Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
A Rare Localization of HIV-Associated Adenoid Cystic Carcinoma: Clinical Case Volume 4 - Issue 4
Mame Sanou Diouf1, Moustapha Ndiaye2*, Amadou Thiam1, Hussein Ghezael1, Khadim Diouf1, Richard EA Deguenonvo1, Abdou Sy3, Malick Ndiaye3 and Raymond Diouf1
- 1Cheikh Anta Diop University, Grand Yoff Hospital Center, Dakar, Senegal
- 2Hospital intern, Senegal
- 3Diamniadio Children’s Hospital, Dakar, Senegal
Received: January 30, 2020; Published: February 18, 2020
Corresponding author: Moustapha Ndiaye, Hospital intern, Senegal
DOI: 10.32474/SCSOAJ.2020.04.000191
Abstract
Adenoid cystic carcinoma (ACC) represent less than 1% of carcinomas of the head and neck. Sublingual localization is a very rare case behind localizations in the accessory, submandibular and parotid salivary glands. This is a case of sublingual gland ACC associated with HIV2 infection in a 52-year-old female patient. The diagnosis was made after anatomopathological examination of a biopsy specimen and confirmed by the histological study of the operative specimen; it was cystic adenoid carcinoma cribriform type. The treatment started was the exclusive surgery. There was no recurrence after 6 months of follow-up.
Keywords: Adenoid cystic carcinoma, Sublingual gland, HIV
Introduction
Adenoid cystic carcinoma (ACC) represent slowly growing and potentially aggressive malignant lesions. They are characterized by their peri-neural extension justifying their tendency to recidivism. ACC account for less than 1% of head and neck carcinomas. Their sublingual location is a very rare case, behind the locations at the minor salivary glands, submandibular and parotid [1]. We report by drawing from the literature review, the case of a ACC of the sublingual gland associated with HIV2 infection which was revealed by a painful mass of the floor of the mouth. Local control was obtained after a surgical procedure without additional radiotherapy.
Case
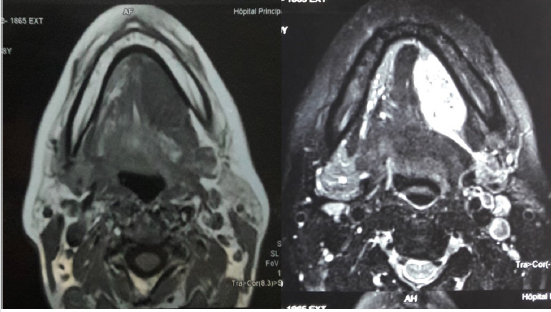
This case is about a 52-year-old female patient who had a painful mass of the oral floor that gradually increased in volume and has been evolving for about 13 months. The examination found a hard, sensitive mass of the left anterolateral floor measuring about 4cm in length and covered with a healthy-looking mucosa (Figure 1). The cervical lymph node areas were free. The rest of the examination was without particularity. The MRI had objectified a T2 hyposignal tissue process enhanced after contrast injection, measuring 42 x 21mm, developed from the left anterolateral floor and did not extend beyond the median line. The tumour came into contact with the mandible without invading it (Figure 2).
Figure 2: Tissue process of the left anterolateral floor with contrast enhanced MRI.
A(left): tissue process of the left anterolateral floor; B(right): contrast enhanced MRI.
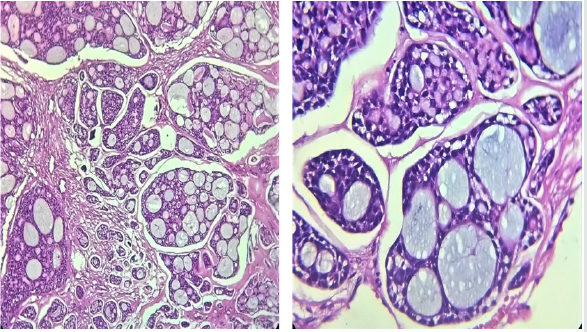
A mass biopsy was performed, and histological examination revealed adenoid cystic carcinoma of the sublingual gland. The retroviral serology performed as part of the preoperative assessment was positive (HIV2). The extension assessment was negative, and the tumour was classified T3 N0 Mx. The surgical treatment consisted of a complete excision of the enlarged mass to the adjacent muscles; a left triangular neck dissection had also been performed. A nasogastric tube was put in place at the end of the procedure. We had not noted any postoperative complications and the nasogastric tube removed at Day 17 postoperatively. Our patient had not received adjuvant radiotherapy because of her particular terrain (HIV2) and because of the healthy resection margins. The histological study of the operative specimen confirmed the initial diagnosis of adenoid cystic carcinoma which was cribriform type (Figure 3). After a 6 months follow-up there was no recurrence. Management of HIV infection had been undertaken in the Internal Medicine Department.
Discussion
Epidemiological aspects
Adenoid cystic carcinomas represent 27.9% of the overall incidence of salivary gland cancers [2]. This rate also corresponds to less than 1% of all head and neck carcinomas. Sublingual localization is rare; the main site of localization is the accessory salivary glands (30%), the submandibular gland (15 to 30%) followed by the parotid gland (2 to 15%) [1]. Female predominance is clear with a median age of 59 years and a peak incidence between 50-60 years [3-5]. That was the case with our patient.
Clinical-radiological aspects
The most common clinical presentation is a mass of slow growth associated with pain attributed to its tendency to perineal invasion [2]. Nodal involvement is rare; it varies between 6 and 10% if we consider all possible locations (glandular and extraglandular) [5]. The MRI examination is the examination of choice, it allows to give the limits of the lesion and to look for a perineal invasion. Panoramic dental radiography and CT are useful for searching for bone extension [1,2].
Histological aspects
ACC are asymmetric tumours with various lobules. There are 3 histological types that can be classified into 2 grades: low grade (tubular and cribriform type) and high grade (solid type). In our case, the ACC was low grade. The main character of ACC is nervous invasion. It would seem that perinervous invasion, unlike intra nervous invasion, has no influence on survival [1,5].
Therapeutic aspects
Surgery is indicated when possible and must respect the margins of resection. There are no data supporting the systematic use of radiotherapy [6].
Prognostic factors
Several factors influence the prognosis of ACC; the following are
poor prognostic factors [1,5].
a. lymph node involvement
b. high-grade tumours
c. the nervous invasion
d. invaded resection margins
In our patient, the tumour was low-grade without node
extension. The MRI did not show any nerve invasion and the
resection margins were healthy. This is a case of good prognosis.
The relationship between HIV and cystic adenoid carcinoma
HIV infection is known to cause salivary glandular dysfunctions: lymphoepithelial cysts, non-Hodgkin’s lymphoma, Kaposi’s sarcoma. HIV-associated salivary glandular hypertrophy in adult patients living with HIV is estimated at 5% [7,8]. The parotid gland is the major salivary gland most affected by HIV-associated tumour pathology [7-9]; the sublingual gland is exceptionally affected. Since the ACC of the sublingual gland is extremely rare [1], HIV association is even more so and has not been found in the literature. On this basis, the relationship between HIV and cystic adenoid carcinoma of the sublingual gland remains a mystery and leaves us with no answer to the following questions: would HIV infection promote the occurrence of ACC in the sublingual gland? Would it change the tumour evolution? Does it influence the prognosis of the disease?
Conclusion
We have just reported a rare location of an adenoid cystic carcinoma of the salivary glands. This was a case of good prognosis whose surgery was sufficient to obtain local control. Association with HIV infection has not been reported as a risk factor; nor has it been a therapeutic failure despite being an obstacle to radiotherapy. However, the patient must be re-evaluated regularly so as not to ignore a recurrence that is characteristic of the adenoid cystic carcinoma.
Financial Disclosure
None.
Conflict of Interest
None.
Authors Contributions
Mame Sanou Diouf proposed the publication of the case and made his corrections to the manuscript, Moustapha Ndiaye wrote the manuscript. All the other authors made additional corrections.
References
- Song JY (2016) Adenoid cystic carcinoma of the sublingual gland: A case report. Imaging Science in Dentistry 46(4): 291-296.
- Coca-Pelaz A, Rodrigo JP, Bradley PJ (2015) Adenoid cystic carcinoma of the head and neck - An update. Oral Oncology 51(7): 652-661.
- Dubergé T, Bénézery K, Resbeut M (2012) Carcinomes adénoïdes kystiques ORL: étude rétrospective multicentrique de 169 cas. Cancer/Radiothérapie 16: 247-256.
- Kokemueller H, Eckardt A, Brachvogel P (2004) Adenoid cystic carcinoma of the head and neck--a 20 years’ experience. Int J Oral Maxillofacial Surg 33(1): 25-31.
- Meyers M, Granger B, Herman P (2016) Les carcinomes adénoïdes kystiques ORL : une étude multicentrique prospective REFCOR de 95 cas. Annales françaises d’oto-rhino-laryngologie et de pathologie cervico-faciale 133: 11-16.
- Mourad WF, Hu KS, Shourbaji RA, Harrison LB (2013) Management of sarcomatoid salivary duct carcinoma of the submandibular gland duct with coexisting seropositive human immunodeficiency virus. The Journal of Laryngology & Otology 127(6): 621-624.
- Brette MD, Ben Bahmed R, Monteil JP (2007) Manifestations oto-rhino-laryngologiques et séropositivité au virus de l’immunodéficience humaine. Encyclopédie Médico-Chirurgicale.
- Goldman Nelson, Shuja S, Makary R (2013) Mucoepidermoid carcinoma presenting as a large cyst of the parotid gland in HIV disease. Ear, Nose & Throat Journal 92(7): 310-311.
- Jeffers L, Webster-Cyriaque JY (2011) Viruses and Salivary Gland Disease (SGD): Lessons from HIV SGD. Adv Dent Res 23(1): 79-83.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...