Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2643-6760
Case Report(ISSN: 2643-6760) 
A Rare Case of Penile Fournier’s Gangrene in A Young Healthy Patient Volume 6 - Issue 1
Almeida M1*, Capitão M2, Tawadros T3 and Pellet L4
- 1Department of General Surgery, Hospital RivieraChablais, VaudValais, Switzerland
- 2Department of Internal Medicine, Hospital Geral de Santo António, Portugal
- 3Department of Urology, Hospital RivieraChablais, VaudValais, Switzerland
- 4Department of Plastic Surgery, Hospital RivieraChablais, VaudValais, Switzerland
Received: September 18, 2020; Published: October 05, 2020
Corresponding author:Almeida M, Department of General Surgery, Hospital RivieraChablais, VaudValais Avenue de Belmont 25 1820 Montreux, Switzerland
DOI: 10.32474/SCSOAJ.2020.06.000226
Abstract
Fournier’s gangrene refers to a rare perineal infection with fulminant evolution towards multiorgan failure if no surgical treatment is quickly instaured. It mainly affects immunocompromised patients. Very few cases of Fournier’s gangrene circumscribed to the penis in young healthy patients were published to date. We treated a rare case of a penile Fournier’s gangrene in a young healthy man.
Case Presentation
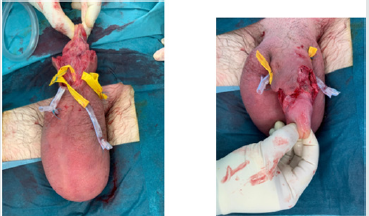
Figure 1: Patient’s penis at presentation. Note the ongoing necrosis at the tip penile foreskin. Pulling back foreskin was impossible at this time due to excruciating pain.

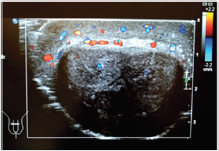
Figure 2: Penile ultrasound at arrival. Important oedema of the soft tissue sparing muscular tissues. Good permeability of vascular structures reported by the radiologist.
A 32-year-old healthy man was brought to hospital who
consulted for a swollen and highly painful penis that started two hours earlier. Upon anamnestic investigation, patient described a
vesicular penian lesion a week before, following a single episode
of non-protected sexual intercourse. On physical examination, his
penis was abnormally erythematous and uniformly oedematiated,
measuring approximately 18 cm in extension and 5 cm in diameter
(Figure 1). Manipulations were impossible due to extreme pain.
Fever, hypotension, and tachycardia were also present.Biochemical
and hematological laboratory findings were consistent with an
infectious state while urinalysis was not possible because patient
could not urinate. Pain was refractory to opioid medication in high
doses. An urgent penile US showed important subcutaneous signs
of infection with sparing of muscular tissues (Figure 2).
We decided to complement with anabdominal-pelvic CT scan
that did not reveal any abdominoperineal abnormalities.Immediate
empiric broad spectrum antibiotic therapy (Piperacillin-Tazobactam
4.5g qid I.V. + Clindamycin 900 mg tid I.V.) was instaured after two
swab skin tests and blood cultures. Emergent surgical debridement
took place as well as suprapubic catheterization. At day 1, a second
surgery was performed because of ongoing penile cutaneous
necrosis (Figures 3&4). The patient remained in intensive unit care
for 3 days for hemodynamic surveillance and hypoxemia. Wound care
took place every day, with a protocol of water mixed Chlorexidine
(©Hibidil) disinfection followed by generous application of
hyaluronate plus silver sulfadiazine (Ialugen plus©) covered with
a paraffin gauze dressing. A multisensible Streptoccus Pyogenes
was isolated from one of the swabs and debrided skin while blood
cultures where negative. Histo-pathological examination confirmed
a Fournier gangrene. Large spectrum probabilistic antibiotherapy
was replaced by Amoxicilline-Clavulate 1g bid PO for a total of 10
days. By day 15 (Figure 5), patient left the hospital and the same
wound care protocol was continued with every-day outpatient
consultations. By day 30, patient was submitted to a plastic
reconstructive procedure (Figure 6). Suprapubic catheterization
was withdrawn by day 36.
Figure 3:Aspect of the penis several hours after first debridement (day zero). Ongoing necrosis at the cutaneous tip of the penis.

Figure 5: Aspect of the penis day 15 after debridement, dorsal view on the left, ventral view on the right. Note at least 1 cm sparing of ventral penile skin. Suprapubic catheter in place.

Figure 6: Aspect of penis by day 34 after first debridement, day 4 after plastic reconstruction with scrotal advancement flap. Suprapubic catheter still in place.

Discussion
Fournier’s gangrene is a rare and rapid-evaluating soft tissue infection that requires urgent diagnosis and treatment with broad spectrum antibiotics and surgical debridement[1]. In the majority of cases, patients need several debridement’s in the first days after diagnosis[2]. Patient history needs to be considered. Mortality rates still approach 20 % nowadays[3].To our knowledge, this is one of the few reports of penile limited Fournier’s gangrene in a healthy young patient. The decision to surgical intervention cannot be postponed if diagnosis is in doubt. Other differential diagnosis as penile fracture, paraphimosis or dorsal vein thrombosis may be evoked but must be promptly excluded by appropriate anamnesis, septic status and appropriate imaging tests as any delay might imply hazardous consequences. Patient’s history is of paramount importance and cannot be overemphasized.
References
- Thwaini A (2006) Fournier's gangrene and its emergency management. Postgrad Med J 82(970): 516-519.
- Eke N (2000) Fournier's gangrene: a review of 1726 cases. Br J Surg 87(6): 718-728.
- Hahn HM (2018) Analysis of prognostic factors affecting poor outcomes in 41 cases of Fournier gangrene. Ann Surg Treat Res 95(6): 324-332.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...