ZD).
Acknowledgement
This work was supported by the School of Medicine of Anhui University of Technology. The First People’s Hospital affiliated to Anhui University of Technology (Huainan First People’s Hospital) participated in the data collection.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Gardiner KR, Russell CF (1995) Thyroidectomy for large multinodular colloid goitre. Journal of the Royal College of Surgeons of Edinburgh 40(6): 367-370.
- Pradeep PV, Sattar V, Krishnachaithanya K, Ragavan M (2011) Huge thyromegaly: challenges in management. ANZ journal of surgery 81(5): 398-400.
- Harada K, Fujikawa T (2018) Giant adenomatous thyroid nodule compressing the trachea. Journal of general and family medicine 19(6): 219-220.
- Haugen BR, Alexander EK, Bible KC, et al. (2016) 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid : official journal of the American Thyroid Association 26(1): 1-133.
- Yin G, Zhang L, Dai T (2022) Application and Visualization of Human 3D Anatomy Teaching for Healthy People Based on a Hybrid Network Model. Journal of healthcare engineering 2022: 3702479.
- Wang ZH, Fu GM, Chen J, Chen YB, Tang Y (2017) [Application of computer aided design and 3D visualization technology in the operation of thyroid cancer with trachea invasion]. Zhonghua er bi yan hou tou jing wai ke za zhi = Chinese journal of otorhinolaryngology head and neck surgery 52(10): 774-776.
- Chen YB, Wang ZH, Fu GM, Wan QX, Li XJ, et al. (2020) Application of Computer-Aided Design (CAD) and Three-Dimensional (3D) Visualization Technologies in the Diagnosis and Treatment of Refractory Thyroid Tumors. Cancer management and research 12: 6887-6894.
- Sigdel B, Neupane B, Pokhrel A, Nepali P (2022) Giant multinodular goiter for 24 years; hidden in a village in Western Nepal. Clinical case reports 10(7): e6041.
- Le QV, Nguyen HV, Mai N, Nguyen HX Surgical treatment result of giant thyroid tumor: Case series in Vietnam. International journal of surgery case reports 54: 103-107.
- Said A, Konimba C, Ilias T (2022) Emergency management of a giant compressive goitre: a case report. The Pan African medical journal 41: 265.
- Yano T, Okada T, Sato H, Tomioka R, Tsukahara K, et al. (2021) Preoperative Evaluation of Substernal Goiter by Computed Tomography in the Extended Neck Position. Case reports in oncology 14(3): 1353-1358.
- Wang X, Zhou, Li YC (2020) Surgery for retrosternal goiter: cervical approach. Gland surgery 9(2): 392-400.
- Fang CH, Zhang P, Zhou WP (2020) Efficacy of three-dimensional visualization technology in the precision diagnosis and treatment for primary liver cancer: a retrospective multicenter study of 1 665 cases in China]. Zhonghua wai ke za zhi. Chinese journal of surgery 58(5): 375-382.
- Jian ZH, Li JY, Wu KH (2022) Surgical Effects of Resecting Skull Base Tumors Using Pre-Operative Multimodal Image Fusion Technology: A Retrospective Study. Frontiers in neurology 13: 895638.
- Noro S, Seo Y, Honjo K (2022) Visualization and Maneuverability Features of a Robotic Arm Three-Dimensional Exoscope and Operating Microscope for Clipping an Unruptured Intracranial Aneurysm: Video Comparison and Technical Evaluation. Operative neurosurgery (Hagerstown, Md) 22(1): 101-105.
- Westermaier T, Linsenmann T, Homola GA (2016) 3D rotational fluoroscopy for intraoperative clip control in patients with intracranial aneurysms--assessment of feasibility and image quality. BMC medical imaging 16(30).
- Chinese S, Liver C, Clinical P, Digital I (2020) [Clinical practice guidelines for precision diagnosis and treatment of complex liver tumor guided by three-dimensional visualization technology (version 2019)]. Nan fang yi ke da xue xue bao = Journal of Southern Medical University 40(3): 297-307.
- Fang C, An J, Bruno A (2020) Consensus recommendations of three-dimensional visualization for diagnosis and management of liver diseases. Hepatology international 14(4): 437-453.
- Liao R, Liu L, Song B, Wan X , Wang S, et al. (2022) 3D-Slicer Software-Assisted Neuroendoscopic Surgery in the Treatment of Hypertensive Cerebral Hemorrhage. Computational and mathematical methods in medicine 2022: 7156598.
- Ruusuvuori P, Valkonen M, Kartasalo K (2022) Spatial analysis of histology in 3D: quantification and visualization of organ and tumor level tissue environment. Heliyon 8(1): e08762.
- Liimatainen K, Latonen L, Valkonen M, Kartasalo K, Ruusuvuori P, el al. (2021) Virtual reality for 3D histology: multi-scale visualization of organs with interactive feature exploration. BMC cancer 21(1): 1133.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





